High Bioelectrical Impedance is Associated with High Blood Pressure Among US Adults - National Health and Nutrition Examination Survey, 2001 And 2002
Jing Guan1, Jian-Long Zhai2, Yu Wang3, Qing-Zhen Zhao3 and Chao Liu3*
1Stomatology Division, Hebei General Hospital, Shijiazhuang, China
2Heart Center, Hebei General Hospital, Shijiazhuang, China
3The First Cardiology Division, The First Hospital of Hebei Medical University, Shijiazhuang, China
Submission: January 13, 2020; Published: February 07, 2020
*Corresponding author: Chao Liu, The First Cardiology Division, The First Hospital of Hebei Medical University, 89 Donggang Road, Shijiazhuang, Hebei Province, China, 050031
How to cite this article:Guan J, Zhai J, Zhao Q, Liu C. High Bioelectrical Impedance is Associated with High Blood Pressure Among US Adults - National Health and Nutrition Examination Survey, 2001 And 2002. J Cardiol & Cardiovasc Ther. 2020; 15(5): 555923. DOI: 10.19080/JOCCT.2020.15.555923
Abstract
Background: Bioelectrical impedance analysis (BIA) is a simple method to estimate body composition. BIA measures the electrical impedance of body tissues that can be used to calculate an estimate of fluid volumes, total body water, body cell mass, and fat-free body mass. However, to our knowledge there are few studies that examine the relationship between BIA and blood pressure. Therefore, we designed the present study to test the relationship between blood pressure and BIA in US adults using data from the National Health and Nutrition Examination Survey (NHANES).
Methods: We reviewed data from 2328 subjects aged 18 years and older (maximum 49) who participated in the NHANES between 2001 and 2002. Blood pressure was indexed to the body mass index (BMI) to standardize the impact of fat tissue. The Pearson correlation coefficients were derived. We also conducted partial correlation using age and gender as co-variables to rule out the potential bias. A multiple linear regression was used to model the dependence of blood pressure on age, gender, and BIA.
Results: There was a significantly correlation between BIA (i.e. fluid volume) and systolic blood pressure (r = 0.35 to 0.39, P < 0.001) and diastolic blood pressure (r = 0.36 to 0.39, P < 0.001). All these correlations were further strengthened after adjusting for age and gender.
Conclusion: BIA (i.e. fluid volume) positively correlated to blood pressure in US adults; however, because this was an observational study, further investigation is needed to verify our results as well as identify the mechanisms.
Keywords: Bioelectrical impedance analysis; Body mass index; Systolic blood pressure; Diastolic blood pressure; Association; Adults
Abbrevations: BIA: Bioelectrical Impedance Analysis; BMI: Body Mass Index; BI: Bioelectrical Impedance; BP: Blood Pressure; MSNA: Muscle Sympathetic Nerve Activity; BCM: Body Cell Mass
Introduction
In human tissue, bioelectrical impedance is high in fat tissue and low in lean tissue. Nonfat or lean tissue is highly conductive due to its richness in intracellular fluid and electrolytes. Whereas, fat tissue contains very little fluid, thus has high resistance to electrical current. Bioelectrical impedance analysis (BIA) is a simple method to estimate body composition. BIA measures the electrical impedance of body tissues that can be used to calculate an estimate of fluid volumes, total body water, body cell mass, and fat-free body mass.
Hypertension is the most common chronic condition and one of leading causes of morbidity and mortality in the world. The causes of primary hypertension are complex and not fully understood. Nevertheless, the links between environmental factors, such as excess intake of salt, obesity, and perhaps sedentary lifestyle, and hypertension have been well established in studies over the past several decades. The efficacy of the diuretic therapy to alter fluid volumes and lower blood pressure has been proven in the patients with hypertension. Additionally, age also play an important role in the progress of hypertension because the aorta is stiffening with increasing age. It is worthy of noting that the above factors, such as obesity, body fluid volume, and age can affect the bioelectrical impedance (BI) as well. However, to our knowledge there are few studies that examine the relationship between BI and blood pressure (BP). Therefore, we designed the present study to test the relationship between BP and BI in US adults using data from the National Health and Nutrition Examination Survey (NHANES).
