Chylopericardium In a Young Woman Revealing A Mediastinal Cystic Lymphangioma: A Case Report
I Tlohi*, B Nassour, L Affendi, M Khalil and R Habbal
Department of Cardiology, CHU IBN ROCHD, Casablanca, Morocco
Submission: November 14, 2022; Published: December 01, 2022
*Corresponding author: Imane Tlohi, Department of Cardiology, CHU IBN ROCHD University hospital, Casablanca, Morocco
How to cite this article: I Tlohi, B Nassour, L Affendi, M Khalil, R Habbal . Chylopericardium In a Young Woman Revealing A Mediastinal Cystic Lymphangioma: A Case Report. J Cardiol & Cardiovasc Ther. 2022; 17(5): 555974. DOI: 10.19080/JOCCT.2022.17.555974
Abstract
Isolated chylopericardium due to mediastinal cystic lymphangioma is a rare entity. We report a case of asymptomatic chylopericardium in an 18 years old female with no history of trauma, thoracic surgery, malignancy, infection, or tuberculosis sand who presented with cardiomegaly noticed on chest x-ray before surgery of mandibular subluxation. Echocardiography showed a large number of pericardial effusions and pericardiocentesis yielded 1.25 L of milky-colored fluid which showed a triglyceride level of 4.82 g/L and cholesterol of 0.29 g/L with a cholesterol to triglyceride ratio of <1, characteristic of the chylous fluid. Chest computed tomography showed a huge mediastinal cystic lymphangioma. The patient successfully responded to continuous pericardial drainage and a medium-chain triglyceride diet then she was referred to the thoracic department for surgery. This type of case risks being misdiagnosed as tuberculosis, especially in countries where tuberculosis is endemic. Therefore, assessing pericardial fluid for chyle is crucial.
Keywords: Mediastinal cystic lymphangioma; Chylopericardium; Chylous pericardial effusion
Introduction
Chylopericardium effusion is characterized by the accumulation of chyle in the pericardium. It is often idiopathic but can occur after trauma, tuberculosis, chest radiation, and malignancy. Herein we describe chylopericardium effusion in a young woman revealing a huge mediastinal lymphangioma. To the best of our knowledge, this is the first reported similar case of chylopericardium effusion revealing a mediastinal cystic lymphangioma in South Africa.
Aim of the Study
We report this case in view of its rarity and is the first case report in South Africa of chylopericardium revealing mediastinal lymphangioma. We believe that this type of case risks being misdiagnosed as tuberculosis, especially in countries where tuberculosis is endemic. Therefore, assessing pericardial fluid for chyle is crucial.
Case Summary
An 18 years old female patient was admitted to the cardiology department of Casablanca’s university hospital for abundant pericardial effusion well tolerated. This pericardial effusion was suddenly discovered in front of cardiomegaly on a chest x-ray performed as part of a preoperative assessment of mandibular dislocation surgery.
She had no history of trauma, tuberculosis, thoracic surgery, neoplasm, or radiation therapy. The patient had no cough, sputum, dyspnea, chest pain, or swelling of the lower limbs. Clinical examination was unremarkable except for muffled heart sounds. Her blood pressure was 130/83 mmHg, and her heart rate was 88 beats/minute. Electrocardiography showed a sinus rhythm with low voltage complexes. Her laboratory tests showed a normal hemoglobin level at 12.5 g/dl, normal platelet count at 229000, normal white blood cells (WBC) at 6.79x103/μL, and lymphocytes at 1.25x103/μL. Biochemistry analysis revealed CRP at < 1 mg/l, total protein of 65 g/L, albumin 35 g/L, alanine aminotransferase (ALT) 7 U/L, aspartate aminotransferase (AST) 13 U/L, triglycerides 0.66 mmol/L, LDL cholesterol 2.19 mmol/L. Serum electrolytes were normal.
