Diabetes and Atrial Fibrillation
Marco Comaschi*
Department of Internal Medicine, ICLAS GVM Care & Research, Italy
Submission: December 04, 2019; Published: December 18, 2019
*Corresponding author: Marco Comaschi, Internal Medicine Unit - ICLAS GVM Care & Research - Rapallo (GE), Italy
How to cite this article:Marco Comaschi. Diabetes and Atrial Fibrillation. J Cardiol & Cardiovasc Ther. 2019; 15(4): 555917. DOI: 10.19080/JOCCT.2019.15.555917
Summary
The correlation between Atrial Fibrillation (AF) and Diabetes presents controversial aspects. The main studies performed on this topic are observational and epidemiological, retrospective and carried out on large health databases. However, a statistically significant independent link has been demonstrated, also related to the duration of the disease and the degree of metabolic control obtained. The alleged pathophysiological implications are due both to the alteration of the neurovegetative system common in diabetes, and especially to the insulin resistance component present in diabetic patients.
Keywords: Atrial fibrillation; Supraventricular arrhythmia; Pulmonary veins; Left atrium; Atrial depolarization
Introduction
Atrial fibrillation is the most common form of arrhythmia, after extrasystoles. It is a condition that affects 1-2% of the general population in Western countries; its prevalence increases with age and, at the same age, it is more frequent in males than in females. In juvenile age it is rare, but it affects 5% of people over 65, reaching 18% in the population aged 85 or over [1]. Atrial fibrillation is a supraventricular arrhythmia triggered by electrical impulses coming from myocardial muscle cells present at the junction between the four pulmonary veins and the left atrium.
In atrial fibrillation the electrical activity of the atria is completely disorganized and does not correspond to an effective mechanical activity. The waves of atrial depolarization, or f waves, are of small amplitude and have a very high frequency (400-600 pulses per minute). Under these conditions, the atrioventricular node (AVN) receives many more impulses from the atrium than it is able to conduct, thus exerting a filter function that transmits to the ventricles a number of beats that are not excessively high: numerous pulses penetrate, in fact, only partially in the AVN and lock into it. This variability of atrioventricular conduction causes the ventricles to contract irregularly. The electrocardiographically salient aspects of atrial fibrillation will therefore be the presence of f waves and the irregularity of beats. From the clinical point of view the atrial fibrillation is subdivided according to the way of presentation in:
a) Paroxysmal: when the episodes occur and resolve spontaneously in less than a week.
b) Persistent: when the arrhythmic episode does not stop spontaneously but only following external therapeutic interventions.
c) Permanent: when appropriate cardioversion attempts are not considered, or therapeutic interventions have proved ineffective.
Epidemiological studies
The theme of the relationship between atrial fibrillation (chronic or paroxysmal) and diabetes has been the subject of numerous scientific publications relating to as many studies, retrospective or prospective, always mostly observational, of an epidemiological nature. The number of studies that found a significant and presumably causal correlation between diabetes and AF is more or less equal to that of as many studies that did not detect this significance. This is to a large extent due to the designs of the studies carried out, often burdened by important defects of “recruitment” of the populations and cohorts taken into consideration, and by the objective difficulty to obtain certified diagnoses correctly dated, and, finally, by constant presence of other significant comorbidities such as other causes of arrhythmia.
The results of recent research indicate that FA is relatively common in diabetic people and should be considered as a “marker” of particularly adverse outcomes, which requires aggressive treatment of all risk factors [2]. The overlap of diabetes and AF also contributes to a well-defined increase in the risk of thromboembolic stroke [3]. Although both Diabetes and AF undoubtedly share common previous conditions, such as hypertension, atherosclerosis and obesity [4-6], the confluence of these two conditions clearly points towards the need for further studies. Diabetes has long been recognized as a risk factor for AF [7,8], and in several subsequent studies this has been reaffirmed [9-11]. However, the potential independent contribution of diabetes to the prevalence and incidence of AF has not been clearly evaluated until the work published by Nichols et al. [12] Diabetes Care in October 2009. These authors conducted a comparative analysis of the prevalence and incidence of AF in a very large population of diabetic and non-diabetic patients, taken from the Databases of the HMO Kaiser Permanente Northwest (480,000 subjects), from which a computer record was available for each individual of each medical examination, all standardized laboratory data and prescriptions received and dispensed by pharmacies in all clinics. The complete data related to people with diabetes were dating back to 1989. The study thus selected 17.372 diabetic subjects and as many non-diabetics from the same registry with identical characteristics (age, sex) (Table 1).
