Prevalence of Cameroon Cardiovascular Risk Factors Linked to Severe forms of COVID-19
William Ngatchou1,2*, Jean Cyr Yombi3*, Francis Nde4, Michel P Hermans5, Philippe van de Borne6, Elysée Claude Bika Lele7,8, Liliane Mfeukeu Kuaté9, Charles Kouanfack10, Pascal Bovet11 and Daniel Lemogoum6,8,12
1Department of Surgery, Douala Faculty of Medicine and Pharmaceutical Sciences, University of Douala, Cameroon
2Hypertension clinic and Cardiac Surgery Department, St Pierre Hospital, Université Libre de Bruxelles, Brussels, Belgium
3Department of Infectious Diseases, Saint Luc University Hospital, Université Catholique de Louvain, Brussels, Belgium
4Department of Public Health, Université Libre de Bruxelles, Brussels, Belgium
5Endocrinology and Nutrition Unit, Cliniques Universitaires St-Luc, Université Catholique de Louvain, Brussels, Belgium
6Hypertension Clinic, Department of Cardiology, Erasme University Hospital, Université Libre de Bruxelles, Brussels, Belgium
7Physiology and Medicine of Physical Activities and Sports Unit, Faculty of Sciences, University of Douala, Douala, Cameroon
88Cameroon Heart Institute, Cameroon Heart Foundation, Douala, Cameroon
9Department of Medicine and Specialties, Faculty of Medicine and Biomedical Sciences, University of Yaoundé 1, Yaoundé, Cameroon
10Department of Public Health, Faculty of Medicine and Pharmaceutical Sciences, University of Dschang, Dschang, Cameroon
11Department of Epidemiology and Health Services, University Center for Primary Care and Public Health, Lausanne, Switzerland
1212Department of Medicine and Specialties, Faculty of Medicine and Pharmaceutical Sciences, University of Douala, Douala, Cameroon
Submission: January 22, 2021; Published: October 29, 2021
*Corresponding author: William Ngatchou, Department of Surgery, Douala University, Cameroon
How to cite this article: William N, Jean Cyr Y, Francis N, Michel P H, Philippe v d B, et al. Prevalence of Cameroon Cardiovascular Risk Factors Linked to Severe forms of COVID-19.J Cardiol & Cardiovasc Ther. 2021; 17(3): 555961. DOI: 10.19080/JOCCT.2021.17.555961
Summary
Objective: Several cardiovascular risk factors (CVFRs) have been linked with severe forms of the coronavirus disease 2019 (COVID-19). We examined the prevalence of adult Cameroonians with obesity, hypertension, and diabetes.
Methods: We extracted data of 19132 participants aged 18 years or above (57% men, mean age: 44∙5 years) from a nationwide cross-sectional study performed by the Cameroon Heart Institute between 2014 and 2019. Participants were recruited in the 10 regions of Cameroon using a multistage-cluster sampling frame. Socio-demographic and anthropometric variables, blood pressure (BP) and fasting capillary glucose were recorded. The distribution of CVRFs, with 95% confidence intervals, was estimated according to sex and age categories. We also examined the prevalence of combined CVRFs.
Findings: The age-standardized prevalence of hypertension, obesity, and diabetes was 39∙7%, 29∙2 %, and 8∙8 %, respectively. Among the participants, 56.0 % had at least one of the three considered risk factor, while 18∙4 % had two or three. The prevalence of having at least 1 of the 3 CVRFs was 43∙1% at age 18-44 years 69% at age 45-64 years. At age 65 years or more, 73∙6% and 18∙5%, respectively, had at least one or two risk factor(s).
Conclusion: The high prevalence of obesity, hypertension and diabetes in Cameroon underlies large proportions of people at risk of developing severe COVID-19 forms. In addition to the continued need to strengthen clinical and public health interventions to reduce the cardiovascular disease (CVD) burden in the population, it may be useful that national COVID-19 guidelines explicitly address screening, preventive and treatment procedures for people at increased risk of CVD.
Research in Context
Evidence before this study
Several studies reported that older patients and CVRFs such as hypertension, diabetes and obesity are associated with severe forms of COVID-19. However, data on the prevalence of these CVRFs is limited in sub-Saharan Africa.
