Recurrence infectious Pericarditis Caused by Propionibacterium Acnes - a Case Report
Muhemin Mohammed1, Rein Jan Piso2, Jens Gerrit Hellige1 and Nisha Arenja1*
1Department of Cardiology, Kantonsspital Olten, Switzerland
2 Department of Medicine, Kantonsspital Olten, Switzerland
Submission: December 02, 2019; Published: December 18, 2019
*Corresponding author: Nisha Arenja, Department of Cardiology, Kantonsspital Olten, Solothurner Spitäler AG, Baslerstrasse 150, 4600 Olten, Switzerland
How to cite this article:Muhemin Mohammed, Rein Jan Piso, Jens Gerrit Hellige, Nisha Arenja. Recurrence infectious Pericarditis Caused by Propionibacterium Acnes - a Case Report. J Cardiol & Cardiovasc Ther. 2019; 15(4): 555916. DOI: 10.19080/JOCCT.2019.15.555916
Background
Abstract:Acute pericarditis is mostly caused by viral infection. In addition, rare cases of pericarditis can occur in association with rheumatic diseases and bacterial infections. Inadequate initial response to therapy may lead to very difficult management of chronic or recurrent pericarditis, which may result in pericardial constriction
Case Summary: We present an interesting case of a 57-year-old man with a history of hypertension. He presented with chest discomfort, dyspnoea and a history of flu-like symptoms. Physical examination, laboratory, and radiographic findings were consistent with acute pericarditis. In the course the patient suffered from several recurrences despite optimal therapy regime with Nonsteroidal Anti-Inflammatory Drugs (NSAID) and later Colchicine. A surgical exploration with pericardial fenestration was performed. The histological analysis identified Propionibacterium acnes as causative bacteria. The postoperative course was uneventful and the condition of the patient improved rapidly. However, after discharge, the patient’s condition worsened again and a rehospitalisation was necessary. This time a cardiac Magnetic Resonance Imaging (MRI) was performed, which demonstrated clearly pericardial oedema and late enhancement without myocardial involvement suggesting the diagnosis of Propionibacterium acne associated pericarditis without any further complications. For this time, the patient was treated with i.v. antibiotics. A systemic penicillin therapy had a dramatic beneficial effect and resulted in complete recovery of patients` condition.
Discussion:Pericarditis is a very uncommon complication of a systemic Propionibacterium acne infection. Prognosis dependents on the correct diagnosis and therapy. Our experience suggests diagnostic escalation in patients in initial therapy failure..
Learning point:When the initial response to therapy is inadequate, the differential diagnosis for rare conditions such as other infectious agent and systemic diseases should be considered
Keywords: Propionibacterium acne; Pericarditis; Pericardectomy; Cardiac magnetic resonance imaging
Abbreviations: NSAID:Nonsteroidal Anti-Inflammatory Drugs; CRP: C-Reactive Protein; CK: Creatine Kinase; ECG: Electrocardiogram; CMR: Cardiovascular Magnetic Resonance Imaging
Introduction
Acute pericarditis is a frequent disease caused by inflammation of the pericardium and can occur isolated or as a manifestation of a systemic disease. It is recorded in approximately 5% of all causes of chest pain presented to the Emergency Department and occurs in all ages, with equal incidence in males and females [1]. In most cases of acute pericarditis, a definitive aetiology is not pursued and possible viral origins (commonly enteroviruses, adenovirus) are considered without further diagnostic [2-5]. Other causes of acute pericarditis include malignancy and autoimmune disorders. Acute pericarditis is characterized clinically by a triad of chest pain, pericardial friction rubs with electrocardiographic changes [6]. However, pericarditis may be complicated by the development of a pericardial effusion, possibly triggering cardiac tamponade or can lead to a disabling syndrome of heart failure from pericardial constriction and, rarely, death [7,8]. Most patients respond well to nonsteroidal anti-inflammatory drugs (NSAIDs). Additional or as second-line therapy, Colchicine has been shown to be safe and effective [9,10].
In case of recurrence, or clinical features unresponsive to NSAIDs and colchicine, a diagnostic evaluation and further investigation should be considered.
Timeline
• One week before admission: The patient complained about flu-like symptoms.
• The day of admission: He presented with chest discomfort and dyspnea. The same day diagnosis of pericarditis was performed, and the patient was hospitalized.
• Day of discharge: Patients symptoms had improved and only residual pericardial effusion was recognized on echocardiography. An outpatient’s clinical follow-up was arranged.
• First outpatient control was two weeks later: This time he complained of relapsing symptoms. A combined therapy of NSAID and Colchicine was prescribed.
• Second outpatient control two weeks later. The patient was free of symptoms and the pericardial effusion was completely regredient.
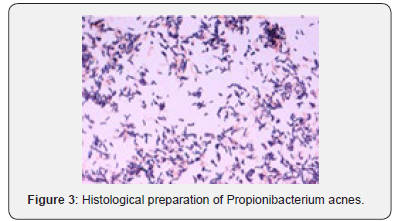
• Second patient’s presentation to the hospital was 3 months later due to progression of chest discomfort. The pericardial effusion was presented again and this time a surgical exploration with evacuation was performed. The symptoms improved rapidly, and the patient was discharged. The microbiological analysis identified in one of two different samples Propionibacterium acnes bacteria. As Propionibacterium acne is part of the skin flora, it was first considered as possible contamination.
