Active Bleeding after Valve Surgery under Extracorporeal Circulation: Incidence and Risk Factors? Prospective Observational Study on 59 Patients in a West African Country
Elhadji Boubacar BA1*, Diagne PA1, SARA C2, Gaye I1, BA PO1, Traoré MM1, Camara Mory2, Lèye PA, Mbengue AA2, Camara L2, Touré M2, Laye C2 and Kane O1
1Faculty of Medicine of the Cheikh Anta Diop University, Senegal
2National University Hospital of FANN, Senegal
Submission: November 04, 2022; Published: December 07, 2022
*Corresponding author: Elhadji Boubacar BA, Faculty of Medicine of the Cheikh Anta Diop University, Senegal
How to cite this article: Elhadji Boubacar BA, Diagne PA, SARA C, Gaye I, BA PO, et al . Active Bleeding after Valve Surgery under Extracorporeal Circulation: Incidence and Risk Factors? Prospective Observational Study on 59 Patients in a West African Country. J Cardiol & Cardiovasc Ther. 2022; 17(5): 555975. DOI: 10.19080/JOCCT.2022.17.555975
Abstract
Introduction: Active bleeding after cardiac surgery is defined as blood loss > 1.5 ml / kg / h for 6 consecutive hours within the first 24 hours or in case of re-operation for haemostasis within the first 12 hours postoperatively.
The aim of our work was to assess the incidence and risk factors for the occurrence of active bleeding in postoperative valve surgery with extracorporeal circulation.
Patients and methods: Prospective observational study, conducted over 5 months at the Dakar cardiac Centre. All patients who underwent valve surgery under extracorporeal circulation were included. Exclusion criteria were: death in the operating room or during the first 6 hours, incomplete medical records.
Results: Our work included 59 patients, with a predominance of females (sex ratio = 0.6) and a mean age of 31 years. All patients underwent scheduled surgery, and none of them were in acute cardiac decompensation. Only 25.4% of the patients were on LMWH, which was stopped 24 hours before the operation . Preoperatively, 11.8% of patients had moderate anemia, 3.4% had mild thrombocytopenia, 30.5% had low prothrombin levels (40-70%), 5.1% had an impaired left ventricular ejection fraction, 8.5% had moderate right ventricular systolic dysfunction, and more than half (54.2%) had severe pulmonary arterial hypertension (PAH). Intraoperatively: Intravenous induction was predominant (79.6%), all patients received tranexamic acid, priming of the extracorporeal circulation (ECC) was done with crystalloids alone in 83% of cases, the mean duration of the ECC was 140 min, sympathomimetics were used in 72.3% of patients and transfusion was performed in 45.7% of patients. The incidence of active bleeding in the ICU was 52.5% with the main risk factors being low age, low BMI, preoperative anticoagulant treatment, long bypass surgery and low prothrombin level.
Conclusion: Active bleeding is a serious complication in cardiac surgery and may be responsible for an increase in perioperative morbidity and mortality
Keywords: Active bleeding; Valve surgery; Incidence
Abbreviations: ECC: Extracorporeal Circulation; LVEF: Left Ventricular Ejection Fraction; TAPSE: Tricuspid Annular Plane Systolic Excursion; MVR: Mitral Valve Replacement; TP : Tricuspid Plasty; MP : Mitral Plasty; TVR : Tricuspid Valve Replacement; AVR : Aortic Valve Replacement; PAH: Pulmonary Arterial Hypertension; LMWH : Low Molecular Weight Heparin; SPAP: Systolic Pulmonary Arterial Pressure
Introduction
Active bleeding after cardiac surgery is defined as blood loss > 1.5 ml/kg/hr for 6 consecutive hours in the first 24 hours or in case of re-operation for haemostasis in the first 12 hours postoperatively [1]. This is a major and serious complication feared by the resuscitating anesthetist and surgeons, which may be responsible for anemia and transfusion, leading to an increase in peri-operative morbidity and mortality [2,3]. The aim of our study was to evaluate the incidence and risk factors for the occurrence of active bleeding after valve surgery under extracorporeal circulation (ECC).
