Intravascular Lithotripsy in Recently Implanted Underexpanded Drug Eluting Stents
Ief Hendrickx*, Jo Dens, Koen Ameloot and Mathias Vrolix
Ziekenhuis Oost-Limburg, Genk, Belgium
Submission: November 27, 2019; Published: December 20, 2019
*Corresponding author: Ief Hendrickx, Ziekenhuis Oost-Limburg, Schiepse bos 6, 3600 Genk, Belgium
How to cite this article:MIef Hendrickx, Jo Dens, Koen Ameloot, Mathias Vrolix. Intravascular Lithotripsy in Recently Implanted Underexpanded Drug Eluting Stents. 2019; 15(4): 555918. DOI: 10.19080/JOCCT.2019.15.555918
Non-Structured Abstract
Percutaneous coronary interventions of severely calcified lesions are often associated to poor procedural outcome and long-term stent failure. Extensive plaque modification by using intravascular lithotripsy can enhance stent expansion.
Keywords: Angiography; Coronary interventions; Calcified stenosis; Undilatable lesions
Abbreviations: IVL: Intravascular lithotripsy; ATM: Atmosphere; NSTEMI: Non-ST Elevation Myocardial Infarction; ECG: Electrocardiogram; LAD: Left Anterior Descendens; Cx: Circumflex; RCA: Right Coronary Artery; OCT: Optical Coherence Tomography; MSA: Minimum Stent Area; CT: Computer Tomography
Introduction
Severely calcified coronary arteries can be challenging and often require multiple plaque modification techniques before successful stent implantation. Lesion preparation with semi-compliant balloons is usually insufficient. Therefore, special balloons such as non-compliant, cutting, scoring and high-pressure balloons are frequently used. Atherectomy (or laser) is often the final step in lesion modification but is less effective in severe concentric calcification which extends deep in the vessel wall.
Intravascular lithotripsy (IVL) by Shockwave (Shockwave Medical, US) can be used for advanced plaque modification. Shockwave balloons generate pulsatile sonic pressure waves (up to 50 atmosphere) that passes through the surrounding tissue to create a series of micro-fractures in the calcium at a balloon pressure of 4 atmosphere (atm). In the DISRUPT CAD I study, this resulted in a clinical success of 95% without major dissections or perforations [1]. When lesions are not adequately prepared and calcium is insufficiently cracked, stent implantation may result in severe underexpansion which predisposes to stent thrombosis and in-stent restenosis [2]. The use of IVL to improve expansion of freshly implanted drug eluting stents is currently off-label. We present 2 cases in were IVL is used for successful optimization of expansion of recently implanted drug eluting stents.
Case Series
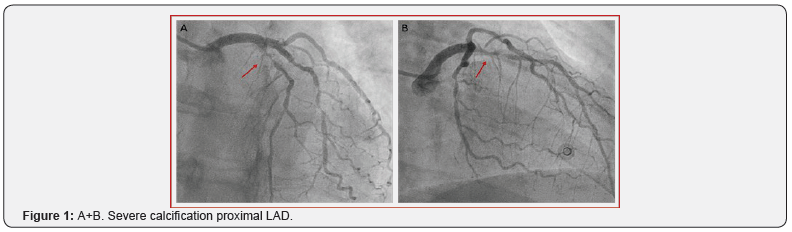
The first case is a 50-years old female patient who presented at the emergency department with Non-ST Elevation Myocardial Infarction (NSTEMI). The electrocardiogram (ECG) showed iso-electric ST-T segment with mildly elevated high-sensitive troponin T (152 ng/L, cut-off < 100 ng/L). Coronary angiography showed diffuse three vessel disease with the culprit lesion on the proximal Left Anterior Descendens (LAD) (Figure 1A+B). Because of the technical feasible approach in a non-diabetic patient, percutaneous coronary intervention was preferred above surgical revascularization. The LAD lesion was ad hoc treated and the other non-culprit lesions on the circumflex (Cx) and Right Coronary Artery (RCA) were staged.
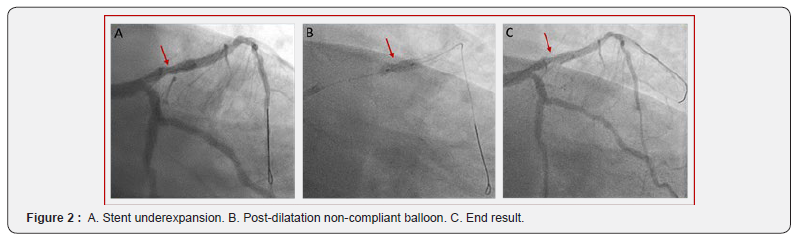
In the presence of severe calcification of the proximal LAD, plaque modification was performed using 3.0 mm semi-compliant balloon, 3.0 mm non-compliant balloon and 3.0 mm cutting balloon (Wolverine, Boston Scientific, US), followed by stent implantation (3.0 x 26 mm Resolute Onyx, Medtronic, US) (Fig 2A). Severe angiographic stent underexpansion persisted after aggressive post-dilatation with a 3.5 mm non-compliant balloon up to 26 atm (Figure 2B+C).
