Daidzein- A Caveolin Inhibitor Exerts Antihypertensive Effect and Improves Endothelium-Dependent Vasorelaxation in a Rat Model of DOCA-Salt-Induced Hypertension
Shalini Jamwal1* and Saurabh Sharma2
1 Department of Pharmacology, Abhilashi University, India
2Department of Pharmacology, CT University, India
Submission: Augsut 22, 2019; Published: September 26, 2019
*Corresponding author: Shalini Jamwal, Department of Pharmacology, School of Pharmacy, Abhilashi University, Mandi (H.P), India
How to cite this article:Shalini J, Saurabh S. Daidzein- A Caveolin Inhibitor Exerts Antihypertensive Effect and Improves Endothelium-Dependent Vasorelaxation in a Rat Model of DOCA-Salt-Induced Hypertension. J Cardiol & Cardiovasc Ther. 2019; 15(1): 555905. DOI: 10.19080/JOCCT.2019.15.555905
Abstract
Daidzein- A caveolin inhibitor has antioxidant properties that could improve redox-sensitive vascular, cardiac and renal changes associated with deoxycorticosterone acetate/1% NaCl high salt (DOCA/HS)-induced hypertension. We investigated the possible involvement of caveolin and daidzein its inhibitor in hypertension and endothelial dysfunction in a mineralocorticoid-salt mouse model (DOCA-Salt). Hypertension was induced in sham control mice by nephrectomy and deoxycorticosterone acetate (DOCA)-salt treatment for 6-weeks. (Control uninephrectomized mice drank 1% NaCl water). Nephrectomy + DOCA (40mg/kg, s.c: 6 weeks) administration increased mean arterial blood pressure in rats after 6 weeks as compared to normal control group. VED was assessed in terms of decreased serum nitrite/nitrate conc., reduced glutathione levels, ACh-induced endothelium-dependent vasorelaxation, and SNP-induced endothelium-independent Vasorelaxation. These rats received cotreatment of different doses of daidzein (0.2, 0.4mg/kg/day, sac) for 5 weeks. Daidzein (0.2mg/kg/day., and 0.4 mg/kg/day., sac for 1 week) and lisinopril 1mg/kg., p.o., 1 week) treatment for one week significantly ameliorated VED in hypertensive rats measured in terms of decreased reduced glutathione level, serum nitrite/nitrate conc. increased Ach-induced endothelium-dependent vasorelaxation as compared to the hypertensive group. However, sodium nitroprusside did not produce any change in SNP-induced endothelium-independent vasorelaxation that shows that effect is specifically due to the improvement of endothelium dysfunction. Our results demonstrate that daidzein reduces oxidative stress, prevents development and progression of hypertension as well as cardiac and renal hypertrophy in DOCA/HS-induced hypertension via modulation of activated eNOS, endogenous antioxidants, serum NO.
Keywords: Vascular endothelial dysfunction; Hypertension; Doca-Salt; Nitric oxide; Caveolin; Endothelium
Introduction
Hypertension is a most prominent risk factor for heart disease, ischaemic stroke, and other cardiovascular diseases, resulting in significant morbidity, mortality and financial burden globally [1]. Hypertension has been associated with vascular reactivity impairment to relaxant agents. In several models of experimental hypertension, the NO-dependent relaxation is reduced. Impaired relaxation to NO, both endothelium-dependent [2] and endothelium-independent [3] has been observed in arteries from renovascular hypertensive rats. This impairment has been attributed to several factors such as endothelial dysfunction by decreased NO release and/or endothelium-derived hyperpolarizing factor [4] increased production of superoxide anions [5] and alterations in the membrane potential of VSMCs.
