Cardiac Tamponade Due to Primary Hypothyroidism: A Rare Presentation
Hind Tahri*, Imane Tlohi, Leila Azzouzi and Rachida Habbal
Ibn Rochd University Hospital, Casablanca, Morocco
Submission: March 18, 2020; Published: March 30, 2020
*Corresponding author: Hind Tahri, Department of Cardiology, Ibn Rochd University Hospital, Casablanca, Morocco
How to cite this article:Hind T, Imane T, Leila A, Rachida H. Cardiac Tamponade Due to Primary Hypothyroidism: A Rare Presentation. J Cardiol & Cardiovasc Ther. 2020; 16(1): 555930. DOI: 10.19080/JOCCT.2020.16.555930
Abstract
The occurrence of pericardial effusion during a hypothyroid state is frequent. This clinical evolution justifies the realization of an echocardiographic exam at diagnosis and during follow-up in the management of patient with hypothyroid disease. The pejorative clinical signs of pericardial effusion are relatively rare; the evolution into a pericardial tamponade is not frequently reported. This retrospective report covers the clinical evolution of 3 cases of pericardial tamponade commonly demonstrating a primary hypothyroidy. The echocardiogram allowed for immediate diagnosis of the tamponade; supported by the clinical aspect and the diagnosis of hypothyroidy confirmed biologically. The treatment approach was based on pericardiocentesis of the pericardial effusion associated with progressive hormonotherapy resulting in a favorable clinical outcome and the elimination of the pericardial effusion.
Keywords: Cardiac tamponade; Hypothyroidism; Pericardiocentesis
Background
Moderate to large pericardial effusion secondary to hypothyroidy is well described in the literature. Most of the reported cases highlight the rarity of cardiac tamponade in the setting of hypothyroidy, which is generally associated with recurrent viral infections contributing to the progression towards tamponade [1]. The etiology of pericardial effusions and early diagnosis are critical in determining the clinical evolution and prognosis of these cases while potentially avoiding often costly and unnecessary exams [2]. During our report, we discuss a series of three patients with pericardial tamponade associated to a hypothyroidy.
Cases Presentation
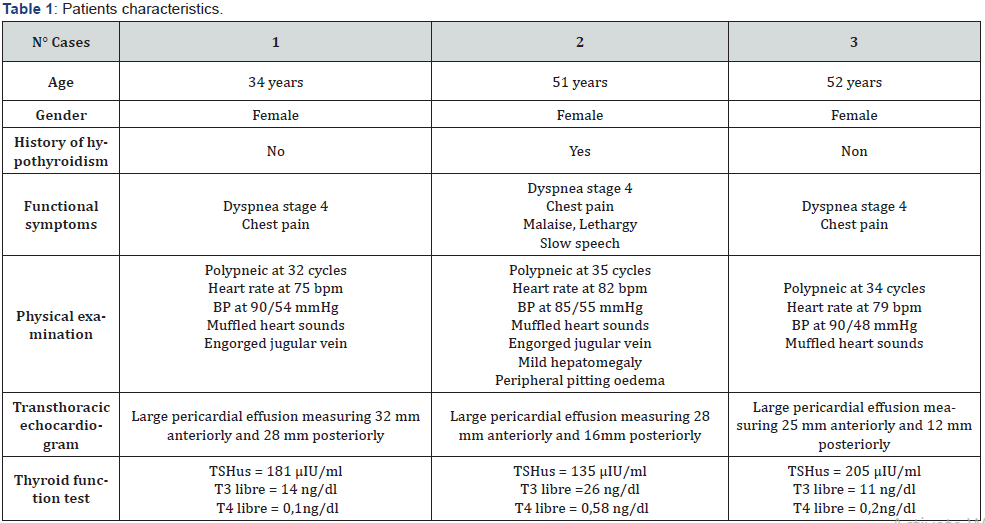
During 2019, three cases of tamponade were admitted to the Cardiology department at the University Hospital Center Ibn Rochd of Casablanca, of which the initial characteristics are presented in Table 1. The three cases were of female sex with a median age of 45 years. Two of the three cases presented flu-like symptoms a week prior to the hospitalization associated with the tamponade. The primary clinical signs were shortness of breath at rest and chest pain. All cases presented in a hypotensive state (without any signs of peripheric hypoperfusion) and symptoms of right heart failure. The thyroid gland was unpalpable in the three cases. Electrocardiogram (ECG) showed normal heart rate with low voltage pattern, electrical alternans were found in one patient (case 1). Thoracic radiography demonstrated cardiomegaly in the three cases as depicted in Figure 1.

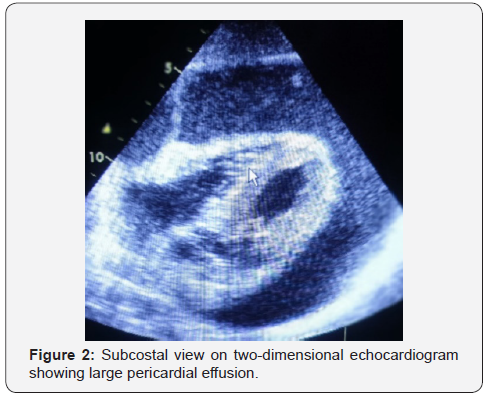
The transthoracic echocardiogram was realized in all cases demonstrating clinically relevant pejorative signs and representing indications to emergency intervention; in particular, the presence of pericardial effusion of great abundance with compressive signs (Figure 2).