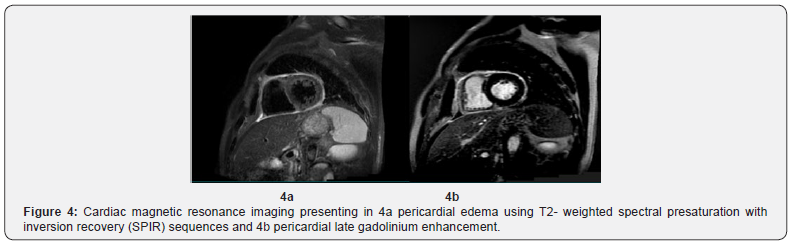
• One month later the patient presented with fever and the evidence of pericardial effusion. A CMR diagnosed pericarditis. The diagnosis of Propionibacterium acne associated pericarditis was now suspected and a resistance equitable antibiotic treatment started, which dramatically improved patients’ symptoms.
• Three months later: He was free of symptoms and there was no evidence of recurrence on clinical and echocardiography evaluation.
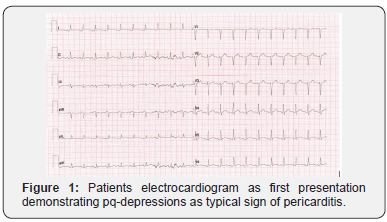
A 57-year-old caucasian man with chest discomfort and dyspnea was admitted to our hospital. He reported about flu-like symptoms, such as malaise, headache and cough a week before presentation. He was known for hypertension and gastroesophageal reflux disease. Medical history included a therapy with proton pump inhibitor and angiotensin-converting-enzyme inhibitor and he was a cigarette smoker. Physical examination was unremarkable, except of an elevated systolic blood pressure of 169/87mmHg at presentation. The laboratory investigations demonstrated elevated levels of C-Reactive Protein (CRP) of 60mg/L (normal value < 5mg/L) and leukocytes count of 11x10^9/L with a neutrophilia of 9.2x10^9/L (normal value 1.7-6.9x10^9/L), whereas the high-sensitive Troponin I and Creatine Kinase (CK) were in the normal range. The Electrocardiogram (ECG) showed sinus tachycardia (max. HF 129/min) with a specific PQ segment depressions (Figure 1). On transthoracic echocardiography the left ventricular was hypertrophic with the ejection fraction within the normal range (65%), without wall motion abnormalities and with normal valvular structures and function. The right ventricle was also normal in size and function. However, we found a circular pericardium effusion up to 5 mm, without any hemodynamic influence of the cardiac function.
After diagnosis of acute pericarditis, the patient was treated with a Nonsteroidal Anti-Inflammatory Drug (NSAID) (Ibuprofen 3 x 600mg), which is in accordance to European Society of Cardiologie (ESC) Guidelines for the diagnosis and management of pericardial diseases [10]. Since the patient’s condition improved after two days of hospitalization and the pericardial effusion showed regressive under therapy, a treatment escalation with Colchicine was not emendatory. Before discharge, a residual pericardial effusion was recognized on echocardiography and an outpatient’s clinical follow-up was arranged.
Case Presentation
In the first outpatient control he complains of worsening symptoms. The echocardiography demonstrated an increase in pericardial fluid collection. Therefore, we decided to add Colchicine with a dose of 0.5mg twice a day to the therapy. In the next outpatients control, a month after the combined treatment of NSAID and Colchicine, he was asymptomatic with no evidence of pericardial fluid. So, that NSAID were reduced in dose.