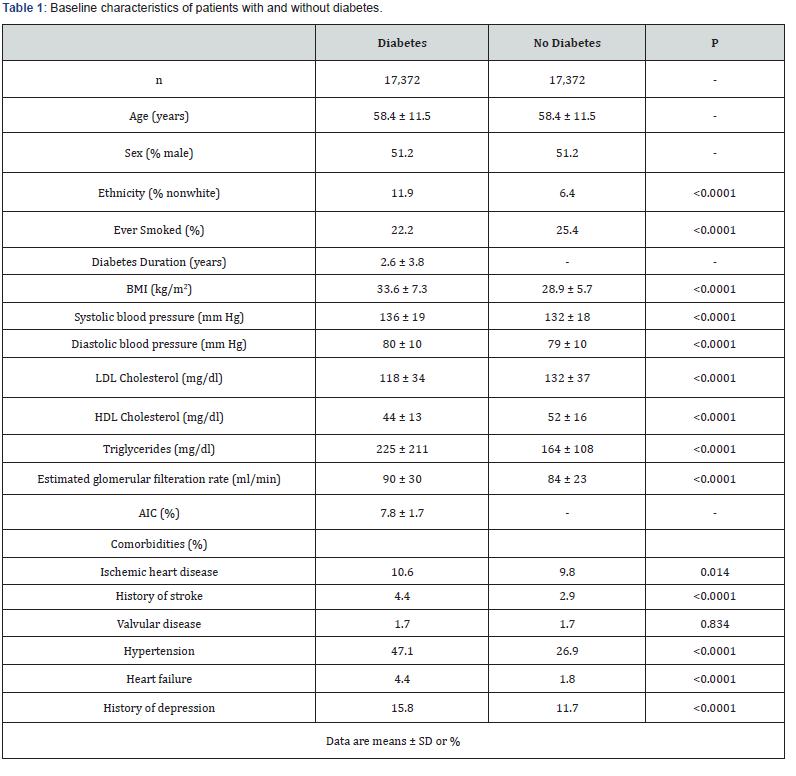
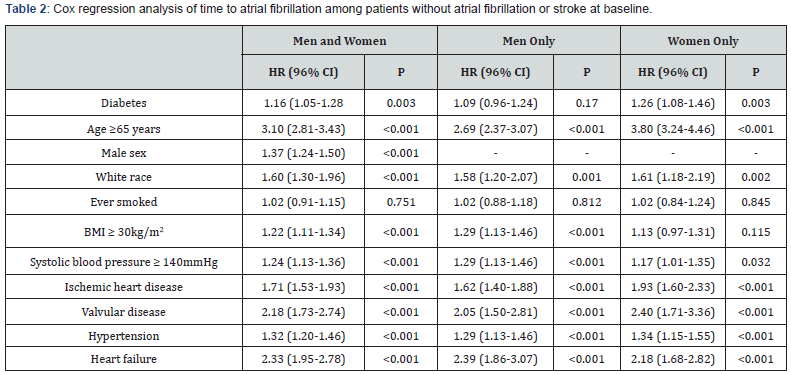
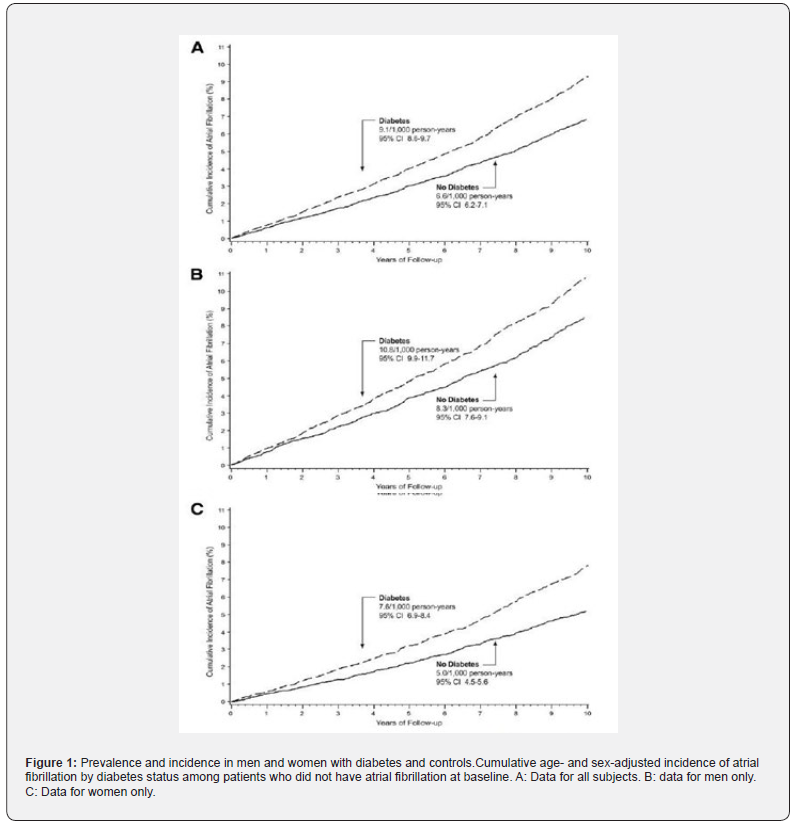
The prevalence of AF was significantly greater among patients with diabetes (3.6 vs. 2.5%, P _ 0.0001), increased with age in both groups, but significantly exaggerated among diabetics. This same relationship was also observed between males and females; although in men there was a higher prevalence of AF in each age group regardless of diabetes, the difference in prevalence between those with and those without diabetes was higher in women than in men. At a follow-up of 7.2 ± 2.8 years, the 16057 diabetics without AF nor history of stroke at the baseline developed AF at an incidence rate, adjusted for age and sex, of 9.1 per 1000 persons/year, compared with a rate of 6.6 among the 16471 nondiabetics. Diabetic people therefore had an additional 16% risk of presenting with AF (HR = 1.16), substantially higher in women (1.26) and not statistically significant in men (1.09) (Table 2 & Figure 1).