In healthy human subjects, inhibition of NO synthase by N-monomethyl-L-arginine acutely increased Blood pressure, peripheral vascular resistance, and fractional excretion of Na+. Hypertension is associated with an impaired endothelial function that includes reduced production and/or NO release. The NO production is regulated by eNOS activation in response to the increase of [Ca2+], phosphorylation, dimerization of proteins and protein interactions have been reported that caveolin directly binds to eNOS, thereby regulating the NO production [6]. Caveolae are abundant in the endothelial cells where they regulate endothelial NO-synthase (eNOS) and NO production by interaction with caveolin-1, the structural caveolae protein [7]. Endothelial Cells (EC) are thought to have one of the highest levels of caveolin-1. One of the major functions of endothelial cells is to maintain vascular tone and structure; in addition, endothelial cell layer forms an important interface between circulating blood and vascular smooth muscle cells. Several proteins residing in or recruited to caveolae serve as regulators of eNOS. Some of the proteins that modulate the eNOS activity include caveolin-1, Heat Shock Protein (HSP) 90, cationic amino acid transporter 1 (arginine transporter), Ca2+- calmodulin, and ion channels, Ca2+ pump, sGC, and bradykinin B2 receptor, VEGF receptor 2 and others [7]. eNOS appears to be associated with caveolin, which precludes calmodulin binding to the enzyme. Binding of Calmodulin simultaneously disrupts the inhibitory caveolin-eNOS interaction. The ability of calmodulin to activate eNOS is inhibited by CK2 kinase, a mechanism thought to lead to selective disassociation of phosphorylated calmodulin from eNOS eNOS dissociates from caveolin-1, calcium-calmodulin complex (CAM) binds to ENOS, and electron transport is restored, as is NO production. Caveolin topically inhibits eNOS in quiescent cells both by impeding the signaling of caveolae-targeted receptors that transduce eNOS-stimulatory signals as well as by sterically blocking the calmodulin binding site in eNOS. In the endothelium, caveolin-1 negatively regulates NO signaling by binding to eNOS. The activation of caveolar eNOS depends on its dissociation from caveolin-1. In response to various stimuli such as VEGF and shear stress, eNOS binds to HSP90 which facilitates calmodulininduced displacement of caveolin-1 from eNOS [8]. However, the interrelationship of caveolin-1 and eNOS is a dynamic one. For example, caveolin-1 is crucial for agonist-induced eNOS activation. Thus, the aim of this study was to demonstrate daidzein a caveolin inhibitor may have beneficial actions on NO activity and perhaps have the potential to selectively improve hypertension and its associated vascular complications.
Material and Methods
Experimental animals
Wistar albino rats weighing 125–175g (8-10-week-old) purchased from animal house, I.S.F College of Pharmacy, Moga, Punjab, were employed in the present study. They were housed in an air-conditioned room and were kept in standard laboratory conditions under natural light and dark cycles (approximately 14 h light/10h dark) and humidity 60±5% and temperature of 25 ± 3°C in the departmental animal house. The animals were allowed free access of standard diet (24% protein, 5% fat, 4% fiber, 55% carbohydrates, 0.6% calcium, 0.4% phosphorous, 7% moisture and 4% ash w/w) and tap water ad libitum and allowed to acclimatize for 2 weeks before starting the experiments. The experimental protocol was approved by the Institutional Animal Ethics (IAEC) and conformed to the Indian National Science Academy (INSA) Guidelines for the use and care of experimental animals in research.
Drugs and chemicals
Daidzein was purchased from MedChi Express LLC chemicals and DOCA from Sigma-Aldrich. Other chemicals and biochemical reagents of analytical grade were used freshly.
Doca- salt induced hypertension
DOCA- Salt-induced hypertension is due to the sodiumretaining properties of the steroid causing increases in plasma and extracellular volume. The hypertensive effect is increased by salt loading and unilateral nephrectomy in rats. Wistar Albino rat (125-175g) were anesthetized with Ketamine (70mg/kg, i.e.) and xylazine (5mg/kg, i.e.) through a flank incision, the left kidney was removed. The rats were injected twice weekly with 40mg/kg, s.c. deoxycorticosterone-acetate in olive oil for 6 weeks. Drinking water is replaced with a 1% NaCl solution. Blood pressure starts to rise after one week and reaches Mean arterial blood pressure value between 160- and 190mm Hg after 6 Week.
Experimental protocol (Each Group N=6):
Group I Normal control: Rats were maintained on normal chow diet with drinking water. Group 11 Hypertensive control: Rats were uninephrectomized and DOCA Salt was administered twice weekly for 6 weeks and drinking water replaced with 1% NaCl solution. Group III Hypertensive rats were treated with Daidzein (0.2mg/kg/day, s.c) for the 1st week started from the 5th week of DOCA Salt administration. Group IV Hypertensive rats were treated with Daidzein (0.4mg/kg/day, s.c) for last week started from the 5th week of DOCA Salt administration. Group V Hypertensive rats were treated with Lisinopril (1mg/kg/day, pp.) for the 1st week started from the 5th week of DOCA Salt administration.