Patients and Methods
This was an observational, prospective, descriptive and analytical study of patients operated on for valve surgery in the cardiac department of the Fann University Hospital in Dakar over a 5-month period from 12/10/2021 to 08/03/2022.
All patients scheduled for valve surgery under ECC were included in the study.
Exclusion criteria were: patients who died intraoperatively or during the first 6 hours, patients with incomplete or unusable records. All patients included in the study had a cardiology consultation with systematic electrocardiogram and transthoracic cardiac ultrasound. They also had a cardiac surgery consultation before being sent for the pre-an aesthetic consultation. After confirmation of suitability for anesthesia, patients were included in the surgical programme.
Upon arrival in the operating room, patients were routinely monitored with an electrocardioscope, non-invasive blood pressure and peripheral oxygen saturation. In addition to this standard monitoring, patients were routinely fitted with a central venous line and an arterial catheter. These were used to measure central venous pressure and invasive arterial pressure respectively. A trans-oesophageal ultrasound was systematically performed intraoperatively either by a cardiologist or by the anesthetist. A blood-sparing strategy was systematically carried out with the administration of tranexamic acid. Antibiotic prophylaxis was also administered to all patients. At the end of the operation, all patients were systematically transferred to the intensive care unit.
The software used for the descriptive and analytical statistical analysis of the data and for the production of the figures are the following: Epi Info, SPSS, Stata, Excel table.
Descriptive Results
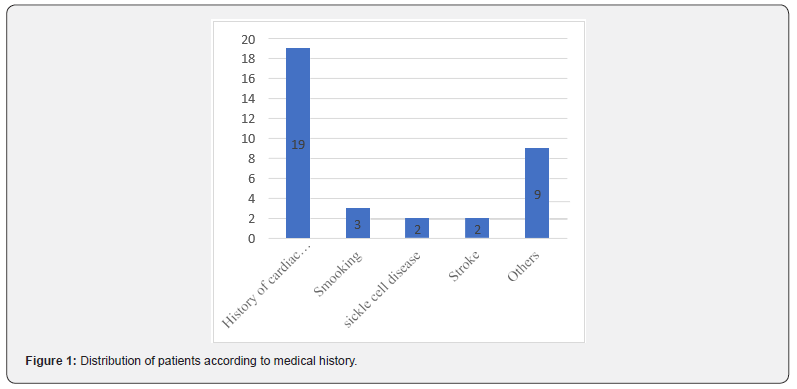
Our study included 59 patients with a predominance of women, i.e. a sex ratio of 0.6. The average age was 31 years with extremes of 08 and 76 years. Determination of the body mass index (BMI) before the operation revealed that 5.1% of patients were overweight and 37.3% were thin. No previous history or comorbidities were noted in 45.7% of patients. Hospitalization for acute cardiac decompensation was reported in 19 patients (32%), including 03 episodes in 07 patients, 02 episodes in 03 patients, 01 episode in 09 patients. The most common cause was hypertension (6.7%), followed by smoking with 5% of cases (See Figure 1).
Previous cardiac surgery was noted in 03 patients including 02 cases of mitral valve replacement (MVR) and 01 case of mitral plasty (MP). Only 25.4% of the patients were on anticoagulant therapy with low molecular weight heparin (LMWH), which was stopped 24 hours prior to surgery. Preoperatively, there were 11.8% cases of moderate anemia with hemoglobin (Hb) between 8-10g/dL, 3.4% mild thrombocytopenia (130,000-150,000/ mm3), 30.5% low prothrombin levels (40-70%), impaired left ventricular ejection fraction (LVEF) in 5.1% of patients (LVEF between 33-50%), moderate right ventricular systolic dysfunction in 8.5% of cases with a TAPSE between 11-15 mm, severe pulmonary arterial hypertension (SPAP > 50mmHg) in more than half of our population (54.2%).