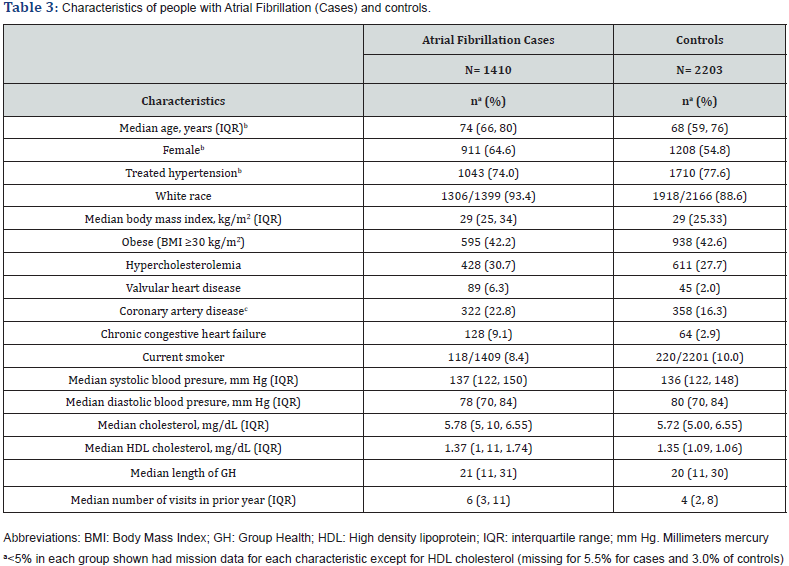
In this observational study, therefore, it was found that AF is 44% more prevalent and there is a greater probability of 38% developing it in the presence of diabetes, with a certain significance only for the female gender. However, the study did not take into consideration two parameters of great importance: the duration of diabetic disease and the degree of metabolic control. This defect was corrected by a publication of an American study in 2010 [13], reported by the Journal of General Internal Medicine. In this study the Authors have found, thanks once again to the computer databases, all the new cases of AF recorded from October 1, 2001 to December 31, 2004, selecting at the same time a control population “case-matched” by the same databases (Table 3).