Materials and Methods
Study Sample
This cross-sectional study used data from 2328 subjects aged 18 and older (maximum 49) who participated in the NHANES between 2001 and 2002 [1]. The survey provides information on the demographics and health status of the US civilian, noninstitutionalized population by using a complex, stratified, multistage, probability-sampling design [2]. Demographic characteristics can be found in Table 1.
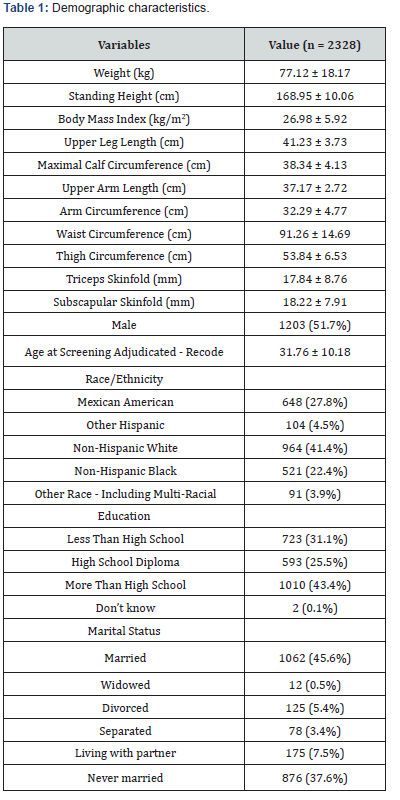
Data are expressed as mean ± standard deviation. BMI, body mass index.
Blood pressure measurement
The average systolic and diastolic pressures were used to analyze the relationships between BP and BI. The average BPs were calculated using the following protocol: If more than one BP readings were obtained, the first BP reading was excluded from the average. If there was only one BP reading, that reading was the average. If there were only two BP readings, the second BP reading was the average. If all diastolic BP were 0, the average was 0. Exception: if one of diastolic BP reading was 0, the diastolic BP reading with 0 was not used to calculate the average. If 2 of 3 diastolic BP reading are 0, then the reading that is not 0 was used to calculate the average [3].
BIA measurement
The protocol of BIA was described elsewhere [3]. In brief, the examinees were in a supine position. The arms should be separated from 15 degrees from the trunk of the body and the legs comfortably separated. Multi-frequency BIA, using different frequencies, was passed between surface electrodes placed on right hand and right foot. At frequencies below 5 kHz, and above 200 kHz, poor reproducibility has been noted. Therefore, we used 5, 50, 100, and 200 kHz to evaluated bioelectrical impedance.
Statistical analysis
Statistical analyses were carried out using SPSS 16.0 statistical package. Blood pressure was indexed to the Body Mass Index (BMI) to standardize the impact of fat tissue. The Pearson correlation coefficients were derived. We also conducted partial correlation using age and gender as co-variables to rule out the potential bias. A multiple linear regression was used to model the dependence of blood pressure on age, gender, and BI. Standardized coefficients were calculated to reflect the relationship between BP and the above variables. All statistical tests were two-sided and P-value < 0.05 was considered as significant.