Isolated aortic ring preparation (Each group n=6) wire myograph
Group VI HT (Isolated aortic ring preparation) + Daidzein(2μm/l). Group VII HT (Isolated aortic ring preparation) + Daidzein(2μm/l) + L-NAME (10μm/l). Group VII HT (Isolated aortic ring preparation) + Daidzein(2μm/l) + Glibenclamide (5μm/l)
Assessment of Hypertension
Assessment of mean arterial blood pressure
The rat blood pressure was measured by Tail cuff method (NIBP-BIOPACK MP 100, USA). Rat tail was heated with the exact time of 3 minutes after that tail was inserted into the cuff, the pressure was applied with cut off pressure of 250mmHg and mean arterial blood pressure was recorded by Data Acquisition System (BIOPAC).
Assessment of Oxidative Stress
Reduced glutathione (GSH)
To measure reduced glutathione level, aortic tissue homogenate (in 0.1 M phosphate buffer Ph 7.4) was taken. The procedure was followed initially as described by Ellman, 1959. The homogenated was added with an equal volume of 20% Trichloroacetic Acid (TCA) containing 1mm EDTA to precipitate the tissue proteins. The mixture was followed to stand for 5min prior to centrifugation for 10min at 200 rpm. The supernatant (200μl) was then transferred to a new set of the test tube and added 1.8ml of the Ellman reagent (5,5`-dithio bis-2-nitrobenzoic acid) (0.1mm) was prepared in 0.3M phosphate buffer with 1% of sodium citrate solution. Volume was made up to 2ml of all the test tubes. After the completion of the total reaction, the solution was measured at 412nm against blank. Absorbance values were compared with a standard curve generated from a standard curve from known GSH. The level of GSH was expressed as μmol/mg of Aortic wt [9].
Serum nitrite/nitrate level using greiss reagent
Serum nitrite/nitrate was estimated using Greiss reagent which served as an indicator of nitric oxide production. 400μl of carbonate buffer (Ph 9.0) was added to 100μl of serum sample followed by addition of small amount (˜0.15g) of the coppercadmium alloy. The tubes were incubated at room temperature for 1 hour to reduce nitrate to nitrite. The reaction was stopped by adding 100μl of 0.35M sodium hydroxide following this, 400μl of zinc sulfate solution (120mm) was added deproteinate the serum samples, the samples were allowed to stand for 10min and then centrifuged at 4000g for 10min. Greiss reagent (250μl of 1.0% sulphanilamide and 250μl of 0.1% napthaylaminediaminedihydrochloric acid in water) was added to aliquots (500μl) of clear supernatant and serum nitrite/nitrate was measured spectrophotometrically at 545nm. The standard curve of sodium nitrite was plotted and expressed as μmol/l [10].
Estimation of tumor necrosis factor –alpha (TNF-α) levels
TNF- α level was estimated by using rat TNF-a kit (RayBio, Rat TNF-alpha ELISA kit protocol) which uses a microtitre plate reader read at 450nm. Concentrations of TNF-α were calculated from the plotted standard curve.
Principle
This assay employs the quantitative sandwich enzyme immunoassay technique. An affinity polyclonal antibody specific for mouse TNF-α has been precoated onto a microplate. Standards, controls, and samples are pipettes into wells and any rat TNF-a present is bound by the immobilized antibody. After washing away any unbound substances, an enzyme-linked polyclonal antibody specific for rat TNF- GSK-3β level was estimated by using a rat. TNF- α is added to the wells. Following a wash to remove any unbound antibody-enzyme reagent, a substrate solution is added to the wells. The enzyme reaction yields a blue product that turns yellow when the stop solution is added. The intensity of the color measured is in proportion to the amount of rat TNF-a bound in the initial step. The sample values are then read off the standard curve [11].
Vasoreactivity
Ach and SNP induced vasorelaxation
Isolated rat aortic ring preparation: -The rats were sacrificed by cervical dislocation, followed by decapitation. Thoracic aorta was removed, cut into a ring of 4-5mm in length and mounted in an organ bath containing Krebs- henseleit solution (NaCl,119Mm, Kcl,4.7mm; KH2PO4.1.2Mm and CaCl2,2.5 Mm) of PH 7.4, bubbled with carbonated oxygen ( 95% O2 and 5% CO2 ) and maintained at 37ºC. The preparation was allowed to equilibrate for 90min under 1.5g tension. The isometric contractions were recorded with a force transducer (Ft-2040) connected to a physiograph (INCO, Ambala, India) the aortic ring preparation was primed with 80mm KCL to check its functional integrity and to improve its contractility. The cumulative dose response of Ach (10-8 to 10-4 M) or sodium nitroprusside SNP (10-8to 10-4M) were recorded in phenylephrine (3×10-6M) precontracted with intact or denuded endothelium, respectively [12].