A pulse wave Doppler showed significant respiratory variations in mitral and tricuspid inflow velocities during inspiration and expiration in the three cases. All patient underwent an emergency pericardiocentesis. The pericardial fluid was yellow and was sent for cytological and biochemical investigation. The diagnosis of hypothyroidy were based on the biological laboratory findings; elevated TSH levels and low levels of free T3 and T4. Other than the hormonal dosing of the thyroid, the biological findings were negative and accompanied by complementary gynecological examination, abdominopelvic echography, mammography, tuberculosis panel, and panel for systemic diseases. The median duration of hospitalization was 8 days. All patients were treated with thyroxine 100 μg daily which was later increased gradually to 200 μg daily with a positive clinical evolution. The 6-month follow-up exam was free of any signs with an echocardiogram negative for the presence of a recurrent pericardial effusion and a normalization of the TSH levels.
Discussion
Hypothyroidy can provoke pericardial effusions of various cavities including the pericardium, peritoneum, pleura, middle ear, uvea, joints, and scrotum [3]. These effusions are exudative in nature with a primary mechanism linked to the extravasation of the hygroscopic mucopolysaccharide in the cavities with increased capillary permeability, decreased lymphatic drainage, and greater retention of salt and water [4]. The fluid retention is generally slow. The pericardium has the ability to chronically distend; inhibiting any major hemodynamic changes even in massive pericardial effusions [5]. Effusions in hypothyroid patients are generally accompanied by elevated levels of cholesterol; with reported cases of cholesterol pericarditis causing tamponade [6]. Although pericardial effusions are frequent in hypothyroid state, cardiac tamponade is primarily an occurrence in cases with long-term disease or in patients with previous and confirmed hypothyroidy [2].
Most cases of cardiac tamponade are identified in older patients of female sex. There are reports of cases of massive pericardial effusions linked to hypothyroidism state in children [7]. It is important to note the presence of patients with clinically relevant pericardial effusions in hypothyroid patients without any clinical signs and symptoms of hypothyroid disease such as: weight gain, fatigue, and edema. This was also the case in two of the three patients (case 1 and 3 in this report where hypothyroid signs and symptoms were completely absent). Consequently, hypothyroidy is to be evaluated in all patients with an unexplained pericardial effusion.
The classical signs of cardiac tamponade (triad of Beck) are arterial hypotension, elevation of central venous pressure, and muffled heart sounds; of note these signs were not always present in the patients described in this report. Although the paradoxical pulse is habitual, it is not always evident. The pericardial friction is usual with effusion of low to medium abundance [8]. The ECG can carry clinical information in this setting by identifying a microvoltage with an electric alternance which can be caused by either pericardial effusion or myxedema. The diagnosis of pericardial effusion is generally suspected by a radiographic examination of the thorax and confirmed by cardiac echocardiogram which remains the gold standard with a high specificity and sensitivity. The echocardiographic signs of tamponade were present in the three patients in this report, associated with a tele-diastolic collapse of the right ventricle, compression of the right atrium, and a deviation of the interventricular septum in the left ventricle at inspiration [9].
With adequate medical treatment of hypothyroidism with thyroid hormones and steroids, the vast majority of pericardial effusions resolve slowly but completely; surgery is rarely required. Pericardiocentesis or surgical intervention are often not necessary unless the presence of pericardiac tamponade is confirmed [8]. The occurrence of cardiac tamponade in hypothyroidism is very rare due to the slow accumulation of fluid and pericardial distensibility. When tamponade occurs, it can be caused by provoking factors such as concomitant viral pericarditis.
Conclusion
Hypothyroidism should be ruled out in all patients with unexplained pericardial effusion. This should be considered in the general population and not exclusively in patients with clinically manifest hypothyroidism or in the elderly. Finally, once the diagnosis is established, treatment with thyroid hormones generally leads to the resolution of the pericardial effusion for 2-12 months without sequelae.
Competing Interests
The authors declare that they have no competing interests.
References
- Gupta R, Munyak J, Haydock T, Gernsheimer J (1999) Hypothyroidism presenting as acute cardiac tamponade with viral pericarditis. Am J Emerg Med 17(2): 176-178.
- Sagristà-Sauleda J, Mercé J, Permanyer-Miralda G, Soler-Soler J (2000) Clinical clues to the causes of large pericardial effusions. Am J Med 109(2): 95-101.
- Zimmerman J, Yahalom J, Bar-On H (1983) Clinical spectrum of pericardial effusion as the presenting feature of hypothyroidism. Am Heart J 106(4 Pt 1): 770-771.
- Lin CT, Liu CJ, Lin TK, Chen CW, Chen BC, et al (2003) Myxedema associated with cardiac tamponade. Jpn Heart J 44(3): 447-450.
- Shabetai R (2004) Pericardial effusion: haemodynamic spectrum. Heart 90(3): 255-256.
- Setty NSHDS, Sadananda KS, Nanjappa MC, Patra S, Basappa H, et al. (2014) Massive pericardial effusion and cardiac tamponade due to cholesterol pericarditis in a case of subclinical hypothyroidism: a rare event. J Am Coll Cardiol 63(14): 1451.
- Mehta S (2014) Cardiac Tamponade; A rare Presentation of Childhood Hypothyroidism. Iran J Pediatr 24(5): 663-664.
- Kabadi UM, Kumar SP (1990) Pericardial effusion in primary hypothyroidism. Am Heart J 120(6 Pt 1): 1393-1395.
- Honasoge AP, Dubbs SB (2018) Rapid Fire: Pericardial Effusion and Tamponade. Emerg Med Clin North Am 36(3): 557-565.






