Added value of this study
We analysed data from 19132 participants from a nationwide study performed by the Cameroon Heart Institute between 2014 and 2019. We found that 43% of adults in Cameroon aged 18-44 years, 69% of adults aged 45-64 years and 74% of adults aged 65 years or more had at least one risk factor (among obesity, high BP or diabetes), and could therefore be at increased risk of developing severe forms of COVID-19.
Implications of all the available evidence
The high prevalence of selected CVRFs in Cameroon emphasizes the need for clinical and public health interventions to reduce the burden of non-communicable diseases. In addition, given that several CVRFs increase the risk of developing severe COVID-19, recommendations for COVID-19 in Cameroon, and likely in other SSA countries, should explicitly specify procedures to prevent, detect and treat COVID-19 in persons with CVRFs, particularly in jeopardized and disadvantaged communities.
Introduction
The world is experiencing an unprecedented pandemic of coronavirus disease 2019 (COVID-19) due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). More than 96 million people have been infected worldwide, and nearly 2’000’000 deaths have been reported by January 19th, 2021 [1]. Mortality rates for patients admitted to intensive care units have been initially as high as 22% [2] in China and 26% in Italy [3], but have decreased substantially over time, possibly due to better case-management in hospitals, including better ventilation practices and potentially effective treatments [4].
The African continent seems to be less affected by the COVID-19 pandemic so far, although it is likely that COVID-19 cases and deaths are under-reported. As of September 6, 2020, the WHO estimated that there were over 1 million confirmed cases, with approximately 22,929 cumulative deaths in the region [1].
Hypertension, diabetes and obesity are major cardiovascular risk factors (CVRFs) of noncommunicable diseases [5,6]. Regardless of the COVID-19 pandemic, most sub-Saharan Africa (SSA) countries are facing a growing burden of cardiovascular and metabolic conditions, 5-7 mostly driven by the adoption of unhealthy lifestyles, resulting in an increasing prevalence of CVRFs such as obesity, hypertension, and type 2 diabetes mellitus (T2DM) [5-7,8].
In addition, the detrimental impact of CVRFs on health is aggravated with the advent of SARS-CoV-2 infection [5,7]. Indeed, many studies have now shown that severe form of COVID-19 occurs more often, among persons with comorbid conditions and CVRFs [9,10], including diabetes, obesity and hypertension. 3 For example, Adams et al. [11] estimated that 45∙4% of US adults were at risk of complications from COVID-19 as a result of gender, age, comorbidities and CVRFs. In Africa, a recent large cohort study in South Africa (SA) has shown that risk factors such as gender, age, hypertension, diabetes, HIV and tuberculosis were associated with COVID-19 poor outcome [12].
Black African ancestry was also reported to confer an increased risk of death from severe COVID-19 in the United States and in England [13], although it is not yet clear if race is a true cause or if the apparent effect is confounded by underlying unfavourable conditions such low socio-economic conditions and high burden of comorbidities in these population groups.
In Cameroon, several population-based surveys have indicated an increasing prevalence of hypertension, diabetes and obesity, predominantly in urban areas [8,14,15]. This could aggravate the outcomes of the ongoing COVID-19 pandemic, particularly in view of limited access of many inhabitants to adequate healthcare [1]. The present study aims to estimate the proportion of adults who might be at increased risk for complications and death from COVID-19, based on the prevalence of selected CVRFs.
Methods
This was a nationwide, cluster-specific cross-sectional, population-based survey carried out by the Cameroon Heart Institute between 2014 and 2019 in the 10 main regional cities of Cameroon, including Bafoussam (West), Bamenda (North-West), Bertoua (East), Buea (South-West), Douala (Littoral), Ebolowa (South), Garoua (North), Maroua (Far-North), and Ngaoundere (Adamaoua). Cameroon is a Central Africa country with an area of 472,442 km2 and a population of over 25 million inhabitants. The population density at national level is fairly low (56 inhabitants/ km2) but it can be much higher in urban areas, where more than half of the Cameroonian population lives [16]. The gross national income (GNI) per capita was 1,440 $ per capita in year 2018. At least 32∙8% of the population lives on less than US$ 1 per day [16].
In this study, a total of 19132 adults aged ≥18 years who declared permanent residency in the survey areas for the past 6 months, and gave informed consent, were included. Pregnant women were excluded. The detailed survey design and methods were previously described [14].