Results
Correlation between systolic BP and BI
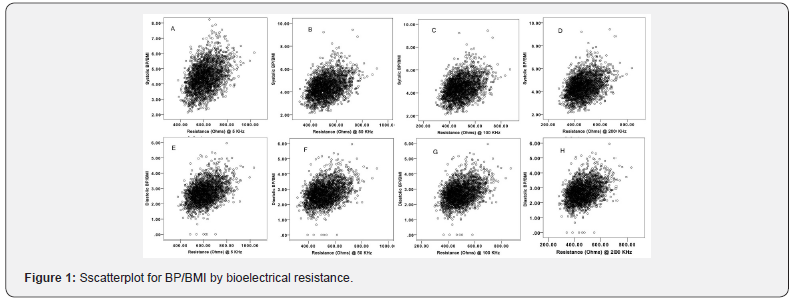
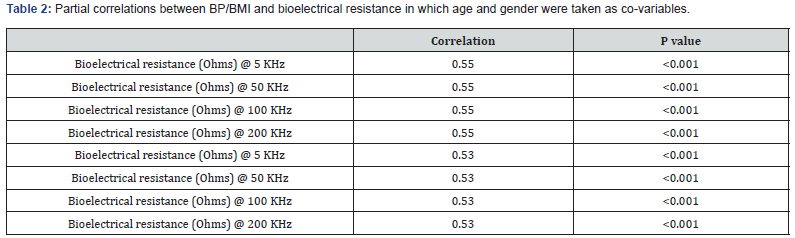
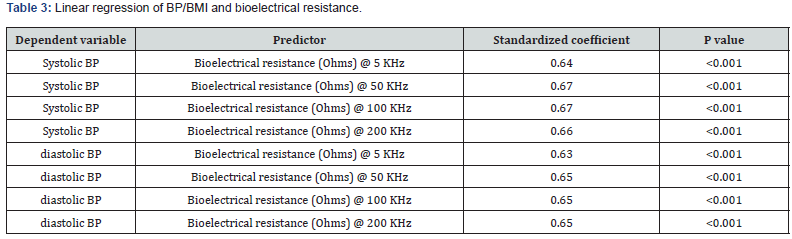
The analysis using Pearson’s correlation coefficient between BI and systolic BP are shown in Figure 1. There was a strong correlation between BI and systolic BP (Figure 1A-D). The correlations were consistent at variable frequency BIA, (5 kHz, 50 kHz, 100 kHz and 200 kHz). The correlation between BI and systolic BP remained unchanged in partial correlation in which age and gender were taken as co-variables (Table 2). In multiple linear regression models, standardized coefficients were calculated. Finally, the relationship between BI and systolic BP was established, which was consistent with unadjusted results.
Correlation between diastolic BP and BI
As showed in Figure 1 (Figure 1E-H), there was a strong correlation between BI and systolic BP using Pearson’s correlation coefficient. The correlations were consistent at variable frequency BIA, (5 kHz, 50 kHz, 100 kHz and 200 kHz). The correlation between BI and diastolic BP remained unchanged in partial correlation in which age and gender were taken as co-variables (Table 3). Similar to the above multiple linear regression model, the relationship between BI and diastolic BP was established as well (Table 3).
Discussion
Our study showed that there is a moderate but statistically significant positive correlation between BP and BI that is independent of age, BMI, and gender, indicating fluid volume overload contributes to the BP in adults.
Body mass and fat distribution with incidence of hypertension
A positive association of overweight and hypertension has been consistently reported from numerous cross-sectional and prospective studies over many decades. Over the past decades, a link between obesity and hypertension development has also been well established [4,5]. More specifically, visceral adipose, rather than total adiposity, play a more important role in this relationship [6]. It is well also well documented there is a positive association between overweight and high BI as well. However, the correlation between BP and BI remains unchanged after standardizing BP with BMI (i.e. the body fat mass) in the present study, indicating there must be some other mechanisms needing to be clarified.
Gender and blood pressure
Gender has an important impact on blood pressure. Premenopausal women tend to have lower arterial blood pressure and less risk of hypertension than age-matched men. Sex hormones such as estradiol and testosterone have direct impact on vascular, renal and heart cells. Overall, evidence showed that estradiol is anti-hypertensive, whereas testosterone is hypertensive [7]. Sex hormones also have direct role impact on body fat mass. To eliminate the impact of gender, we controlled the gender at partial correlation analysis. However, the association between BIA and systolic pressure still exist after controlling the impact of gender.
Antifungal resistance
As people age, blood pressure tends to increase, so does the risk of hypertension [7,8]. The mechanisms of age-related arterial blood pressure elevation are complex. Several underlying mechanisms have been proposed [9]. First, muscle sympathetic nerve activity (MSNA) increases with age [7], which can contribute to the increase in BP. Second, inflammation increases with age. Increased inflammation response leads to infiltrations of T cells and macrophages that could cause tissue injury and arterial stiffening. Third, the prevalence of metabolic syndrome also increased with age. In such subjects, vascular endothelial dysfunction and oxidative stress activates extracellular matrix metalloproteinases, resulting in vascular remodeling and arterial stiffening. To eliminate the impact of age, we controlled the age at partial correlation analysis. However, the association between BIA and systolic pressure still exist after controlling the impact of age.