Intraoperative phase:
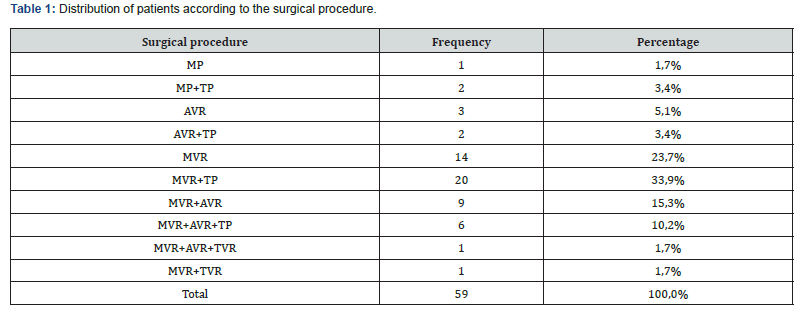
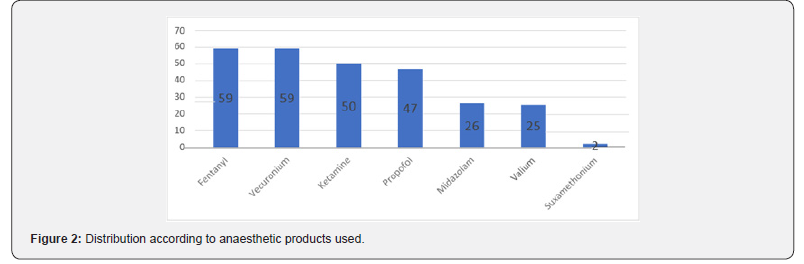
The most common procedure was mitral valve replacement (MVR) combined with tricuspid plasty (TP) with a rate of 33.9%, followed by isolated MVR with 23.7% (see procedure distribution in Table 1). All patients received general anesthesia with orotracheal intubation. Intravenous induction was predominant with 79.6% compared to 20.4% for the inhalation route (see Figure 2). All patients received tranexamic acid intraoperatively either in 3 boluses of 15mg/kg (91.5%) or continuously at 10mg/kg/hour after a bolus of 10mg/kg (8.4%). Regarding extracorporeal circulation, priming was carried out in 83% of cases with crystalloids alone and in 20% with a combination of crystalloids and colloids, the average duration of the ECC was 140 min [61-372 min]. Hemodynamically, norepinephrine was used in 43 patients (72.8%), dobutamine in 10 patients (16.9%) and milrinone in 23 patients (38.9%). Twenty-seven of our patients (45.7%) were transfused intraoperatively (see Figure 3). All our patients received protamine sulphate after the cessation of the ECC in order to antagonize the effect of heparin (protamine dose = cumulative heparin dose).

Post-operative phase:
The biological assessment carried out at at the first hour of admission to the intensive care unit revealed: anaemia with an Hb level < 10g/dl in 42.4% of cases, 37.3% thrombocytopenia (platelet level < 150,000/mm3), a drop in the prothrombin level (<70%) in 61% of cases The cardiac echodoppler in the immediate postoperative period revealed: severe alteration of the systolic function of the left ventricle (LVEF < 40%) in 16.9% of cases; systolic dysfunction of the right ventricle (TAPSE < 10 mm) in 40.7%, severe PAH in 6 patients (SPAP > 50mmhg), i.e. 10.2%. Fifteen patients received tranexamic acid immediately postoperatively, i.e. 24.4%. Transfusion of labile blood products was performed in 25 patients, i.e. 42.3%.
Active bleeding was observed in 31 patients, i.e. an incidence of 52.5% with bleeding over the first six hours > 1.5ml/kg/h. Of these patients, 03 were taken back to the operating room for haemostasis.
The outcome was favorable in 89.8% of patients despite active bleeding postoperatively. The overall mortality was 10.1% or 6 patients, distributed as follows:
i. Two of our deaths (3.38%) were directly related to the severe acute bleeding syndrome; Two of our patients died at day 4 and day 5 following sepsis from nosocomial pneumonia;
ii. One of the patients developed a stroke followed by sepsis from nosocomial pneumonia and died at day 8; One death at day 5 was related to acute kidney injury;
iii. None of the patients who required revision surgery died.