Molecular Assays
Assessment of mRNA expression of eNOS
100mg of aortic tissue was homogenized in 1ml of triazole reagent and incubated for 5min at 20ºC. 0.2ml of chloroform was added to the homogenate, incubated at 20ºC for 3min. the mixture was centrifuged at 10,000g for 15min at 4ºC, the upper aqueous phase was isolated and 0.5ml isopropyl alcohol was added to precipitate RNA. The sample was centrifuged at 10,000g for 15min at 4ºC to form a gel-like pellet of RNA in the tube. The supernatant was removed, RNA pellet was washed with 75% ethanol, mixed, centrifuged at 7,500g for 5min at 4ºC and RNA pellet was briefly vacuum dried for 5-10min. The RNA was quantified by ultraviolet absorbance spectrophotometry to ascertain A260/A280 ratio<1.6 and dissolved in RNase-free water. The 5μl reverse primer was added to crude RNA, 29μl reverse transcriptase buffer incubated for 10min at 65ºC and cooled on ice. 16U AMV transcriptase (10U/ μl) and 5μl 10nM dNTP mixture were added, incubated at 42ºC for 1hr and 10mM Tris buffer (pH- 7.5) was added to synthesized single-stranded cDNA. 5μl cDNA product was mixed with 4μl dNTP mixture, 5μl forward primer, backward primer, 10 X amplification buffer, 0.9μl of Taq DNA polymerase enzyme (3U/μl) and 70.1μl RNase free water in PCR tube and overlaid with 100μl mineral oil. 24 PCR cycles of GAPDH (94ºC for 1min, 62ºC for 1min, 72ºC for 1min ) and 30 PCR cycles of eNOS (94ºC for 1min , 62ºC for 1min, 72ºC for 1 min) followed by 1 cycle at 57ºC for 2min and 72ºC for 7min were performed using 1 half of the reverse transcription mixture (Biorad, MJ Mini Thermal cycler), sense and antisense primers for eNOS: (5’-TCCAGAAACACAGACAGTGCA-3’ and 5’–CAGGAAGTAAGTGAGAGC -3’resp.) and for GAPDH (5’- TCCCTCAAGATTGTCAGCAA -3’ and 5’- AGATCCACAACGGATACATT -3’ resp. ) were used. The PCR products so obtained were analyzed on ethidium bromide-stained agarose (1.5%) gel on Gel electrophoresis apparatus (Biorad). The eNOS and GADPH products were quantified using the image (Gel Doc EZ image, Biorad) and the amount of eNOS was normalized with respect to the amount of GAPDH product [12].
Statistical Analysis
All values will be expressed as mean ± S.D. The data for aortic ring preparations were statistically analyzed using repeated measures of ANOVA followed by Newman-Keul` test. The data for aortic glutathione level, serum nitrate/nitrite level, mean arterial blood pressure (MABP) were statistically analyzed using oneway ANOVA followed by Tukey`s multiple comparison tests. The p-value <0.05 was considered to be statistically significant.
Results
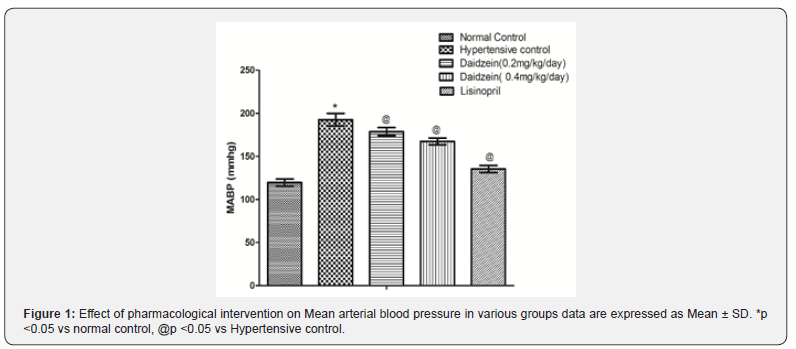
Effect of pharmacological interventions on mean arterial blood
Nephrectomy + DOCA salt-induced hypertension for six weeks has been noted to produce vascular endothelial dysfunction. Nephrectomy + DOCA administration increases mean arterial blood pressure (MABP) in rats after 5 weeks as compared to normal control group. Treatment with Daidzein (0.2mg/kg/ day, 0.4mg/kg/day, s.c) and lisinopril for the 1st week started from the 5th week of DOCA Salt administration significantly decreased mean arterial blood pressure (MABP) as compared to hypertensive rats (Figure 1).