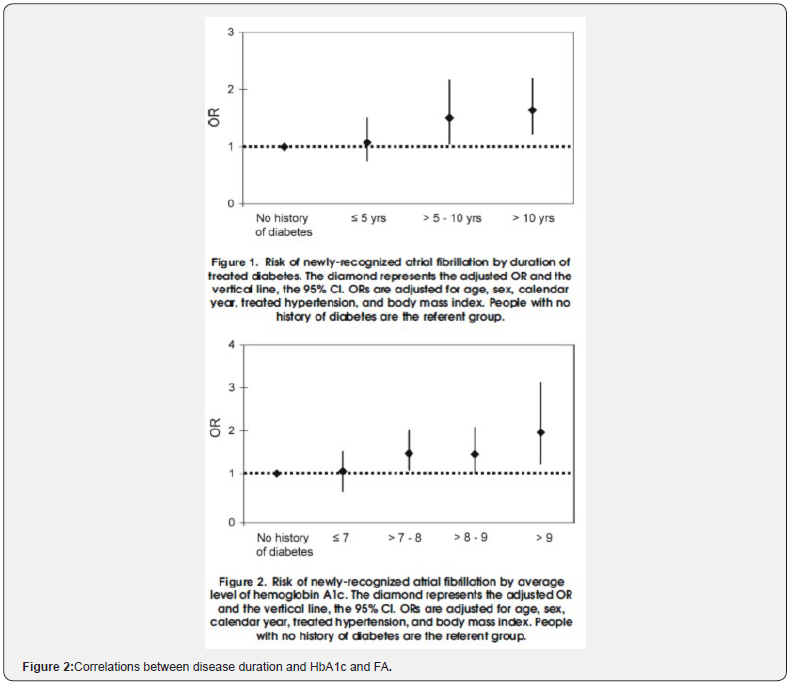
Treated diabetes was present in 17.9% of cases and in 14.1% of controls (OR = 1.40, adjusted for sex, age, hypertension in therapy and BMI). Diabetes without drug treatment was not associated with an increased risk of AF, while, among the subjects in therapy, the association in the presence of obesity was much stronger. The duration of the disease was shown as an element of progressive association (OR = 1.07 for duration <5 years, 1.51 between 5 and 10 years, 1.64> 10 years), allowing us to define that every year more of disease duration increased the risk of 3%. A specular result was obtained with the evaluation of the available data of HbA1c: OR = 1.06 for HbA1c <7%, 1.48 for HbA1c between 7 and 8%, 1.48 for HbA1c between 8 and 9%, and finally 1.96 for HbA1c> 9%. Also, in this case the degree of risk increase was defined for each point of HbA1c, equal to 14% more (Figure 2).
The same group of authors then published in 2012, again in the Journal of General Internal Medicine [14], a study centered on the association between permanent AF and BMI, as well as diabetes and hypertension. The results showed a strong and significant relationship between BMI and chronic AF, and not for the applicant, while they did not record significance with the presence of diabetes and hypertension. However, in this case diabetes was considered as an “on-off” factor, without any consideration for the duration of the illness or the degree of metabolic control. However, it remains a contribution of great importance also for the physiopathological implications related to insulin resistance and the inflammatory component present in the conditions of obesity.