Analytical Results: Statistical Correlations
Epidemiological data
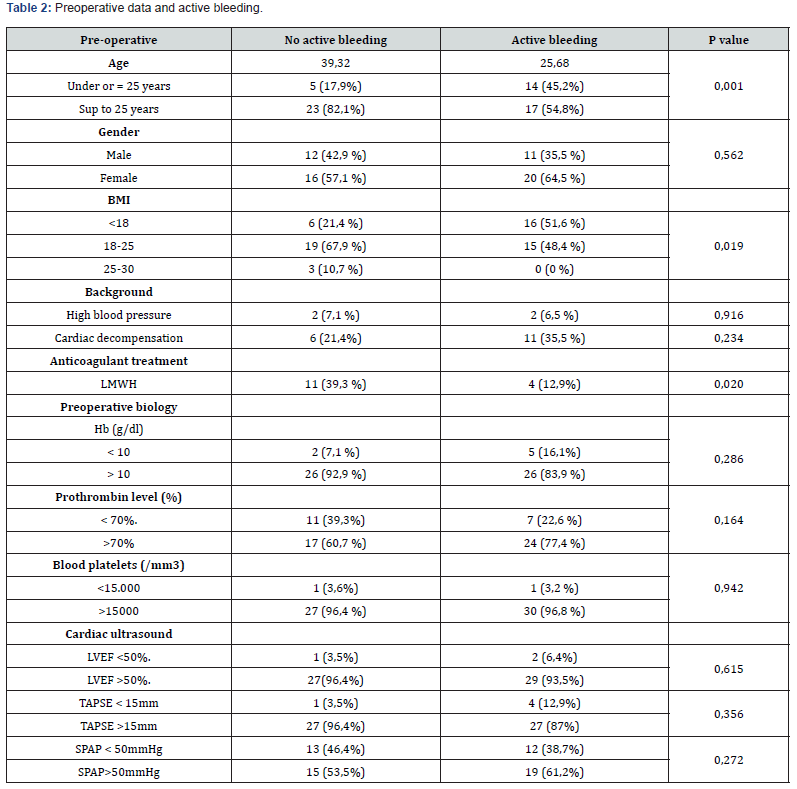
Patients who experienced an active bleed had a mean age of 25.68 years compared to 39.32 years for those who did not experience an active bleed (p = 0.001), suggesting that a younger age may be a risk factor for the occurrence of an active bleed.
Patients with a low BMI (<18 kg/m2) had a 3.9-fold greater risk of active bleeding than patients with a BMI greater than 18 kg/m2 (Odds Ratio = 3.906; p=0.019).
Patients who were on LMWH also had a 4.4 times greater risk of active bleeding than patients who were not on anticoagulation (Odds Ratio = 4.367; p=0.02).
Differences in other parameters such as gender, history, biology or preoperative treatment were not significant (see Table 2).
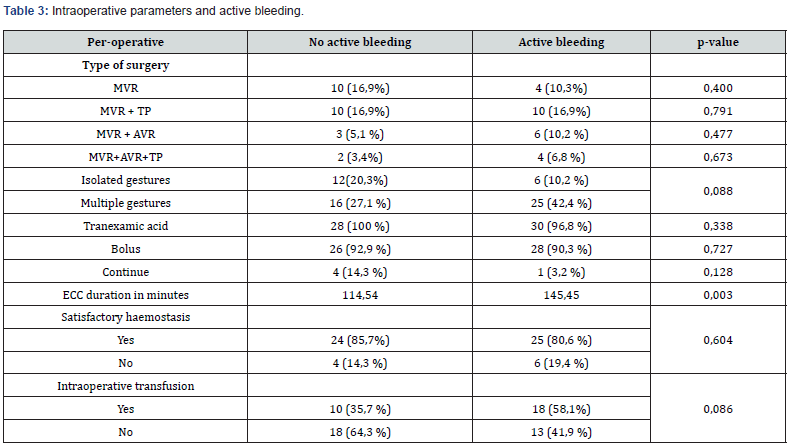
Intraoperative data
Of the parameters studied intraoperatively (see Table 3) to detect a risk factor for active bleeding intraoperatively, the duration of the bypass surgery was the only determining parameter. Patients with a ECC duration of more than 130min had a higher risk of active bleeding with an odds ratio of 3.88.
Post-operative data
Among the postoperative parameters (see Table 4), only a low prothrombin count seemed to have an impact on the occurrence of active bleeding with a p=0.029.