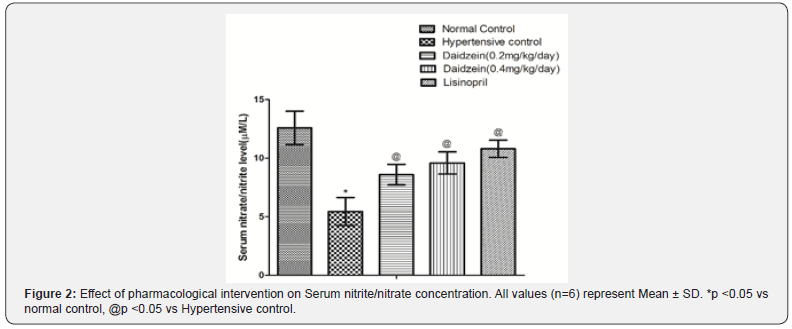
Effect of pharmacological interventions on serum nitrite/nitrate concentration
The serum concentration of nitrite/nitrate was noted to significantly reduced in Hypertensive control (DOCA, 40mg/kg”’, s.c.) as compared to normal control. Treatment with Daidzein (0.2mg/kg/day, 0.4mg/kg/day, s.c) and lisinopril for the 1st week started from the 5th week of DOCA Salt administration significantly increased the serum concentration of nitrite/nitrate as compared to hypertensive control (Figure 2).
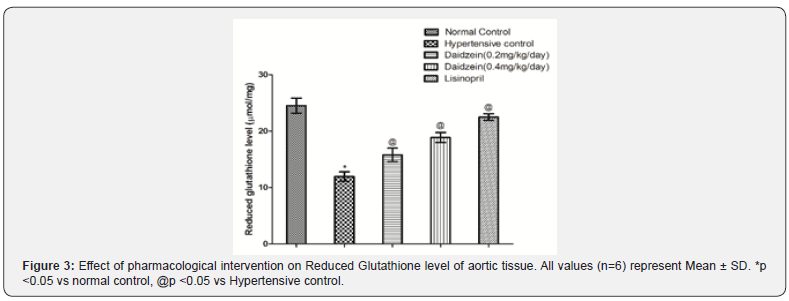
Effect of pharmacological Interventions on reduced glutathione level in thoracic aorta
Aortic GSH concentration was noted to significantly reduce in hypertensive control after 6 weeks in comparison to normal control rats. Treatment with Daidzein (0.2mg/kg/day, 0.4mg/kg/ day, s.c) and lisinopril for the 1st week started from the 5th week of DOCA Salt administration significantly increased the serum concentration of nitrite/nitrate as compared to hypertensive control (Figure 3).
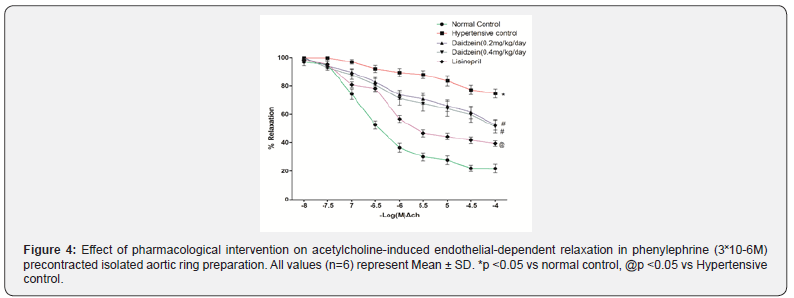
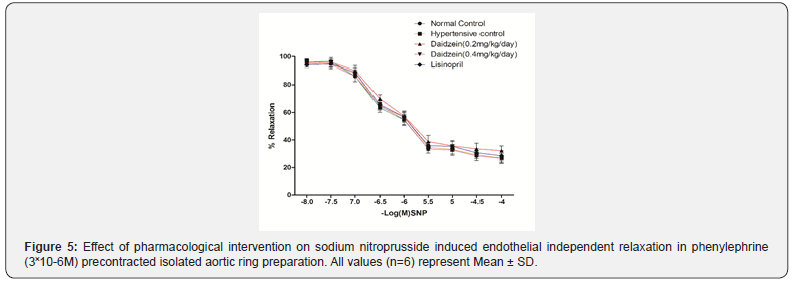
Effect of pharmacological interventions on endothelium-dependent and independent relaxation
Ach and SNP in a dose-dependent manner produced endothelium-dependent and independent relaxation in phenylephrine (3X10-6M) pre-contracted isolated rat aortic ring preparation. DOCA (40mg kg-1, s.c.) induced hypertension markedly attenuated Acetylcholine-induced endotheliumdependent relaxation but they did not affect SNP-induced endothelium-independent relaxation. Moreover, Daidzein (0.2mg/kg/day, 0.4mg/kg/day, s.c) and lisinopril for the 1st week started from the 5th week of DOCA Salt administration significantly prevented hypertension induced attenuation of Achinduced endothelium-dependent relaxation (Figure 4 & 5).
