Assessment of Left Ventricle and Left Atrial Function by Speckle Tracking Echocardiography in Hypertensive Patients
Imran Hameed*
Ziauddin University, Pakistan
Submission: November 27, 2019; Published: December 10, 2019
*Corresponding author: Imran Hameed, Anklesaria Nursing Home, Sir Aga Khan III Road, Garden, Karachi, Pakistan
How to cite this article:Imran Hameed. Assessment of Left Ventricle and Left Atrial Function by Speckle Tracking Echocardiography in Hypertensive Patients. J Cardiol & Cardiovasc Ther. 2019; 15(3): 555912. DOI: 10.19080/JOCCT.2019.15.555912
Abstract
Hypertension is a common clinical entity and is responsible for high cardiovascular morbidity and mortality. It affects especially the left sided chambers of the heart mainly i.e. the left ventricle and left atrium. Conventional parameters can detect the dysfunction in these chambers when it is too late. Speckle tracking echocardiography a relatively new modality but by virtue of its ease of use, angle independency and robustness can detect dysfunction at a sub-clinical stage, when effective remedies can save the patient from the deleterious effects of hypertension. In this manuscript the basics and the present clinical status of speckle tracking echocardiography in hypertensive patients have been reviewed.
Keywords: Hypertension; Echocardiography; Strain; Speckle tracking; Sub-clinical dysfunction
Introduction
Hypertension affects a large section of nearly every society in the world. According to World Health Organization worldwide data, its overall prevalence in adult population was 26.4% (95% CI 26.0 - 26.8%) in 2000 and by 2025 this has been projected to 29.2% (CI 28.8 – 29.7%) [1]. For this reason, it is one of the leading causes of CV mortality and morbidity especially heart failure [2]. Besides its deleterious effects on various body parts, heart and blood vessels are its main targets especially left ventricle and left atrium. The main function of left ventricle is to pump blood to meet the metabolic requirements of the body, any deterioration in it causes profound effects. Left atrium as we know is not just a passive chamber and its functioning is needed by left ventricle for effective performance. For decades now echocardiography has been the primary modality for assessment of cardiac chambers [3]. This could be in the way of size (diameters and volumes) or function (LV-E.F., etc. LA-diastolic parameters).
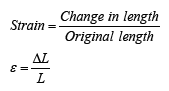
Later research has shown that pathological changes in these parameters are appreciated much later by the conventional methods of echocardiography. Another parameter known as “strain” was found to detect changes in the function of these chambers much earlier. Strain is the ratio of change in length of an object to its resting length on application of a force:
Discussion
Modalities for the acquisition of strain
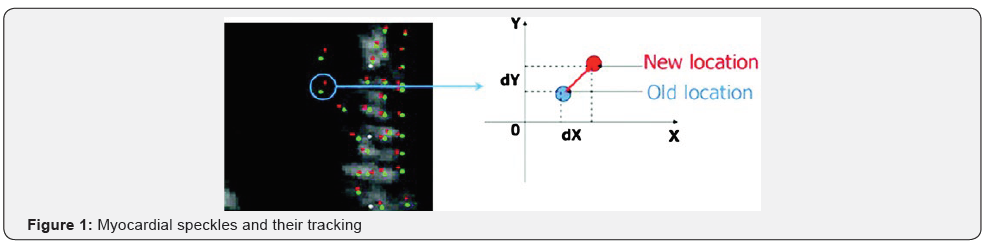
Detection of strain involved many different modalities like sonomicrometry and MRI tagging. The former, because of its invasive nature, could not be used in routine medical practice whereas tagged MRI, because of its cost and relative unavailability, also cannot be used for this purpose as a routine clinical tool. It has been found that during the acquisition of image by 2-D echocardiography as ultrasound strikes the myocardium, a part of it is reflected back, whereas much of it gets refracted and scattered, producing “speckles.” Movement of these speckles (each comprising of 20-25 pixels) during myocardial contraction can be tracked frame to frame, Figure 1, thus the shortening (or lengthening) of myocardial segment (and collectively of the whole myocardium) can be assessed easily. This phenomenon is known as “speckle tracking.”
Types of Left ventricle strain
Heart muscle, in left ventricle, is arranged in three layers with muscle fibers in the sub-endocardial layer making an angle of 80 degrees (right-handed helix) with the horizontal and as they wrap further towards the sub-epicardial layer get more horizontal, making an angle of nearly 60 degrees (left-handed helix), Figure 2 well elaborated and illustrated by Sotoru Kishi [4].