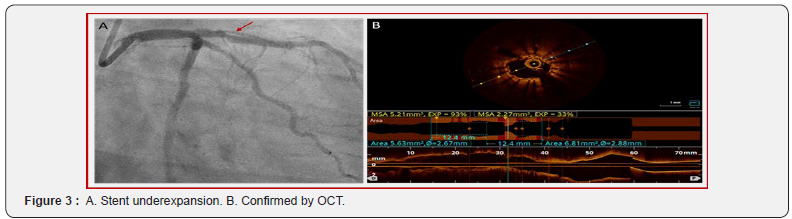
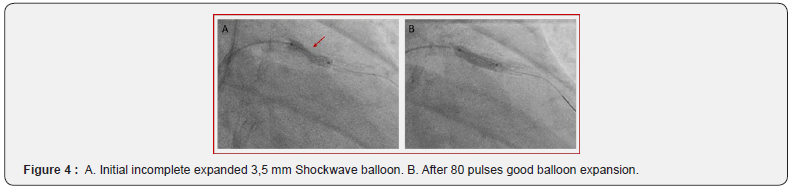
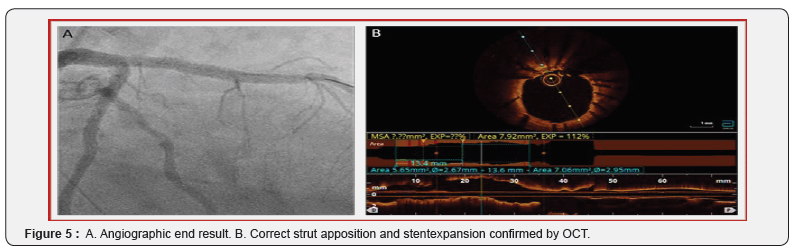
One week later, the non-culprit lesions on the Cx and RCA were successfully treated. Six weeks later, re-evaluation of the LAD stent was performed using Optical Coherence Tomography (OCT). Both coronary angiography and OCT (Figure 3A+B) confirmed significant underexpansion of the proximal LAD stent due to severe concentric calcification. The minimum stent area (MSA) was 2.27 mm² and stent expansion 33%. IVL was performed by using a 3.5 mm Shockwave balloon inflated at 4 atm with application of 80 pulses (8 runs of 10 pulses) at the narrowest segment. After application of all pulses, the balloon opened nicely (Fig 4A+B). Post-dilatation with a 3.5 mm non-compliant balloon up to 24 atm was repeated. The final result showed a full stent expansion with correct strut apposition, confirmed by OCT (Figure 5A+B). The MSA was 7.92 mm². Three-month clinical follow-up was reassuring with no subjective angina, normal echocardiography and exercise test.
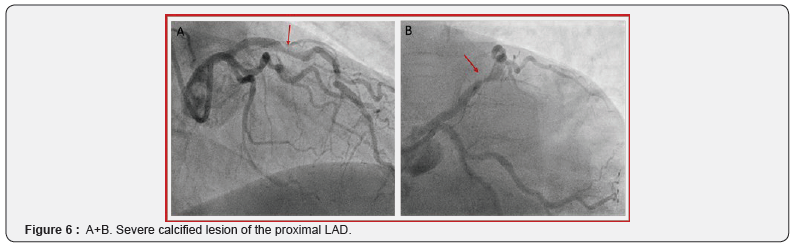
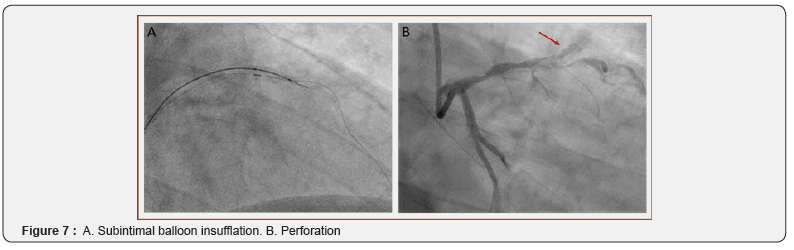
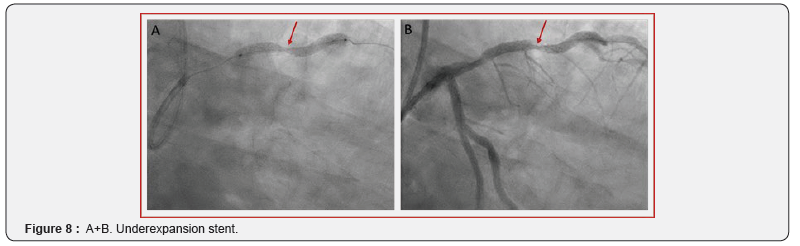
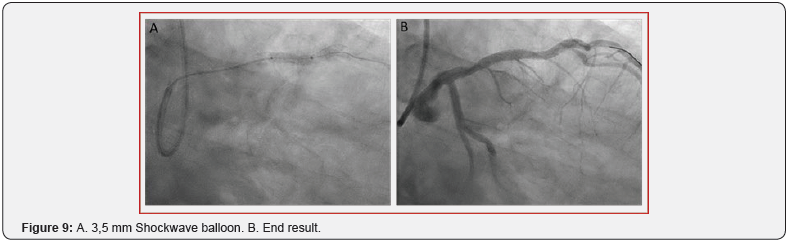
The second case is a 64-years old male patient who was referred to the cathlab because of stable angina and visualization of a severe stenosis of the proximal LAD on Computer Tomography (CT) scan. He had a normal resting ECG and preserved left ventricle function. Coronary angiography confirmed the severe calcified lesion on the LAD (Figure 6A+B). A 2.5 mm semi-compliant balloon was used for pre-dilatation. However, balloon rupture occurred and the balloon could not be retrieved (an intracoronary snare and a guide extension were not able to pass the balloon). To dislodge the trapped balloon fragment, which caused ST elevation due to absent distal flow, the technique of external crush was used (puncture and ballooning towards the subintimal space) followed by retrieval of wire and fragmented balloon (Fig 7A). Although the trapped balloon could now successfully be retrieved, this caused a perforation Ellis type II (Fig 7B). Since there was a perforation, no atherectomy was performed. Instead a new balloon dilatation followed by stent implantation was preferred (3.0 x 32 mm Synergy, Boston Scientific, US). The stent could seal the perforation but showed severe underexpansion (Figure 8A+ B). IVL was performed by using a 3.5 mm Shockwave balloon inflated at 4 atm with application of 60 pulses (6 runs of 10 pulses) (Figure 9A). Post-dilation was performed using a 3.5 mm non-compliant balloon with an acceptable angiographic residual underexpansion < 30% (Figure 9B). Seven months clinical follow-up was reassuring with no subjective angina and normal echocardiography and exercise test.