Participants were recruited using a three-cluster level sampling strategy, with health district at the first level, residency area the second level, and household at the third level. Data collection was largely consistent with the methodology of the WHO STEPwise approach for chronic diseases surveillance [17]. A closed-ended questionnaire assessed socio-demographic variables (age, sex, schooling, employment, etc.), medical history, current medications, smoking habits, alcohol intake, and physical activity. Body height was measured using a fixed stadiometer, and weight was measured using electronic medical scales. Body mass index (BMI) was calculated as weight in kilograms divided by the square of height in meter (kg/m2). Obesity was defined as a BMI ≥30.0 kg/m2.
Blood pressure (BP) was measured under standardized conditions [14] in a secluded place at home, after a 15-min rest and in the sitting position. Three consecutive BP measurements were carried out, at time intervals of 5 min, using a validated automated sphygmomanometer (HEM-705 CP, Omron Corporation, Tokyo, Japan) with a cuff width adjusted to the arm circumference. A fourth measurement was obtained if the first three readings differed by >10 mmHg. The averages of the nearest three BP and heart rate (HR) readings were considered in this study. Mean arterial pressure (MAP) was calculated as diastolic BP plus one-third of pulse pressure (PP; systolic BP minus diastolic BP). Hypertension was defined as a BP ≥140/90 mmHg and/or ongoing antihypertensive medication [18].
Participants were instructed to fast overnight for at least 8 hours and capillary fasting blood glucose (FBG) was determined using a glucometer (Accu-Chek Aviva, Roche, Mannheim, Germany). Diabetes mellitus was defined according to American Diabetes Association (ADA) criteria [19], i.e. a FBG ≥126 mg/dL (7 mmol/l) and/or being on glucose-lowering medication(s).
Ethical issues
This study was carried out in accordance with the recommendations of the Helsinki Declaration. Written informed consent was obtained from all participants. This study protocol received a research authorization from the Cameroonian Ministry of Public Health (n°061/L/MINSANTE/SG/DSPS/DSK) and an ethical approval from the Ethics Committee of the University of Douala (n° CEI-UD/61/02/2015/T).
All data were analysed using IBM SPSS® version 22. Quantitative variables are presented as mean ± standard deviation. Prevalence rates of CVRFs were expressed as frequencies and 95% confidence intervals (CI) and were age-standardized according to the Cameroon country’s age structure published in 2019. The distribution of CVRFs, with 95% CI, was tabulated according to sex and age categories and differences were tested using the Student-t test. A score of combined risk factors was calculated that ranged from 0 to 4, based on the presence of the 3 main risk factors considered in this study. Differences were considered significant for p-values less than 0∙05.
Results
Demographic, anthropological and biological characteristics are summarized in Table 1. There were 19,132 participants (57% men) of mean age of 44∙5years (range: 18-89). The overall agestandardized prevalence of CVRFs was 39∙7% for hypertension, 29∙2% for obesity and 8∙8% for diabetes.

BMI: body mass index; BP: blood pressure.
*Age-standardized
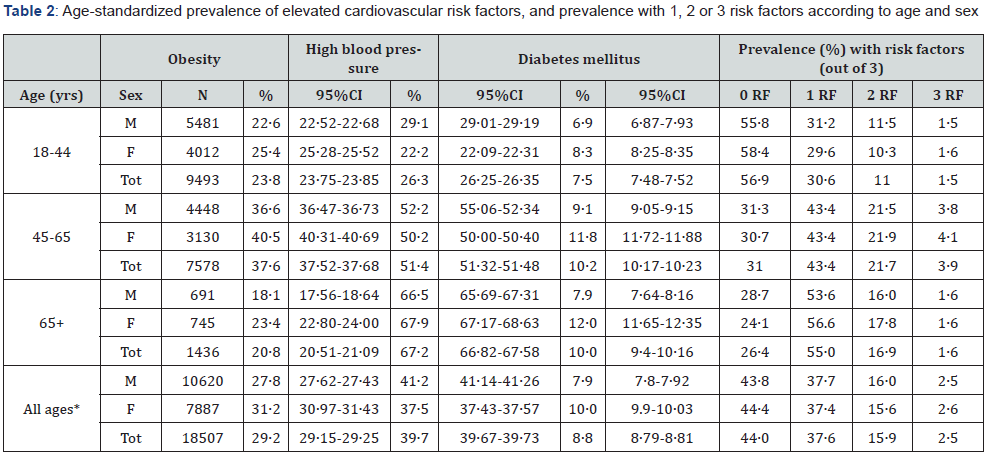
Obesity: BMI >30 kg/m2; High blood pressure: ≥140/90 mmHg or treatment. Diabetes mellitus: based on Fasting Blood Glucose ≥126 mg/dL and/ or being on glucose-lowering medication(s). BMI: body mass index; M: men, W: women; Tot: total. RF: risk factors.