Due to three layered orientation of muscle fibres in Left ventricle contraction occurs in three directions as follows:
a) Longitudinal: shortening occurs along the length of left ventricle mainly due to sub-endocardial fibers.
b) Circumferential: shortening occurs along the circumference of left ventricle mainly due to mid myocardial fibers.
c) Radial; thickening occurs towards the center of left ventricle mainly due to mid and sub-epicaradial fibres.
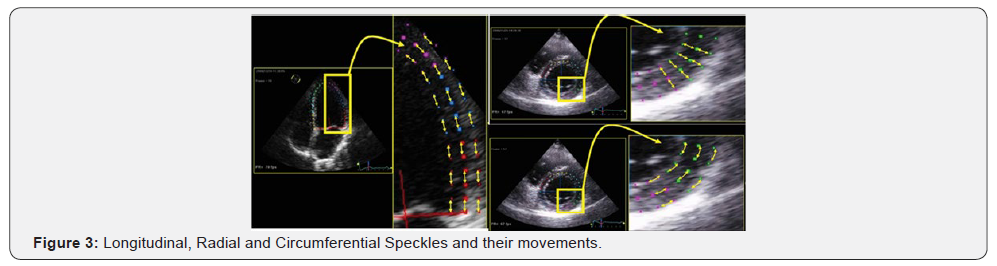
Speckles generated by these three layers can be tracked in the three directions of their movement during contraction [5] as shown in Figure 3, which are referred to as strain of that particular type [6], Figure 4. By assessment of circumferential strain, we can calculate the basal and apical rotation of left ventricle as well. The difference between these two is “twist” and dividing it by the LV length, gives “torsion.”
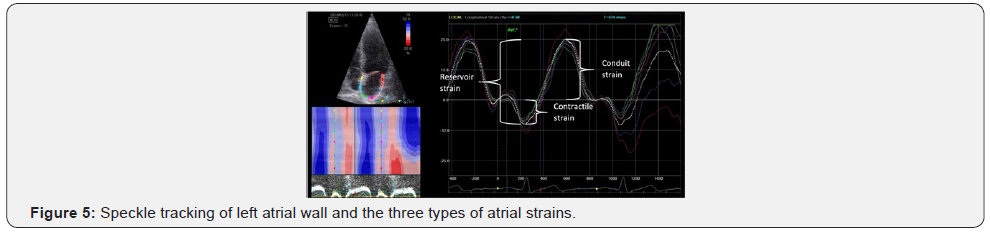
Types of Left atrial strain
Left atrium serves three functions viz. reservoir, conduit and contractile, all of which can be assessed by tracking speckles of LA wall [7] as shown in Figure 5. Changes in these parameters are noted much earlier than any change in size or diastolic parameters can be demonstrated.
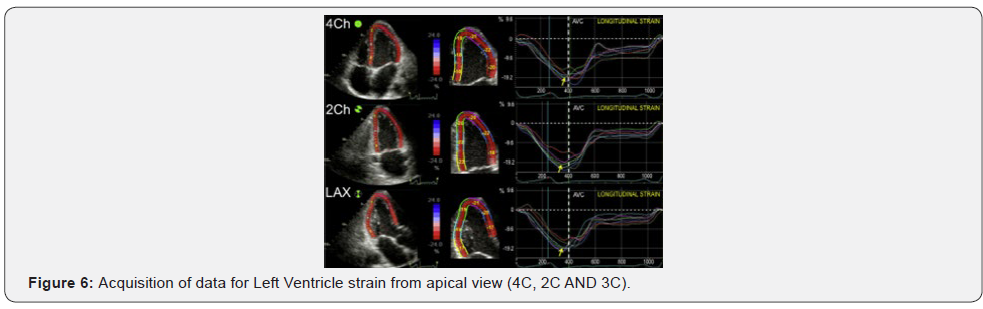
Data acquisition for strain analysis by speckle tracking echocardiography
For LV assessment, data is acquired by obtaining three apical views (4C, 2C and 3C) Figure 6 and three parasternal short-axis views (at base, mid and apex).