Discussion
Significant stent underexpansion, due to severely calcified lesions, predisposes to stent thrombosis and in-stent restenosis. The treatment by the conventional techniques is often limited because of poor contact with the calcification which extends deep in the vessel wall. Based on both cases, the use of intravascular lithotripsy in recently implanted underexpanded stents showed to be feasible and resulted in clear improvement of stent expansion despite balloon inflation of 4 atm. This also implicates that the stents struts may not be an obstacle for the pulsatile sonic pressure waves of lithotrispy. Similar cases have been presented previously [3-7]. Therefore, IVL could be an additional tool for stent optimization and is potentially safer when compared with super high pressure balloon inflations.
Conclusion
The outcome of both cases was successful, but the effects of IVL application on the stent polymer and drugs needs to be investigated more. In non-critical underexpansion (<50% on angiography), IVL probably can be postponed up to 6 weeks after implantation to allow drug delivery during the first weeks after implantation.
References
- Brinton TJ, Ali ZA, Hill JM, Meredith IT, Maehara A, et al. (2019) Feasibility of Shockwave Coronary Intravascular Lithotripsy for the Treatment of Calcified Coronary Stenoses. Circulation 139(6): 834-836.
- Zhang J, Gao X, Kan J, Ge Z, Han L, et al. (2019) Intravascular Ultrasound Versus Angiography-Guided Drug-Eluting Stent Implantation: The ULTIMATE Trial. J Am Coll Cardiol 72(24): 3126-3137.
- Salazar C, Escaned J, Tirado G, Gonzalo N (2019) Recurrent restenosis caused by severe calcific neoatherosclerosis treated with intravascular lithotripsy. Euro Intervention pii: EIJ-D-19-00268.
- Salazar C, Escaned J, Tirado G, Gonzalo N (2019) Undilatable Calcific Coronary Stenosis Causing Stent Underexpansion and Late Stent Thrombosis: A Complex Scenario Successfully Managed With Intravascular Lithotripsy. JACC Cardiovasc Interv 12(15): 1510-1512.
- Ali ZA, McEntegart M, Hill JM, Spratt JC (2018) Intravascular lithotripsy for treatment of stent underexpansion secondary to severe coronary calcification. Eur Heart J.
- Chen G, Zrenner B, Pyxaras SA (2019) Combined Rotational Atherectomy and Intravascular Lithotripsy for the Treatment of Severely Calcified in-Stent Neoatherosclerosis: A Mini-Review. Cardiovasc Revasc Med 20(9): 819-821.
- Watkins S, Good R, Hill J, Brinton TJ, Oldroyd KG (2019) Intravascular lithotripsy to treat a severely underexpanded coronary stent. EuroIntervention 15(1): 124-125.






