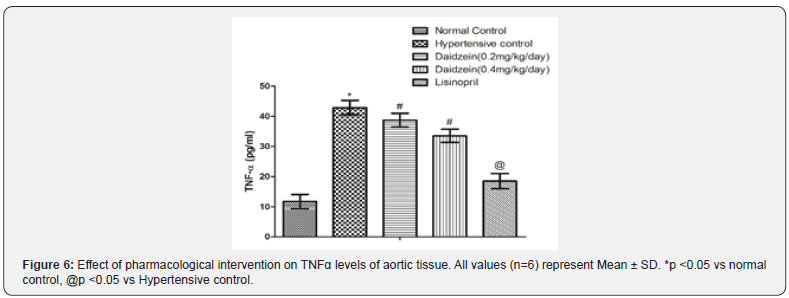
Effect of pharmacological interventions on TNFα levels
Administration of DOCA-Salt (40mg/kg, s.c.) for 6 weeks caused a significant increase in TNFα levels as compared to normal control rats. Treatment with Daidzein (0.2mg/kg/day, 0.4mg/kg/ day, s.c) and lisinopril for the 1st week started from the 5th week of DOCA Salt administration significantly reduced the TNFα levels as compared to hypertensive control (Figure 6).
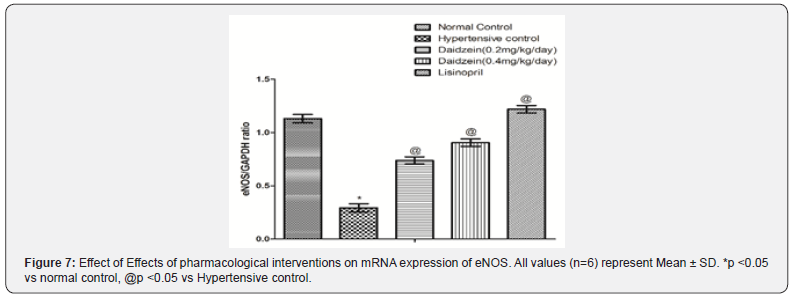
Effect of pharmacological interventions on mRNA expression of eNOS:
Administration of DOCA-Salt (40mg/kg, s.c.) for 6 weeks caused a significant significant decrease in expression ratio of eNOS/GAPDH as compared to normal control rats. Treatment with Daidzein (0.2mg/kg/day, 0.4mg/kg/day, s.c) and lisinopril for the 1st week started from the 5th week of DOCA Salt administration significantly reduced the TNFα levels as compared to hypertensive control (Figure 7).
Discussion
The major findings of our study are that blood pressure lowering effects of Daidzein are associated with increased activation of eNOS and increased serum NO levels. Hypertension is the most common cardiovascular disorder worldwide, and oxidative stress is a major contributor to the elevation of blood pressure and its complication [1-3,6]. Our findings, as well as previous studies, demonstrated that DOCA/HS administration in rats display many characteristics of hypertension including increased SBP, DBP, MBP, oxidative stress, and decreased serum NO levels and eNOS activation. Uninephrectomy + DOCA administration increased mean arterial blood pressure (MABP) in rats after 5 weeks as compared to normal control group.