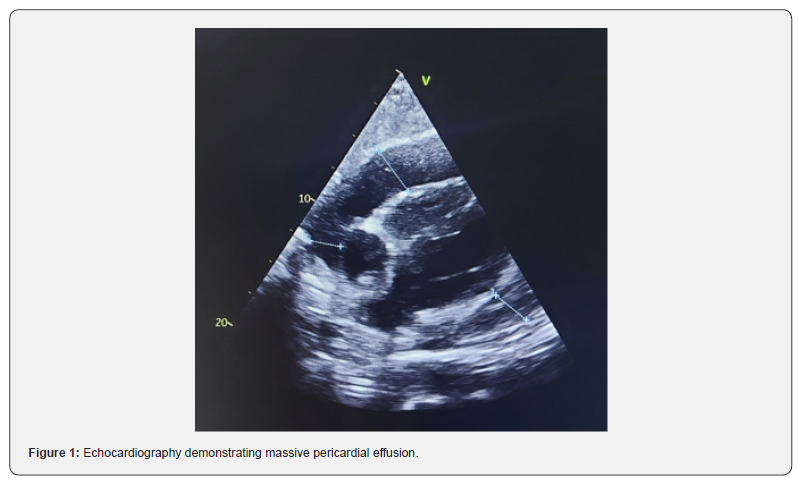
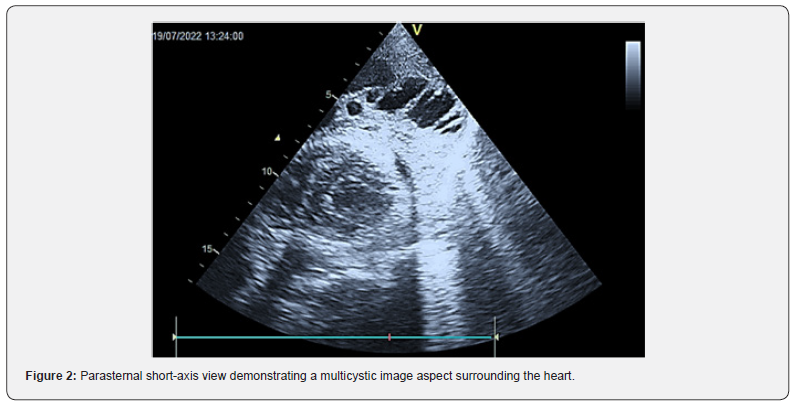
Serum creatinine was normal and the estimated glomerular filtration rate (eGFR, calculated with the MDRD formula) was 119 ml/min/1.73m2. Both blood culture and urine culture were sterile. Echocardiography revealed massive pericardial effusion (pericardial fluid of 3.2 cm at maximal thickness) with no cardiac tamponade and a multicystic image aspect surrounding the heart. Pericardiocentesis was performed via insertion of a pericardial drain removing 1250 cc of milky fluid. Cell counts and biochemistry in the pericardial effusion revealed WBC 425 × 106/L, lymphocytes count 93%, red blood cells 59 × 106/L, total protein 79 g/L, triglycerides 5.45 mmol/L, LDL cholesterol 0.41 mmol/L. Macrobiological analysis of the pericardial effusion didn’t detect any germs. Based on these findings the diagnosis of chylopericardial effusion was confirmed (Figures 1-2).
The indwelling pericardial catheter was removed when no fluid was drained after 10 days. A pericardial biopsy was performed revealing the presence of non-specific inflammatory cells with the absence of caseating necrosis or malignant cells.
As part of the etiological assessment, the detection of Mycobacterium tuberculosis in the pericardial fluid by the gen expert was negative, and 3 cultures of Koch’s bacillus in sputum were negative. Immunological analysis in search of systemic disease and thyroid hormone blood analysis was performed and their results were normal.
A thoracic-abdominal CT scan was realized that has shown the presence of large mediastinal mass occupying the anterior and middle compartments evoking a cystic lymphangioma. This mass is heterogeneous, with areas of low density (around 15 UH) and other areas discreetly enhanced after injection of contrast product, measuring 20 cm in maximum cross diameter, 12 cm in maximum anterior-posterior diameter, and extended over 20 cm in height. It encompasses in its circumference the heart and the large vessels for cervical-encephalic destiny without stenosis or reduction in their caliber with a suspected solution of continuity with the pericardium. Likewise it encompasses the tracheobronchial axis as well as its 2 branches without reduction of their size or endoluminal bud. It comes forward in contact with the anterior chest wall without bone lysis, outside it comes into contact with the mediastinal pleura without detectable sign of invasion, upwards it reaches the superior thoracic orifice (Figure 3).