Discussion
In our study, the mean age of the patients operated on was 31 years with extremes of 8 and 76 years. The median age was 30 years. Moreover, in most series from poor countries, a similar average age is reported, with a more frequent occurrence in school-age subjects [4,5]. In contrast to the low age found in our work as a determining factor, it is the advanced age > 60- 70 years that has been cited in the literature [6,7]. Patients with a low BMI <18 kg/m2 had a 3.9-fold higher risk of active bleeding than patients with a BMI >18 kg/m2 (Odds Ratio = 3.906; p=0.019). Our results are consistent with some studies that clearly show that the higher the BMI, the lower the risk of bleeding or repeat surgery for haemostasis in post cardiac surgery [6-8]. The female predominance in our series has been observed in other studies and is very common in mitral stenosis [5,9]. Although in our study there was a statistically significant relationship between anticoagulant therapy and the risk of active postoperative bleeding, our sample of patients on LMWH was small (CI 1.196-15.951) and few studies have established a clear causal relationship because there is a lack of robust scientific data. Although PAH has been shown to increase operative risk in some series [10,11], we did not find a correlation between PAH and the occurrence of active bleeding postoperatively.
To limit the risk of acute bleeding, tranexamic acid was used intraoperatively in all our patients. This product has antifibrinolytic effects, which have been widely demonstrated to reduce postoperative bleeding. This product has anti-fibrinolytic effects, the effectiveness of which has been widely demonstrated on the reduction of postoperative bleeding, the rate of transfusion and re-intervention for haemorrhage [12]. A long duration of bypass surgery was found in our work to be a determining factor in the occurrence of active bleeding. This is consistent with the literature [7,13,14]. Moreover, Stalis et al. [13] have shown an increase in the time spent on bypass surgery to be an independent factor in repeat surgery for bleeding, and Despotis et al. [14] have shown that there is a 25% increase in the risk of transfusion for cardiac surgery lasting more than 145 minutes.
In our study, thirty-one of our patients had active bleeding postoperatively, i.e. 52.5%, which is a very high bleeding rate compared to other studies of bleeding in cardiac surgery, where the incidences range from 1 to 15% [15,16]. However, only three of our patients (5.1%) required revision surgery. This incidence of revision surgery is similar to the study by Tirilomis et al. [17], where re-explorations after cardiac surgery in adults were 4.8%. It is also in general agreement with the results of the literature which found a rate of re-exploration of around 3% [15,18]. We have identified low prothrombin levels as a factor independently associated with postoperative bleeding. However, although widely studied in the literature [7,19], there has been no evidence of an association between postoperative prothrombin count.
and postoperative bleeding in cardiac surgery. All our patients who presented with active bleeding received transfusion of packed red blood cells and fresh frozen plasma in a 1:1 or 1:2 ratio based on the patient’s hemoglobin level, platelet count, clinical status and hemodynamic status. The acceptable hemoglobin level after cardiac surgery is uncertain. A level of 7 g/dl is sufficient to cover oxygen requirements, perhaps even less in the healthy individual, and this level appears to be transferable to the critical clinical situation [20,21]. Overcompensation is detrimental as haematocrit levels above 34% at ICU entry after cardiac surgery are associated with excess mortality and increased morbidity after coronary bypass surgery [22]. In addition, the criteria for transfusion are better defined on the basis of decision algorithms [23] that integrate coagulation tests and, in particular, delocalised tests. The latter make it possible to mechanically reduce the volume of transfusion [14,24,25].
The overall death rate in our study was 10.1%, i.e. 6 patients, of which two deaths (3.38%) were directly related to active bleeding. The mortality reported in the series varies considerably according to geographical location. In underdeveloped countries, rates between 1 and 7.8% have been reported [26-28].
Limitations of the study
There is no consensus definition of early postoperative bleeding in cardiac surgery. As the universal definition of perioperative bleeding [30] lacks precision in characterizing postoperative bleeding, we based ourselves on the definition proposed by a French team [1]. This study is one of the few to evaluate postoperative bleeding based on the quantity of blood drained by the redons or the need for revision surgery for hemostasis. It was therefore difficult to compare all our results with those in the literature. Due to the small sample size, the sample size was not representative enough.