Table 2 shows the prevalence of elevated CVRFs by sex and age. The prevalence of obesity increased with age and was more frequent in females than males (overall 29∙2%). The prevalence of high BP increased with age and was fairly similar in males and females (overall 39∙7%). The prevalence of diabetes increased with age and was higher in females than males (consistent with higher prevalence of obesity in females than males) and was 8∙8% overall.
As the prevalence of all 3 CVRFs increased with age, the proportions with respectively 1, 2 and 3 CVRFs increased with age (and the prevalence with 0 risk factor decreased with age). Of note, the prevalence of 1, 2 or 3 CVRFs was similar in all age ranges. The prevalence of having at least 1 CVRF, respectively at least 2 CVRFs were 43∙1% and 12∙5% at age 18-44 years, 69∙0% and 25∙6% at age 45-64 years, and 73∙6 and 18∙5% at age 65 years or more. Yet, considering the much smaller numbers of participants aged 65 years or more (which reflects figures in the entire population), and despite the fact that the proportions with at least 1 CVRF was as high as 73% among adults aged 65 years or more, the total numbers of persons with elevated CVRFs was low in this age category.
Discussion
As it is now well recognized, the prognosis of COVID-19 is worsened in older patients and in those with obesity, hypertension or diabetes [2,3,9,10,20] and it has therefore been suggested that these persons could benefit from specific management strategies [21]. Thus, it is useful to assess the prevalence of adults in SSA with one or several CVRFs, as an indication of the numbers of individuals at risk of developing severe forms of COVID-19 and who might benefit from particular preventive measures (e.g. more stringent physical distancing) and/or more intensive health care when developing COVID-19. We found that around 43% of adults in Cameroon aged 18-44 years, 69% of adults aged 45- 64 years and 74% of adults aged 65 years or more had at least one risk factor (among obesity, hypertension or diabetes), which could put them at increased risk of developing a severe form of COVID-19. This prevalence of CVRFs in Cameroon was at least as high in Cameroon as in some Western countries [5,22]. For example, a recent European study reported a prevalence of hypertension of approximately 25%, a prevalence of obesity of 21∙4% and a prevalence of diabetes of 6∙5% [22], i.e. less than in Cameroon. Findings in this study are slightly higher than in a previous nationwide survey in Cameroon in 2013, which reported a prevalence of 29∙7% for hypertension, 23∙5% for obesity and 6∙6% for diabetes, confirming the fairly high prevalence of CVRFs in Cameroon [15].
CVRFs increase the risk of development of severe forms of COVID-19 by several putative mechanisms. Obesity seems to increase the risk of severe COVID- 19 even among younger people [23]. For example, a study of 4,103 young patients with COVID-19 in New York City showed that a BMI >40 kg/m2 was associated with a six-fold increased risk of hospitalization [24]. Obese patients are prone to experience breathing difficulties due to biomechanical constraints, with hypoventilation and increased risk of respiratory infections. Obese patients often display increased levels of several inflammation markers, which may originate from adipocytes, and which predispose to so-called “cytokinic storms”. Overexpression of angiotensin-converting enzyme 2 (ACE2) was also observed in obese patients, which may contribute to thromboembolism events [25]. As already mentioned, obesity can impair respiration and gas exchanges, increase airway resistance, on top of other pathophysiological features such as decreased respiratory muscles strength and lung volume [26].
Infection by SARS-CoV-2 may alter insulin secretion and induce insulin resistance, which could worsen glucose homeostasis in diabetic or prediabetic patients [27]. High levels of troponin and natriuretic peptides were also observed in some critically ill patients, possibly related to inflammation of their vascular system, with diffuse microangiopathy and thrombosis. Inflammation of the myocardium has also been associated with fulminant myocarditis, heart failure, cardiac arrhythmias, acute coronary syndrome, rapid CV deterioration and sudden death [28].