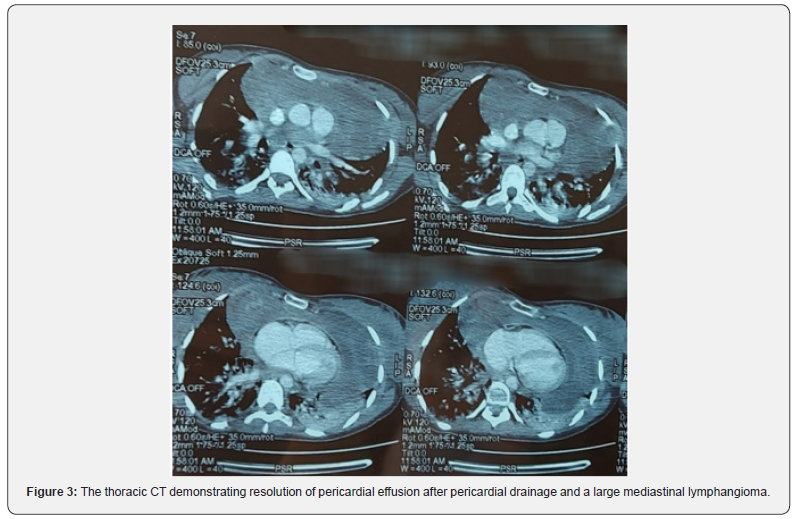
The patient successfully responded to continuous pericardial drainage and a medium-chain triglyceride diet then she was referred to the thoracic department for surgery.
Discussion
Chylopericardium is an uncommon disease entity in which chylous fluid accumulates in the pericardial cavity. It is secondary to a disruption or an obstruction of the thoracic duct that causes inadequate collateral drainage and reflux of chylous lymph through the lymphatics draining the heart and the pericardium [1- 2]. Cardiac surgery, chest trauma, radiation exposure, mediastinal tuberculosis, congenital mediastinal lymphangiectasia, and malignancy are the main causes [1-3].
Idiopathic chylopericardium is retained when all secondary causes of chylopericardium are excluded. The age at diagnosis ranges from 18 to 68 years and the clinical presentation may vary from incidental detection of cardiomegaly (as reported in our case) to those presenting dyspnea, coughing, chest pain, fatigue, or cardiac tamponade [4].
The diagnosis of chylous fluid is based on a milky yellowish appearance with a triglyceride level >500 mg/dL, a cholesteroltriglyceride ratio of <1, negative fluid cultures, and lymphocyte predominance [1]. Diagnosis of chylopericardium can also be made noninvasively by precordial imaging using 99Tc-labeled red blood cells or oral administration of 131I-triolein. As the anatomy of the thoracic duct is well known for its variations, identifying fistulous connections can be made by lymphangiography [5].
Lymphangiomas are benign lesions developed from malformed lymphatic channels. It’s an extremely rare vascular lesion which an incidence is 1:6000–16 000 [6,7]. They are most often located in the neck. Approximately 1% of all lymphangiomas are mediastinal, and lymphangiomas represent 0.7%–4.5% of all mediastinal lesions [6-8].
We distinguish three types of lymphangioma depending on the size of the lymphatic channels. The smallest type is known as capillary lymphangioma, followed by cavernous lymphangioma, and finally cystic lymphangioma (or hygroma). The most common is cystic lymphatic malformation [9].
The diagnosis is made in childhood in more than 90% cases, while adulthood manifestations are very rare [7,8]. Males and females are equally affected without race predilection. Chromosomal abnormalities such as Turner syndrome, Down syndrome, and trisomy 13 and 18 can be associated with mediastinal lymphangioma development [7,8]. It’s most often detected incidentally on chest X-ray as asymptomatic masses, but it can also be revealed by dyspnea, respiratory distress, congestive heart failure, syncope, arrhythmia, or cardiac tamponade [10].