Fibrinogenemia and the use of fibrinogen were not studied in our work, due to its cost and availability. This element would have been interesting to analyze, because the literature has shown that a low level (<2.5g/l) both preoperatively and postoperatively would have an important influence on postoperative bleeding. And it would be a protective factor for bleeding and reoperation for haemostasis, without having any influence on the transfusion rate when it becomes higher than 3.6g/l. Some studies recommend systematic preoperative supplementation with fibrinogen, particularly if the level is less than 1.5 g/l, as recommended by the Formalized Recommendations of Experts [31].
Conclusion
Valve pathologies are an important part of cardiovascular disease in Africa. With the advent of cardiac surgery and extracorporeal circulation in Senegal, a major step forward has been made, allowing early and appropriate on-site management. However, this surgery is fraught with complications during and after the operation. These include active bleeding, which is a complication much feared by anesthetists and surgeons, as it may be responsible for re-operation, anemia and transfusion of labile blood products, all of which are factors that increase morbidity and mortality.
References
- Colson PH, Gaudard P, Fellahi JL, Bertet H, Faucanie M, et al. (2016) Active Bleeding after Cardiac Surgery: A Prospective Observational Multicenter Study. PloSOne 11(9): e0162396.
- Ferraris VA, Ferraris SP, Saha SP, Hessel EA, Haan CK, et al. (2007) Perioperative Blood Transfusion and Blood Conservation in Cardiac Surgery: The Society of Thoracic Surgeons and The Society of Cardiovascular Anesthesiologists Clinical Practice Guideline. Ann Thorac Surg 83(5): S2786.
- Murphy GJ, Reeves BC, Rogers CA, Rizvi SIA, Culliford L, et al. (2007) Increased Mortality, Postoperative Morbidity, and Cost After Red Blood Cell Transfusion in Patients Having Cardiac Surgery. Circulation 116(22): 254452.
- Essop MR, Nkomo VT (2005) Rheumatic and non-rheumatic Heart disease, Epidemiology, Management, and Prevention in Africa. Circulation 112(23): 3584-3591.
- Samiei N, hakimi MR, Yalda M, Peighambari MM, Saeid H, et al. (2014) Surgical outcomes of heart valve replacement: A study of tertiary specialized cardiac center. Arya Atheroscler 10(5): 233-237.
- Karkouti K, O'Farell R (2006) Prediction of massive blood transfusion in cardiac surgery. Can J Anaesth 53(8): 781̼94.
- Lopes CT, dos Santos TR (2015) Excessive bleeding predictors after cardiac surgery in adults: integrative review. J Clin Nurs 24(21-22): 304662.
- Rahmanian PB, Adams DH (2007) Impact of Body Mass Index on Early Outcome and LateSurvival in Patients Undergoing Coronary Artery Bypass Grafting or Valve Surgery or Both. Am J Cardiol 100(11):17028.
- Yayehd K, Kouleke D, Tchamdja T, Tcherou T, Pessinaba S, et al. (2012) Rheumatic valve disease in Lomé: epidemiological aspects and management. J Rech Sci Univ 2(7): 51-58.
- Antunes MJ (2016) Pulmonary hypertension in valve disease: A beast of the past. Journal of Thoracic Cardiovascular Surgery 151(2): 1300-1301.
- Cannesson M, Bastien O, Lehot JJ (2005) Particularities of hemodynamic management after cardiac surgery. Réanimation 14(9): 216-224.
- Wang G, Xie G, Jiang T, Wang Y, Wang W, et al. (2012) Tranexamic acid reduces blood loss after off-pump coronary surgery: a prospective, randomized, double-blind, placebo-controlled study. Anesth Analg 115(2): 239-243.
- Salis S, Mazzanti VV, Merli G, Salvi L, Tedesco CC, et al. (2008) Cardiopulmonary Bypass Duration Is an Independent Predictor of Morbidity and Mortality After Cardiac Surgery. J Cardiothorac Vasc Anesth 22(6): 81422.