Severe forms of COVID-19 have been linked to hypertension and CVD in many studies [29]. For example, two meta-analyses showed that hypertension increased the risk of COVID-19 mortality by 2-3 times [10,30]. However, the mechanisms linking high BP and severe COVID-19 are still unclear [9,31]. Unfortunately, we have not assessed the prevalence of stroke or other target organ damages in our population, but it is clear that the burden of stroke and chronic kidney disease is high in Cameroon given the high prevalence of hypertension, obesity and diabetes [32,33]. Since SARS-CoV-2 viruses enter the lungs and other cells by binding to ACE2 receptors, it was suggested that drugs such as angiotensinconverting enzyme inhibitors (ACEI) and angiotensin-receptor blockers (ARB) may enhance the expression of these ACE2 receptor at the cell surface, which could facilitate virus entry [34]. On the other hand, it has been argued that hypertensive patients may have decreased ACE2 receptor expression, which, once bound to the SARS-CoV-2 viruses, could decrease residual ACE2 receptor availability, leading to elevated angiotensin II, which could drive the onset of an acute respiratory distress syndrome [34]. It is believed that the benefit of maintaining RAAS blockers prescribed for chronic cardiovascular and/or chronic renal diseases might exceed their potential harm in patients with COVID-19 as RAAS inhibitors might protect against organ injury including myocardial injury caused by SARS-CoV-2 [34]. Importantly, a recent review of more than 80 studies showed no detrimental association of ACEI and ARB medications with either the risk of developing Covid-19 or Covid-19 prognosis, while a few studies suggested that these medications may be associated with improved outcomes in patients taking ACEI/ARB before developing Covid-19 [35]. The current recommendation is to continue RAAS inhibitors in both diabetic and non-diabetic hypertensive patients with COVID-19 [35,36].
An important finding of our study was the high proportion of adults in the general population with two or three of the CVRFs assessed in this survey (i.e., approximately 1 in 5 adults aged 45 years or above), which could put them at risk of developing severe COVID-19 [9,31]. Any of these CVRFs was associated with severe forms of COVID-19 in Asian and European studies [2,3,20]. For example, among 3200 young British adults aged 18 to 34 years hospitalized with COVID-19 (21% requiring ICU admission, 10% requiring mechanical ventilation, and 3% who died), over one third of them were obese (25% morbidly obese), 18% had diabetes, and 16% had hypertension [37]. Obesity, hypertension, and male sex were also found to be independent predictors of the need for mechanical ventilation and of death. This has suggested that young adults with multiple CVRFs may face COVID-19 risks similar to middle-aged adults without such risk factors [37].
The population of Cameroon is still relatively young, yet approximately 800,000 people are aged 65 years or above [16]. This corresponds to around 500’000 individuals with at least one CVRF (given a prevalence of around 73% at this age) and around 145,000 individuals have at least two CVRFs (given the prevalence of 18∙5% at this age). Yet, overall, age remains the main risk factor of severe forms of COVID, as shown in most countries. In Africa, age above 60 years was shown to increase COVID-19 mortality risk by more than 24 times as revealed by a recent study in South Africa [12].
Perspectives
This study found that a substantial proportion of the Cameroonian population may be at increased risk of developing severe forms COVID-19 based on the presence of CVRFs known to aggravate the disease or because of older age. This suggests a need to explicitly include, in national COVID-19 recommendations, specific preventive, screening and treatment measures in relation to the risk of severe forms of COVID-19 due to CVRFs and age. More generally, the high prevalence of CVRFs in the population of Cameroon reinforces the need to implement the main recommended barriers measures (physical distancing, hand washing and face masks in certain places). A strategy that also takes into account CVRFs may be useful in view of the weak health systems and limited access to COVID-19 care such as the insufficient numbers of ventilators and high flow of oxygen devices in Cameroon and, more generally, in SSA.
With regards to NCDs, our findings also emphasize the need to further develop programs and policy in multiple sectors to prevent and control CVD and other NCDs among both high-risk individuals and in the overall population, as suggested by WHO and PNUD [38,39]. For example, a syndemic approach, which takes into account both the burden of NCD and socio-economic inequalities, can be particularly relevant in the struggle against COVID-19 [40].