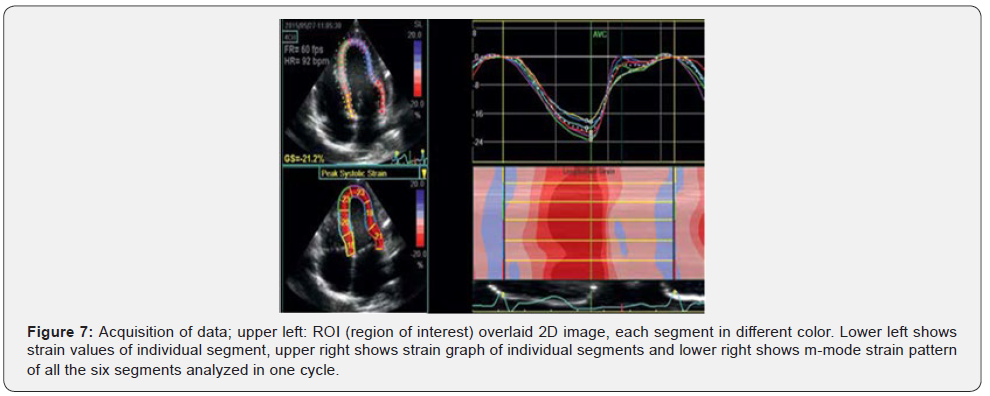
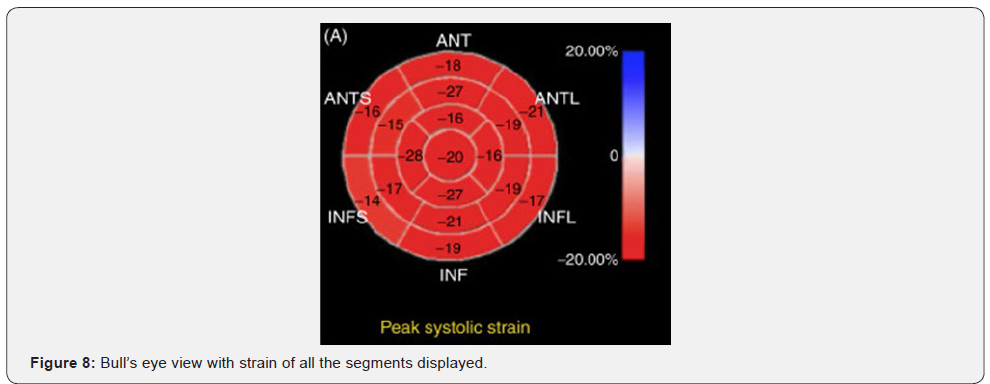
Image depth and frame rate (40-100) should be so set as to get an optimal view and Region of Interest (ROI) is over layed the 2-D image, encompassing the myocardium totally. Analysis can be done live or offline (by special software) and represented by graphs (Figure 7) and a bull’s-eye view (Figure 8) showing the strain values of individual segments with outer circle for basal segments, mid for middle segments and inner circle for apical segments.
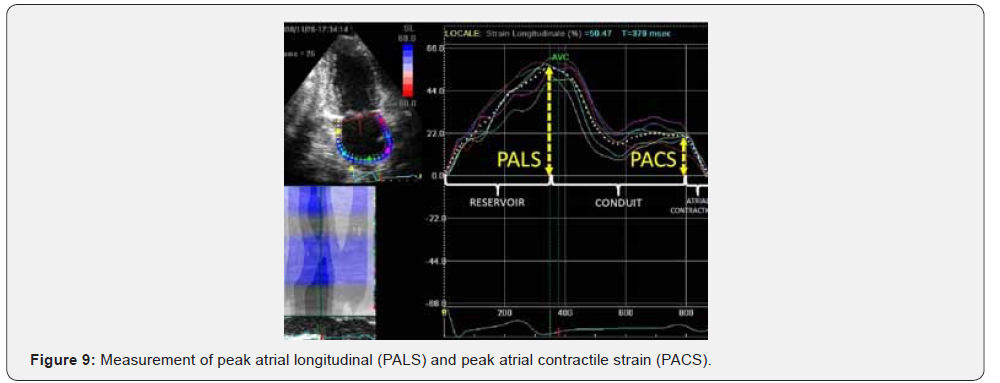
For LA strain acquisition, apical 4 and 2-chamber views are sufficient and a varied number of segments [6-12] are assessed although now total peak longitudinal and contractile strain values are recommended [8] as shown in Figure 9.