The final diagnosis of a mediastinal lymphangioma is made on a histopathologic basis. However, clinical history, manifestation, anatomic location, and specific CT and MRI features can help narrow down the differential diagnoses including include mediastinal cyst, pericardial cyst, and thymic cyst [6].
Lymphangiomas appear on CT as a homogeneous lobulated mass with low attenuation similar to that of water but they can also have higher attenuation if they consist of a combination of fluid, fat, and solid tissue. They can be unilocular or multilocular with thin septations and it is rare to see calcification in them [10].
The treatment of lymphangiomas is based on complete surgical resection. Since they have a potential risk of recurrence, extensive resection is therefore recommended. However, when this is not possible (such as in the case of a huge mass or when vital structures are encased by the tumor), deroofing the mass is mandatory and most of the wall should be excised [10].
Alternative treatments were reported in the literature, when surgery is not feasible, including laser therapy, radiotherapy, chemotherapy, sclerosing agents, and observation (especially for lymphangiomas that are mostly located in the neck [11].
The prognosis following surgery is extremely favorable. Although regular postoperative follow-up review is highly recommended.
Conclusion
Mediastinal lymphangioma revealed by a chylous pericardial effusion is an uncommon clinical presentation. There are relatively few published reports of chylopericardium and lymphangioma represents a rare secondary cause of it. The diagnosis can be suspected on the data of echocardiography and CT but only histopathological proof can confirm it. The treatment is based on complete surgical resection that should be extensive since their a potential risk of recurrence.
Declarations
• Ethics approval and consent to participate: It is not applicable
• Consent for publication: In accordance with international and academic standards, written consent for publication was obtained from the patient and retained by the authors.
• Availability of data and materials: The datasets supporting this article are included in the article.
• Competing interests: The authors declared no conflicts of interest
Author’s Contributions:
This work was carried out in collaboration between all authors.
Acknowledgements:
None of the above.
References
- Dib C, Tajik AJ, Park S, Kheir MEL, Khandieria B, et al. (2008) Chylopericardium in adults: A literature review over the past decade (1996-2006) J Thorac Cardiovasc Surg 136(3): 650-656.
- Dunn RP (1975) Primary chylopericardium: a review of the literature and an illustrated case. Am Heart J 89(3): 369-377.
- Barbetakis N, Asteriou C, Konstantinou D, Giannoglou D, Tsilikas C, et al. (2010) Spontaneous chylous cardiac tamponade: a case report. J Cardiothorac Surg 5: 11.
- Dib C, Tajik AJ, Park S, Kheir ME, Khanderia B, Mookadam F (2008) Chylopericardium in adults: a literature review over the past decade (1996–2006) J Thorac Cardiovasc Surg 136(3): 650-656.
- Mehrotra S, Peeran NA, Bandyopadhyay A (2006) Idiopathic chylopericardium: an unusual cause of cardiac tamponade. Tex Heart Inst J 33(2): 249-252.
- Jeung MY, Gasser B, Gangi A, Bogorin A, Charneau D, et al. (2002) Imaging of cystic masses of the mediastinum. RadioGraphics 22(Spec No): S79-S93.
- D’Souza D, Weerakkody Y (2021) Lymphatic malformations. Reference article, Radiopaedia.org.
- Li O, Sallam YT, Kwan KF, Qiabi M, Paul NS, et al. (2022) Resection of a Large Hemorrhagic Mediastinal Lymphangioma in an Adult Patient: A Radiologic-Pathologic Correlation. Radiol Cardiothorac Imaging 4(1): e210043.
- Jeung MY, Gasser B, Gangi A, Bogorin A, Charneau D, et al. (2002) Imaging of cystic masses of the mediastinum. Radiographics 22 Spec No: S79-S93.
- Zakaria RH, Barsoum NR, El-Basmy AA, El-Kaffas SH (2011) Imaging of pericardial lymphangioma. Ann Pediatr Cardiol 4(1): 65-67.
- Park JG, Aubry MC, Godfrey JA, Midthun DE (2006) Mediastinal lymphangioma: Mayo Clinic experience of 25 cases. Mayo Clin Proc 81(9): 1197-203.






