There are several limitations to this study. Firstly, the prevalence of hypertension may have been overestimated, since BP was measured on only one occasion, while hypertension should be diagnosed based on BP measurements on several visits and/or using ambulatory BP monitoring [41]. Secondly, tobacco use was not assessed in the present study. Tobacco consumption is a powerful CVRF and has also been shown to have a detrimental impact on the risk and prognosis of COVID-19 [42]. Thirdly, our survey did not assess the prevalence of comorbidities and CVD other than the CVRFs assessed in this study, which would have improved our ability to identify individuals at risk of developing severe COVID-19. The main strength of the study is the populationbased design of the survey based on several regions, which allows generalization of the findings to the entire Cameroonian population, and possibly to similar countries in the region, and the use of standard methods to assess the CVRFs of interest.
Conclusion
A high prevalence of hypertension, diabetes and obesity was found in the general adult population of Cameroon. Around twothirds of adults aged 45 years and above had at least one CVRF, and nearly one third had at least two CVRFs, which may expose them at increased risk of both CVD and severe forms of COVID-19. Our findings underscore the need for risk factor management among individuals at risk and for public health measures in multiple sectors to reduce the levels of CVRFs in the general population. Our data also suggest that national recommendations for COVID-19 could specify explicitly specific procedures and interventions for the prevention, screening and treatment of COVID-19 in relation to cardiovascular risk.
Conflicts of Interest
There are no conflicts of interest.
References
- https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200907-weekly-epi-update-4.pdf?sfvrsn=f5f607ee_2
- Wu C, Chen X, Cai Y, Xia J, Zhou X, et al. (2020) Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern Med 180(7): 934-943.
- Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, et al. (2020) COVID-19 Lombardy ICU Network. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA 323(16): 1574-158
- RECOVERY Collaborative Group; Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, et al. (2021) Dexamethasone in hospitalized patients with Covid-19 – preliminary report. N Engl J Med 384(8): 693-704.
- Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, et al. (2012) Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859): 2095-2128.
- NCD, Risk Factor Collaboration (NCD-RisC) (2017) Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 191 million participants. Lancet 389(10064): 37-55.
- Price AJ, Crampin AC, Amberbir A, Kayuni-Chihana N, Musicha C, et al. (2018) Prevalence of obesity, hypertension, and diabetes, and cascade of care in sub-Saharan Africa: a cross-sectional, population-based study in rural and urban Malawi. Lancet Diabetes Endocrinol 6(3): 208-222.
- Katte JC, Dzudie A, Sobngwi E, Mbong EN, Fetse GT, et al. (2014) Coincidence of diabetes mellitus and hypertension in a semi-urban Cameroonian population: a cross-sectional study. BMC Public Health 14: 696.
- Wei-jie G, Wen-hua L, Yi Z, Liang HR, Chen ZS, et al. (2020) Comorbidity and its impact on 1590 patients with COVID-19 in China: A nationwide analysis. Eur Respir J 55(5): 2000547.
- Wang B, Li R , Lu Z, Huang Y (2020) Does comorbidity increase the risk of patients with covid-19: Evidence from meta-analysis. Aging (Albany NY) 12(7): 6049-6057.
- Adams ML, Katz DL, Grandpre J (2020) Population-Based Estimates of Chronic Conditions Affecting Risk for Complications from Coronavirus Disease, USA. EID 26(8).
- Boulle A, Davies MA, Husey H et al. () Risk factors for COVID-19 death in a population cohort study from the Wester Cape Province, South Africa. Clinical Infectious Diseases. https://doi.org/10.1093/cid/ciaa1198.
- (2020) Covid -19 related deaths by ethic group England, Wales: Office for National Statistics.
- Lemogoum D, Van de Borne P, Bika EC, Damasceno A, Ngatchou W, et al. (2018) Prevalence, awareness, treatment, and control of hypertension among rural and urban dwellers of the Far North Region of Cameroon. J Hypertens 36 (1): 159-167.
- Kingue S, Ndong Ngoe C, Menanga AP, Jingi AM, N Noubiap JJ, et al. (2015) Prevalence and risk factors of hypertension in urban areas of Cameroon: a nationwide population-based cross-sectional study. J Clin Hypertens 17(10): 819-824.
- (2020) Cameroon's National Institute of Statistics. Statistics yearbook 2019. Chapter 4: Characteristics of the population 2019: 39-52.
- Organisation Mondiale de la Santé (OMS). Le Manuel de Surveillance STEPS de l’OMS : L'approche STEPwise de l'OMS pour la surveillance des facteurs de risque des maladies chroniques. Genève, Suisse, Organisation mondiale de la Santé, 2005. http://whqlibdoc.who.int/publications/2006/9789242593839 fre.pdf.
- Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, et al. (2013) 2013 ESH/ESC Guidelines for the management of arterial hypertension. The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 31(7): 1281-1357.
- (2010) American Diabetes Association (ADA). Standards of medical care in diabetes-2010. Diabetes Care 33(Suppl 1): 11-61.
- (2020) The European Society for Cardiology. ESC Guidance for Diagnosis and Management of CV Disease during COVID-19 pandemic.
- Zhou F, Yu T, Du R (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395: 1054-1062.
- Timmis A, Townsend N, Chris G (2018) European Society of Cardiology: Cardiovascular Disease Statistics 2017. European Heart Journal 39: 508-579.
- Lighter J, Philipps M, Hochman S (2020) Obesity in patients younger than 60 years is a risk factor for covid-12 hospital admission. Clinical Infections Diseases 71(15): 896-897.
- Petrilli CM Jones SA, Yang J (2020) Factors associated with hospitalization and critical illness among 4,103 patients with COVID-19 disease in New York City. Preprint at med Rxi.
- Madjid M, Miller CC, Zarubaev VV (2007) Influenza epidemics and acute respiratory disease activity are associated with a surge in autopsy-confirmed coronary heart disease death: results from 8 years of autopsies in 34,892 subjects. Eur Heart J 28(10): 1205-1210.
- Stefan N, Birkenfeld AL, Shulze M (2020) Obesity and impaired methabolic health in patients with COVID-19. Nat Rev Endocrinol 16(7): 341-342.
- Nguyen JL, Yang W, Ito K (2016) Seasonal influenza infections and cardiovascular disease mortality. JAMA Cardiol 1(3): 274-281.
- Fried JA, Ramasubbu K, Bhatt R (2020) The variety of cardiovascular presentations of COVID-19. Circulation 141(23):1930-1936.
- Kanwal A, Agarwala A, Warsinger L (2020) COVID-19 and Hypertension: What we know and don’t know. JACC
- Zhang J, Wu J, Sun X (2020) Associations of hypertension with the severity and fatality of SARS-CoV-2 infection: a meta-analysis. Epidemiol Infect 148: e106.
- Lippi G, Wong J, Henry BM (2020) Hypertension and its severity or mortality in Corona virus Disease 2019: a pooled analysis. Pol Arch Intern Med 130(4): 304-309.
- Lekoubou A, Nkoke C, Dzudie A (2017) Recurrent Stroke and Early Mortality in an Urban Medical Unit in Cameroon. J Stroke Cerebrovasc Dis 26(8): 1689-1694.
- Nganou-Gnindjio CN, Hamadou B, Boombhi J (2018) Target Organ Damage in Newly Diagnosed Hypertensive Individuals in Hospital Setting in Yaounde. EC Cardiology: 298-302.
- Vaduganathan M, Vardeny O, Michel T (2020) Renin-Angiotensin-Aldosterone System Inhibitors in Patients with Covid-19. N Engl J Med 382(17): 1653-1659.
- Mackey K, Kansagara D Vela K (2020) Risks and Impact of Angiotensin-Converting Enzyme Inhibitors or Angiotensin-Receptor Blockers on SARS-CoV-2 Infection in Adults. Ann Intern Med 173(3): 195-203.
- Lopes (2020) Continuing versus suspending ACE inhibitors and ARBs: Impact of adverse outcomes in hospitalized patients with COVID-19--The BRACE CORONA Trial.
- Cunningham JW, Vaduganathan M, Clagget BL (2020) Clinical outcomes in young adults hospitalized with COVID-19. JAMA Internal Medicine 181(3): 379-381.
- (2020) WHO Global Action Plan for Prevention and Control of NCDs 2013-20.
- Banatvala N, Small R (2020) Responding to non-communicable diseases during and beyong the COVID-19 pandemic. The BMJ Opinion
- Horton R (2020) Offline: COVID-19 is not a pandemic.
- Bovet P, Gervasoni GP, Ross AG (2003) Assessing the prevalence of hypertension in population: are we doing it right? J. Hypertension 21: 509-517.
- Patavanich R and Glantz SA (2020) Smoking is associated with COVID-19 progression: A Meta-analysis. Nicotine. Tob Res 04(13): 2006-3669.






