Mechanisms of LV dysfunction in hypertension
Hypertension leads to myocardial fibrosis (essentially deposition of type I Collagen), which causes decreased diastolic relaxation as tissues get stiff and later on systolic dysfunction ensues as myocytes are unable to translate contraction into force (9 and 10).
Normal myocardium comprises of myocytes (1/3 of cell), endothelial, vascular smooth muscle cells and fibroblasts which make up rest of the cells [11]. Extracellular matrix comprises of proteins and polysaccharides. Hypertension affects both the components, cellular and non-cellular causing hypertrophy of former and deposition of fibrous tissue in later [12].
This has been aptly demonstrated by Roman Querejeta et al. [13] in their study of 77 patients (34 hypertensives with heart failure, 31 with hypertension only and 12 controls) by correlating HTN, clinical HF, biochemical molecules of fibrosis and histopathology of mid interventricular septal muscle by endomyocardial biopsy. Cardiovascular fibrosis was significantly higher (p< 0.001) in HTN patients than control subjects more so (significantly high) in HTN with HF (7.95 ± 0.55% vs 5.38 ±0.31%; p< 0.001).
Extent of collagen deposition was significantly high in HTN group especially with HF. Further the synthesis of PIP (Propeptide of ProCollagen Type I) was significantly high in HTN group than control. They found a direct correlation level of PIP level in coronary sinus and peripheral vein with cardio-vascular fibrosis (coronary r = 0.759; p<0.001 and peripheral r = 0.867; p < 0.001). All these findings showed significant inverse correlation of EF with cardio-vascular fibrosis (r = -0.393; p < 0.001), coronary PIP (r = 0.387; p < 0.05) and peripheral PIP levels (r = 0.256; p < 0.05).
Mizuno et al. [14] found excellent correlation between the amount of fibrosis and integrated backscatter
It has been shown by Louis Antonio Moreno-Ruiz et al. [15]. that in hypertension, level of oxidized proteins and lipid oxidation
are enhanced and activity of antioxidants like superoxide dismutase, glutathione peroxidase and catalase decrease, causing increased oxidation stress which alters the cellular signaling pathway and modulation of growth, apoptosis, hypertrophy, inflammation and remodeling of cardiac muscle. This oxidation stress leads to accumulation of extracellular matrix, interstitial and perivascular fibrosis, and myocyte hypertrophy. All these changes lead to sub-clinical LV dysfunction as assessed by strain measurement in their study of 50 patients (25 HTN vs 25 controls). Both groups showed normal 2-D echo LVEF. They found a positive correlation between levels of oxidized proteins and GLS (r = 0.386; p = 0.006) and a negative correlation of extracellular superoxide dismutase with GLS (r = 0.404; p = 0.004) as the oxidative stress accentuates or gets prolonged, first diastolic dysfunction and later on deterioration in EF is noted.
Sub-clinical left ventricular dysfunction in hypertensive patients
Numerous studies are now available in literature, showing that in spite of preserved EF as assessed by 2-D echo, reduced strain values are seen when speckle tracking echocardiography is done. Shantanu P Sengupta et al. [16]. in their study of 59 subjects (34 HTN vs 25 control) assessed layered strain and found sub-endocardial and sub-epicardial regions showed reduced longitudinal strain, whereas circumferential strain was reduced in sub-epicardial region only, radial strain was no different in the two groups.
Xio-Xia Luo et al. [17] while comparing 40 youths (age range 18 ± 3 years) with masked hypertension and 40 age-matched normotensive controls found that longitudinal strain (subendocardial and mid-myocardial) along with circumferential strain was significantly reduced in hypertensive group (p < 0.05); no difference was noted with regard to radial strain and apical rotation. 2-D echo EF was normal in the two groups.
Reduction in GLS has been correlated with the pattern of LV geometry in hypertensive patients. Susana Goncalves et al. [18] in their study of 20 normotensive and 229 hypertensive patients found no difference in GLS between the two groups. However, hypertensive group showed 15.3% of the subjects to have reduced GLS and the pattern of reduction correlated with LV geometrical pattern. Concentric remodeled type showed the least drop in strain value and concentric hypertrophy showed the most. In another study, Ting-Yan Xu et al. [19] showed the pattern of strain in the four geometrical types of LV in hypertensive patients. Longitudinal strain was reduced significantly in all types of geometrical patters in all the layers except for normal geometrical pattern (all three layers), mid and epicardial layers in concentrically remodeled pattern in which the drop was not significant. Circumferential strain was increased for sub-endocardial and mid wall in normal geometrical patters and in subendocardial strain in concentrically remodeled pattern. For other layers in these two geometrical patterns it was non-significantly increased. However, it was significantly reduced for all the layers in concentrically hypertrophic and eccentrically hypertrophic types of geometrical patterns. Radial strain did not show any difference for any type of geometrical pattern and for any layer.