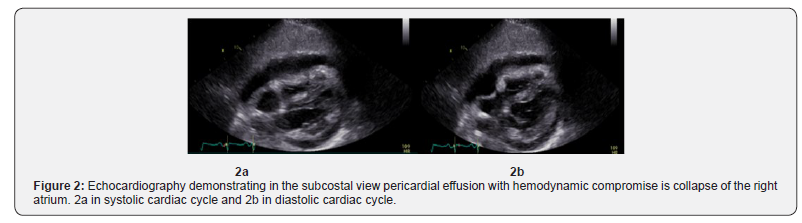
Three months after NSAID and Colchicine therapy the patient presented to our emergency department again reported worsening of the respiratory-depended chest discomfort and fever up to 39°C. This time the echocardiography affirmed an increased, hemodynamic relevant pericardial fluid (Figure 2a & 2b). Laboratory examination showed a highly elevated CRP of 243mg/L and leukocytes count of 13.5 x 10^9/L. Blood cultures were negative. Troponin value was under the cut-off and without any dynamic changes. In this situation, with worsening of symptoms and second clinical relapse despite double antiinflammatory therapy and suspicion of bacterial aetiology, we decided to perform a surgical exploration with evacuation and pericardium-fenestration. The microbiological analysis identified in one of two different samples Propionibacterium acnes bacteria with pus filled inflammatory exudate (Figure 3). Given the fact that Propionibacterium acne is a part of normal skin flora, we believed it to be unlikely the cause of the pericarditis and interpreted the results as a contamination. A few days after surgical exploration the patient’s condition improved rapidly and he could be discharged home. Two weeks after discharge, the patient presented again with the same clinical symptoms. Accordingly, a pericardial effusion up to 9mm was presented on echocardiography. Cardiovascular Magnetic Resonance Imaging (CMR) was performed to roll out further complications, which depicted significant pericardial oedema and delayed gadolinium enhancement of the pericardium without any myocardial involvement (Figure 4a & 4b). In the lack of other demonstrable infectious agent and cause, the patient was given the diagnosis of Propionibacterium acne associated pericarditis. Thus, the patient was treated 5gram intravenous Penicillin every 6 hours for two weeks. For the following two weeks Levofloxacin 2 x 500 mg and Rifampicin 2 x 500mg were prescribed. During the hospital stay the CRP value reached a maximum of 361mg/L and dropped then to 13mg/L. At followup visit 1 and 4 weeks after discharge the patient was free of symptoms. Further, both ECG and echocardiography as well as CRP values were normal. Until now the patient was not admitted to the hospital again and during phone follow up three months later he reported complete freedom of symptoms. The next control to rule out a constrictive pericarditis were carried out in private cardiology practice.
Discussion
Propionibacterium acnes are the most common colonizing bacterium of the skin. As an occasionally pathogenic anaerobe skin microbiota, they are also well known as the cause of acne vulgaris. The Propionibacteria resides mostly in the sebaceous glands and help to prevent the colonization of pathogenic organism by producing propionic-acid and other acidic agents [11]. Beside acne vulgaris, Propionibacterium is also well known as opportunistic pathogens causing postoperative and device related infections, such prosthetic valve, orthopedic and prosthesis infections. Furthermore, Propionibacteria are suspected in specific diseases like SAPHO-syndrome (Synovitis, acne, pustulosis, hyperostosis, osteitis), sarcoidosis und prostate cancer [12]. So far, pericarditis is very uncommon complication after a systemic Propionibacterium acne infection [13].
Conclusion
We presented a rare case of Propionibacterium acne associated pericarditis in an otherwise healthy patient. Detailed history, labor findings, ECG and echocardiography reveals the diagnosis in most of the cases. Generally, patients have a good response to NSAID treatment. However, in persistent signs of inflammations and recurrent pericarditis an early identification of the underlying cause may save the patient from developing late complications of pericarditis. In this case, pericardiectomy has occasionally been indicated to treat the refractory effusion and for investigation of rare causes of recurrent infection.s
Human Ethics
The patient obtained consent for case publication.
Acknowledgement
The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
References
- Groarke J, O'Brien J, Go G, Susanto M, Owens P, et al. (2013) Cost burden of non-specific chest pain admissions. Ir J Med Sci 182(1): 57-61.
- Lange RA, Hillis LD (2004) Clinical practice. Acute pericarditis. N Engl J Med 351(21): 2195-2202.
- Spodick DH (2003) Acute pericarditis: current concepts and practice. Jama 289(9): 1150-1153.
- Troughton RW, Asher CR, Klein AL (2004) Pericarditis. Lancet 363(9410): 717-727.
- Zayas R, Anguita M, Torres F, Gimenez D, Bergillos F, et al. (1995) Incidence of specific etiology and role of methods for specific etiologic diagnosis of primary acute pericarditis. Am J Cardiol 75(5): 378-382.
- Imazio M, Gaita F (2015) Diagnosis and treatment of pericarditis. Heart (British Cardiac Society) 101(14): 1159-1168.
- Kloos JA (2015) Characteristics, Complications, and Treatment of Acute Pericarditis. Crit Care Nurs Clin North Am 27(4): 483-497.
- Imazio M, Battaglia A, Gaido L, Gaita F (2017) Recurrent pericarditis. La Revue de medicine interne 38(5): 307-311.
- Imazio M, Gaita F (2017) Acute and Recurrent Pericarditis. Cardiol clin 35(4): 505-513.
- Adler Y, Charron P, Imazio M, Badano L, Baron-Esquivias G, et al. (2015) 2015 ESC Guidelines for the diagnosis and management of pericardial diseases: The Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC)Endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 36(42): 2921-2964.
- Shu M, Wang Y, Yu J, Kuo S, Coda A, et al. (2013) Fermentation of Propionibacterium acnes, a commensal bacterium in the human skin microbiome, as skin probiotics against methicillin-resistant Staphylococcus aureus. PloS one 8(2): e55380.
- Achermann Y, Goldstein EJ, Coenye T, Shirtliff ME (2014) Propionibacterium acnes: from commensal to opportunistic biofilm-associated implant pathogen. Clin Microbiol Rev 27(3): 419-440.
- Jensen TB, Kheyr MAE, Mohey R (2017) Constrictive pericarditis caused by Cutibacterium (Propionibacterium) acnes: A case report and review of literature. IDCases 10: 79-82.






