Physiopathological considerations
What are the possible mechanisms behind these proven associations? The various published studies mainly focus on the anomalies of the autonomic nervous system, as possible mechanisms of triggering and maintaining the AF. In observational work the onset of AF episodes has been ascribed to changes in the autonomic tone [15]. Diabetic autonomic heart disease, although overestimated, is accompanied by the well-described autonomic neuropathy, and could play a greater role in the genesis of arrhythmia: further confirmation from well-conducted research would be necessary [16,17].
Moreover, several physiopathological mechanisms may underlie the relationship between diabetes and FA [18]. Diabetics have higher CRP levels [19-22], a marker of inflammation that could promote myocardial fibrosis and diastolic dysfunction [23]. Again, diabetes is associated with an enlargement of the left atrium [24] which could affect the development and propagation of electrical return circuits. Furthermore, diabetics are at greater risk of CHD and CHF, which may contribute to the development of FA, and, finally, in obese diabetics, there is a higher prevalence of OSAS [25,26]. In the same study DYDA [23], conducted by AMD and ANMCO on a population of Italian type 2 diabetics without clinical heart disease, a high prevalence of LV, diastolic and systolic dysfunction, absolutely asymptomatic and correlated with the degree of metabolic control and insulin resistance.
Conclusion
In conclusion, despite the limitations linked to the type of studies conducted, observational and retrospective, it can be reasonably stated that the association between the two clinical manifestations, diabetes and AF, exists and is significantly greater than in the population not affected by diabetes. The possible correlation with the various hypoglycemic therapies with which patients are treated remains to be explored; in the recent literature there are only two studies that have investigated this topic: in one case the reduction of the risk of AF was demonstrated in subjects treated with metformin [27] and in the second one by the same Authors, a similar protective action was carried out by the TZDs [28]. Both these classes of drugs act on the mechanisms of insulin resistance.
References
- Heeringa J, van der Kuip DA, Hofman A, Kors JA, van Herpen G, et al. (2006) Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. European Heart Journal 27(8): 949-953.
- Du X, Ninomiya T, de Galan B, Abadir E, Chalmers J, et al. (2009) Risk of cardiovascular events and effect of routine blood pressure lowering among patients with type 2 diabetes and atrial fibrillation: results of the ADVANCE Eur Heart J 30(9): 1128-1135.
- Tsang TS, Petty GW, Barnes ME, O’Fallon WM, Bailey KR, et al. (2003) The prevalence of atrial fibrillation in incident stroke cases and matched population controls in Rochester, Minnesota: changes over three decades. J Am Coll Cardiol 42(1): 93-100.
- Lloyd-Jones DM, Wang TJ, Leip EP, Larson MG, Levy D, et al. (2004) Lifetime risk for development of atrial fibrillation: the Framingham Heart Study. Circulation 110(9): 1042-1046.
- Benjamin EJ, Levy D, Vaziri SM, D’Agostino RB, Belanger AJ, et al. (1994) Independent risk factors for atrial fibrillation in a population-based cohort: the Framingham Heart Study. JAMA 271(11): 840-844.
- Nichols GA, Hillier TA, Brown JB (2007) Progression from newly acquired impaired fasting glucose to type 2 diabetes. Diabetes Care 30(2): 228-233.
- American Diabetes Association (2009) Total prevalence of diabetes and pre-diabetes.
- American Diabetes Association (2008) Economic costs of diabetes in the U.S. in 2007. Diabetes Care 31(3): 596-615.
- Benjamin EJ, Levy D, Vaziri SM, D’Agostino RB, Belanger AJ, et al. (1994) Independent risk factors for atrial fibrillation in a population-based cohort: the Framingham Heart Study. JAMA 271(11): 840-844.
- Furberg CD, Psaty BM, Manolio TA, Gardin JM, Smith VE, et al. (1994) Prevalence of atrial fibrillation in elderly subjects (the Cardiovascular Health Study). Am J Cardiol 74(3): 236-241.
- Psaty BM, Manolio TA, Kuller LH, Kronmal RA, Cushman M, et al. (1997) Incidence of and risk factors for atrial fibrillation in older adults. Circulation 96(7): 2455-2461.