- Despotis Gj, Joist JH, Hogue CW, Alsoufiev A, Maier DJ, et al. (1996) More effective suppression of hemostatic system activation in patients undergoing cardiac surgery by heparin dosing based on heparin blood concentrations rather than ACT. Thromb Haemost 76(6): 902-908.
- Unsworth MJ, Herriot A, Valencia O, Poloniecki J, Smith EJ, et al. (1995) Resternotomy for bleeding after cardiac operation: a marker for increased morbidity and mortality. Ann Thorac Surg 59(3): 664-667.
- Karkouti K, Wijeysundrea D, Scott WB, Callum JL, Davy C, et al. (2007) Variability and predictability of large-volume red blood cell transfusion in cardiac surgery: a multicenter study. Transfusion (Paris) 47(11): 2081-2088.
- Tirilomis T, Bougioukas IG, Friedrich MG, Danner BC, Schoendube FA (2020) Re-exploration Early after Cardiac Surgery in Adults: The Importance of Bleeding-Related Complications. Heart Surg Forum 23(2): E174-E177.
- Karthik S, Grayson AD, McCarron EE, Pullan DM, Desmond MJ (2004) Reexploration for bleeding after coronary artery bypass surgery: risk factors, outcomes, and the effect of time delay. Ann Thorac Surg 78(2): 52734.
- Ramaker A, Meyer P (2009) Effects of acidosis, alkalosis, hyperthermia and hypothermia on haemostasis: results of point-of-care testing with the thromboelastography analyser. Blood Coagul Fibrinolysis 20(6): 4369.
- Carson JL, Noveck H, Berlin JA, Gould SA (2002) Mortality and morbidity in patients with very low postoperative Hb levels who decline blood transfusion. Transfusion 42(7): 812-818.
- Carson JL, Carless PA, Hebert PC (2012) Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. Cochrane Database Syst Rev 10(10): CD002042.
- Spiess BD, Ley C, Body SC, Siegel LC, Stover EP, et al. (1998) Hematocrit value on intensive care unit entry influences the frequenct of Q-Wave myocardial infarction after coronary artery bypass grafting. J thorac cardiovasc Surg 116(3): 460-467.
- Nutall GA, Olivier WC, Santrach PJ, Bryant S, Dearani JA, et al. (2001) Efficacity of a simple intraoperative transfusion algorithm for non erythocyte component utilization after cardiopulmonary bypass. Anesthesiology 94(5): 773-78 l.
- Avidan MS, Alcock EL, Da fonseca J, Ponte J, Desai JB, et al. (2004) Comparison of structured use of routine laboratory tests or near-patient assessment with clinical judgement in the management of bleeding after cardiac surgery. Br J Anesth 92(2): 178-186.
- Shore LL, Manspeizer HE, DePerio M, Francis S, Vela CF, et al. (1999) Thromboelastography-guided transfusion algorithm reduces transfusions in complex cardiac surgery. Anesth Analg 88(2): 312-319.
- Samiei N, Hakimi MR, Mirmesdagh Y, Peighambari MM, Ghavidel AA, et al. (2014) Surgical outcomes of heart valve replacement: A study of tertiary specialized cardiac center. Arya Atheroscler 10(5) :233-237.
- Carapetis JR, Powers JR, Currie BJ, Sangster JF, Begg A, et al. (1999) Oucomas of Cardiac Valve Replacement For Rheumatic Heat Disease in Aboriginal Australians. Asia Pacific Heart J 8(3) :138-147.
- Alizzi AM, Knight JL,Tylly PJ (2010) Surgical challenges in rheumatic heart disease in the australian indigenous population. Heart, Lung and Circulation 19(5-6) :295-298.
- Kangah MK (2010) Iterative valve surgery in Africa: indications, outcomes and risk factors. Cardiovascular Thoracic Surgery 15(4): 93-96.
- Dyke C, Aronson S (2014) Universal definition of perioperative bleeding in adult cardiac surgery. J Thorac Cardiovasc Surg 147(5): 1458-1463.
- Duranteau J, Asehnoune K, Pierre S, Ozier Y, Leone M, et al. (2015) Recommendations on resuscitation of haemorrhagic shock. Anesth Resuscitation 1(1): 6274.






