The strengths of this study include the nationwide populationbased samples from national health surveys with largely identical sampling and measurement methods, the standardization of BP, weight and height measurements and the availability of highquality BIA data. It is a limitation of our analysis that we could not adjust for the intake of salt, fruit and vegetables that are related to both BMI and BP. These parameters were either not measured or lacked.
There are several limitations to the study. First, this is a crosssectional observational study. Thus, we are unable to draw a causal relationship between BI and hypertension. Second, we did not have available measures of site-specific adiposity, so we were unable to assess the relationship between adipose distributions and BP. The trunk of the body with its large cross- sectional area contributes as little as 10% to whole body impedance whereas it represents as much as 50% of whole-body mass [10]. Therefore, changes of the impedance are closely related to changes muscle mass or body cell mass (BCM) of the limbs,instead of the trunk. Even large changes in the visceral adipose within the abdominal cavity may have only minor influence on the measurement of fatfree mass or BCM [11]. Segmental-BIA may be helpful in providing information on fat accumulation in the abdominal region of the trunk.
Conclusion
Bioelectrical impedance, i.e. fluid volume, positively correlates to blood pressure in US adults; however, because this was an observational study, further investigation is needed to verify our results as well as identify the mechanisms.
Funding
The work was supported by grant number (no.20170313) Hebei Health and Family Planning Commission.
Disclosure
The authors have no conflict of interest to declare.
References
- Centers for Disease Control and Prevention, National Center for Health Statistics National Health and Nutrition Examination Survey Data US Department of Health and Human Services, Centers for Disease Control and Prevention, Hyattsville, MD (1999-2000).
- Naqvi AZ, Buettner C, Phillips RS, Davis RB, Mukamal KJ (2010) n-3 Fatty Acids and Periodontitis in US Adults. J Am Diet Assoc 110(11): 1669-1675.
- (2016) National Health and Nutrition Examination Survey: Body Composition Procedures Manual.
- Cassano PA, Segal MR, Vokonas PS, Weiss ST (1990) Body fat distribution, blood pressure, and hypertension. A prospective cohort study of men in the normative aging study. Ann Epidemiol 1(1): 33-48.
- Stamler R, Stamler J, Riedlinger WF, Algera G, Roberts RH (1978) Weight and blood pressure. Findings in hypertension screening of 1 million Americans. JAMA 240(15): 1607-1610.
- Chandra A, Neeland IJ, Berry JD, Ayers CR, Rohatgi A, et al. (2014) The relationship of body mass and fat distribution with incident hypertension: observations from the Dallas Heart Study. J Am Coll Cardiol 64(10): 997-1002.
- Hart EC, Joyner MJ, Wallin BG, Charkoudian N (2012) Sex, ageing and resting blood pressure: gaining insights from the integrated balance of neural and haemodynamic factors. J Physiol 590(9): 2069-2079.
- Writing Group M, Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, et al. (2016) Executive Summary: Heart Disease and Stroke Statistics--2016 Update: A Report From the American Heart Association. Circulation 133(4): 447-454.
- Sun Z (2015) Aging, arterial stiffness, and hypertension. Hypertension 65(2): 252-256.
- Lorenzo AD, Andreoli A (2003) Segmental bioelectrical impedance analysis. Current opinion in clinical nutrition and metabolic care 6(5): 551-555.
- Pirlich M, Schutz T, Spachos T, Ertl S, Weiss ML, et al. (2000) Bioelectrical impedance analysis is a useful bedside technique to assess malnutrition in cirrhotic patients with and without ascites. Hepatology 32(6): 1208-1215.






