- Nichols GA, Reinier K, Chugh SS (2009) Independent contribution of diabetes to increased prevalence and incidence of atrial fibrillation. Diabetes Care 32(10): 1851-1856.
- Dublin S, Glazer NL, Smith NL, Psaty BM, Lumley T, et al. (2010) Diabetes Mellitus, Glycemic Control, and Risk of Atrial Fibrillation J Gen Intern Med 25(8): 853-858.
- Thacker EL, McKnight B, Psaty BM, Longstreth WT Jr, Dublin S, et al. (2013) Association of Body Mass Index, Diabetes, Hypertension, and Blood Pressure Levels with Risk of Permanent Atrial Fibrillation J Gen Intern Med 28(2): 247-253.
- Bettoni M, Zimmermann M (2002) Autonomic tone variations before the onset of paroxysmal atrial fibrillation. Circulation 105(23): 2753-2759.
- Vinik AI, Maser RE, Mitchell BD, Freeman R (2003) Diabetic autonomic neuropathy. Diabetes Care 26(5): 1553-1579.
- Valensi P, Sachs RN, Harfouche B, Lormeau B, Paries J, et al. (2001) Predictive value of cardiac autonomic neuropathy in diabetic patients with or without silent myocardial ischemia. Diabetes Care 24(2): 339-343.
- Lip GY, Varughese GI (2005) Diabetes mellitus and atrial fibrillation: Perspectives on epidemiological and pathophysiological links. Int J Cardiol 105(3): 319-321.
- Aviles RJ, Martin DO, Apperson-Hansen C, Houghtaling PL, Rautaharju P, et al. (2003) Inflammation as a risk factor for atrial fibrillation. Circulation 108(24): 3006-3010.
- Bluher M, Fasshauer M, Tonjes A, Kratzsch J, Schon MR, et al. (2005) Association of interleukin-6, C-reactive protein, interleukin-10 and adiponectin plasma concentrations with measures of obesity, insulin sensitivity and glucose metabolism. Exp Clin Endocrinol Diabetes 113(9): 534-537.
- Yuan G, Zhou L, Tang J, Yang Y, Gu W, et al. (2006) Serum CRP levels are equally elevated in newly diagnosed type 2 diabetes and impaired glucose tolerance and related to adiponectin levels and insulin sensitivity. Diabetes Res Clin Pract 72(3): 244-250.
- Putz DM, Goldner WS, Bar RS, Haynes WG, Sivitz WI (2004) Adiponectin and C-reactive protein in obesity, type 2 diabetes, and monodrug therapy. Metabolism 53(11): 1454-1461.
- Cioffi G, Faggiano P, Lucci D, Maggioni AP, Manicardi V, et al. (2013) Left ventricular dysfunction and outcome at two-year follow-up in patients with type 2 diabetes: The DYDA study. Diabetes Res Clin Pract 101(2): 236-242.
- Rutter MK, Parise H, Benjamin EJ, Levy D, Larson MG, et al. (2003) Impact of glucose intolerance and insulin resistance on cardiac structure and function: sex-related differences in the Framingham Heart Study. Circulation 107(3): 448-454.
- West SD, Nicoll DJ, Stradling JR (2006) Prevalence of obstructive sleep apnoea in men with type 2 diabetes. 61(11): 945-950.
- Gami AS, Hodge DO, Herges RM, Olson EJ, Nykodym J, et al. (2007) Obstructive sleep apnea, obesity, and the risk of incident atrial fibrillation. J Am Coll Cardiol 49(5): 565-571.
- Chang SH, Wu LS, Chiou MJ, Liu JR, Yu KH, et al. (2014) Association of metformin with lower atrial fibrillation risk among patients with type 2 diabetes mellitus: a population-based dynamic cohort and in vitro studies. Cardiovasc Diabetol 13: 123.
- Chao TF, Leu HB, Huang CC, Chen JW, Chan WL, et al. (2012) Thiazolidinediones can prevent new onset atrial fibrillation in patients with non-insulin dependent diabetes. Int J Cardiol 156(2): 199-202.






