Reduction in GLS, as a marker of sub-clinical LV dysfunction in hypertensive patients, has been detected not only during rest but also with exercise. Kai O Hansel et al. [20], in their study of 92 patients (46 HTN vs 46 control) found that both at rest and after exercise, the strain values were lower significantly in HTN subjects. Brain natriuretic peptide (BNP), along with its fragment N-terminal B type Natriuretic Peptide (NT-Pro BNP) is released by myocytes when put on a stretch. These are usually elevated in patients with LVH, thus relating to cardiac remodeling and diastolic dysfunction. Waleed Abdou Ibrahim Hamed et al. [21] in their study of 106 patients (80 HTN vs 26 control) showing normal EF by 2-D echo, found a negative correlation between BNP level and global peak systolic strain, global systolic strain rate, early and late diastolic strain rate in HTN patients with significantly increased BNP levels as compared to control subjects.
Sadiya S Khan et al. [22] in HYPERGEN study (2058 participants) found that LS, e’ velocity and early diastolic strain rate were heritable traits whereas no such association was noted with GCS and GRS.
Sub-clinical left atrial dysfunction in hypertensive patients
Left atrium not only acts as a reservoir and conduit of blood transfer to LV but also contributes (25-30%) of LV cardiac output by virtue of its contractile function. Speckle tracking echocardiography can detect deterioration in various LA parameters in HTN patients much before any change in its size or parameters of diastolic LV function could be noted. This has been shown by Bassam Hennawy et al. [23] in their study of 100 subjects (50 HTN vs 50 control) that global peak atrial longitudinal strain was significantly reduced in hypertensive patients (41.36 ± 2.86 vs 24.00 ± 6.92 p = 0.00).
Hypertension is a leading cause of atrial fibrillation and this especially happens when LA gets enlarged and shows fibrosis in its wall. Atrial fibrillation by itself has got many adverse sequelae. Parameters were searched to detect its potential of occurrence much before any change in LA size or function happens. Ioana Petra et al. [24], in their study of 108 patients (67 with HTN only vs 41 with HTN and one episode of recent AF) found that although both groups showed normal LVEF but PALS and PACS showed good discriminatory capacity as predictors of AF (AUC = 0.88 for PALS and AUC = 0.86 for PACS).
Conclusion
Speckle tracking echocardiography as an emerging tool for the assessment of left ventricular and left atrial function has clearly demonstrated its utility in the detection of sub-clinical dysfunction of these chambers, much before the conventional methods can detect it. Because of its ease of availability, angle independency, robustness and provision of off-line assessment, this modality need be incorporated in every echocardiographic study especially when dealing with hypertensive patients in view of the nearly epidemic prevalence of this clinical entity.
Acknowledgement
Thanks to Ms Huffsa Imran for typing and proofreading the manuscript.
References
- Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, et al. (2005) Global burden of hypertension: analysis of worldwide data. Lancet 365(9455): 217-223.
- Lloyd-James DM, Larson MG, Leip EP, Beiser A, D'Agostino RB, et al. (2002) Lifetime risk for developing congestive heart failure. The Framingham Heart Study. Circulation 106(24): 3068-3072.
- Hameed I (2019) Transthoracic echocardiographic chamber quantification in the light of current guidelines. Pak Heart J 52(2): 100-116.
- Satoru Kishi (2016) Article based on Eizojoho Medical Magazine 48: 14.
- Mondillo S, Galderisi M, Mele D, Cameli M, Lomoriello VS, et al. (2011) Speckle-Tracking Echocardiography A New Technique for Assessing Myocardial Function. J Ultrasound Med 30(1): 71-83.
- Moreira HT, Nwabuo CC, Armstrong AC, Kishi S, Gjesdal O, et al. (2017) Reference Ranges and Regional Patterns of Left Ventricular Strain and Strain Rate UsingTwo-Dimensional Speckle-Tracking Echocardiography in a Healthy Middle-Aged Black and White Population: The CARDIA Study. J Am Soc Echocardiogr 30(7): 647-658.
- Jarasunas J, Aidietis A, Aidetiene S (2018) Left atrial strain - an earaly marker of left ventricular diastolic dysfunction in patients with hypertension and paroxysmal atrial fibriallation. Cardiovasc Ultrasound 16(1): 29.
- Cameli M, Lisi M, Righini FM, Benincasa S, Solari M, et al. (2013) Left atrial strain in patients with arterial hypertension. International Cardiovascular Forum Journal 1: 31-36.
- Schumann CL, Jaeger NR, Kramer CM (2019) Recent advances in imaging of hypertensive heart disease. Curr Hypertens Rep 21(1): 3.
- Diez J, Gonzalez A, Lopez B, Querejeta R (2005) Mechanism of disease: pathologic structural remodeling is more than adaptive hypertrophy in hypertensive hear disease. Nat Clin Pract Cardiovasc Med 2(4): 209-216.
- Weber KT (2000) Fibrosis and hypertensive heart disease. Curr Opin Cardiol 15(4): 264-272.
- Shahnaz AU, Sun Y, Bhattacharya SK, Ahkas RA, Gerling IC, et al. (2010) Fibrosis in hypertensive heart disease: molecular pathways and cardioprotective strategies. J Hypertens 28(Suppl 1): S25-S32.
- Querejeta R, López B, González A, Sánchez E, Larman M, et al. (2004) Increased Collagen Type I Synthesis in Patients With Heart Failure of Hypertensive Origin, Relation to Myocardial Fibrosis. Circulation 110(10): 1263-1268.
- Mizuno R, Fujimoto S, Saito Y, Nakamura S (2007) Non-invasive quantitation of myocardial fibrosis using combined tissue harmonic imaging and integrated backscatter analysis in dilated cardiomyopathy. Cardiology 108(1): 11-17.
- Moreno-Ruiz LA, Ibarra-Quevedo D, Rodriguez-Martinez E, Maldonado PD, Benito Sarabia-Ortega, et al. (2015) Oxidative stress state is associated with left ventricular mechanics changes, measured by speckle tracking in essential hypertensive patients. Oxidative Medicine and Cellular Longevity p. 8.
- Sengupta SP, Caracciolo G, Thompson C, Abe H, Sengupta PP (2013) Early impairment of left ventricular function in patients with systemic hypertension: new insights with 2-dimensional speckle tracking echocardiography. Indian Heart Journal 65(1): 48-52.
- Luo XX, Zhu Y, Sun Y, Ge Q, Su J, et al. (2018) Does masked hypertension cause early left ventricular impairment in youth. Frontiers Pediatr 6: 167.
- Gonçalves S, Cortez-Dias N, Nunes A, Belo A, Zimbarra Cabrita I, et al. (2014) Left ventricular systolic dysfunction detected by speckle tracking in hypertensive patients with preserved ejection fraction. Rev Port Cardiol 33(1): 27-37.
- Xu TY, Yang Y, Li JJ, Li Y, Wang JG (2019) Left ventricular deformation in relation to the geometric pattern in hypertensive patients. Medicine 98(4): e14257.
- Hensel KO, Jenke A, Leischik R (2014) Speckle-tracking and tissue-doppler stress echocardiography in arterial hypertension: a sensitive tool for detection of subclinical LV impairment. Biomed Res Int 472562.
- Ibrahim Hamed WA, Mostafa Kamal A, Noamany MF, Soliman MA, Mohammed Abdel Ra’ouf M (2014) Evaluation of left ventricular performance in hypertensive patients by speckle tracking echocardiography: correlation with brain natriuretic peptide. The Egyptian Heart Journal 66(4): 299-308.
- Khan SS, Kim KA, Peng J, Aguilar FG, Selvaraj S, et al. (2019) Clinical correlates and heritability of cardiac mechanics: the hyperGEN study. Int J Cardiol 274: 208-213.
- Hennawy B, El Kilany W, Galal H, Mamdouh A (2018) Role of speckle tracking echocardiography in detecting early left atrial dysfunction in hypertensive patients. Egyptian Heart J 70(3): 217-223.
- Petre I, Onciul S, Iancovici S, Zamfir D, Stoian M, et al. (2019) Left atrial strain for predicting atrial fibrillation onset in hypertensive patients. High Blood Press Cardiovasc Prev 26(4): 331-337.






