Vascular endothelial dysfunction was assessed in terms of decreased serum nitrite/nitrate conc., reduced aortic glutathione levels, ACh-induced endothelium-independent vasorelaxation, and SNP-induced endothelium-independent vasorelaxation. The earlier results suggest that NO is, in fact, the most important endothelium-derived mediator involved in the Ach-induced relaxation of rat thoracic aortic rings. NO’s pivotal role in the Achinduced relaxation of the rat aorta has already been proposed [13]. Daidzein and lisinopril treatment for 1-week increase mRNA expression of eNOS, decrease in oxidative stress, TBARs, and inflammatory makers TNFα.
Hypertension is associated with an impaired endothelial function that includes reduced production and/or NO release. Endothelial NO synthase (eNOS) catalyzes the conversion of L-arginine to NO. For optimum activation, eNOS is targeted to caveolae. Although it is negatively regulated by caveolin. The NO production is regulated by eNOS activation in response to the increase of [Ca2+] phosphorylation, dimerization of proteins and protein interactions have been reported that caveolin directly binds to eNOS, thereby regulating the NO production. It has been proposed that following a rise in [Ca2+] in endothelial cells, eNOS dissociates from caveolin, allowing activation of this enzyme. Activation of eNOS implies its translocation after its dissociation from caveolin. The overexpression of caveolin impairs NO and Ca2+ signaling, causing a deficit in the endothelium-dependent vasorelaxation. In the pathogenesis of hypertension, the vasoactive peptide of the Renin-Angiotensin System (RAS), angiotensin II and its G Protein-Coupled Receptors GPCRs), play a crucial role by eliciting Reactive Oxygen Species (ROS) and mediating vessel contractility.
Lisinopril is used as the standard agent. Lisinopril belongs to a class called angiotensin-converting enzyme inhibitors, or ACE inhibitors. ACE inhibitors like lisinopril prevent the formation of angiotensin II. They do this by blocking the angiotensin-converting enzyme to convert Ang I to Ang II. They widen the blood vessels and help to reduce the amount of water put back into the blood by the kidneys which consequently reduce MABP in hypertensive rats.
Daidzein, is proposed to possess vasculoprotective properties. Daidzein enhances endothelium-dependent relaxation through an increase in NO synthesis due to an increase in activity or expression of endothelial nitric oxide synthase (eNOS). Daidzein and did not alter eNOS protein in endothelium-intact aortae but reduced expression of caveolin-1 and increased expression of calmodulin, that would account for an increase in eNOS activity.
Daidzein treatment selectively enhances endotheliumdependent relaxation in male rats through an increase in eNOS activity. The increase in eNOS activity is associated with a decreased expression of caveolin-1 and an increased expression of calmodulin in endothelial cells. Daidzein and lisinopril treatment for 1 week after 5 weeks administration of DOCA salt significantly ameliorate vascular endothelium dysfunction (VED) in hypertensive rats assessed in terms of increased reduced glutathione level, serum nitrite/nitrate conc. ACh-induced endothelium-dependent vasorelaxation as compared to the hypertensive group. However, no change in Sodium Nitroprusside (SNP) induced endothelium-independent vasorelaxation shows that effect is confined to endothelium.
Conclusion
In conclusion, we have demonstrated that chronic treatment with EO has a potential to prevent. Development and progression of hypertension associated vascular endothelial dysfunction. These effects are associated with activation of eNOS, improved serum NO levels. This study demonstrates daidzein have beneficial actions on NO activity and perhaps have the potential to selectively improve hypertension and its associated vascular complications.
References
- Weber MA (2014) Clinical practice guidelines for the management of hypertension in the community. The journal of clinical hypertension 16(1): 14-26.
- Callera GE, Yogi A, Tostes RC, Rossoni LV, Bendhack LM (2004) Ca2+-activated K+ channels underlying the impaired acetylcholine-induced vasodilation in 2K-1C hypertensive rats. J Pharmacol Exp Ther 309(3): 1036-1042.
- Rodrigues GJ, Restini CB, Lunardi CN, Moreira JE, Lima RG, et al. (2007) Caveolae dysfunction contributes to impaired relaxation induced by nitric oxide donor in aorta from renal hypertensive rats. J Pharmacol Exp Ther 323(3): 831-837.
- Mantelli L, Amerini S, Ledda F (1995) Roles of nitric oxide and endothelium-derived hyperpolarizing factor in vasorelaxant effect of acetylcholine as influenced by aging and hypertension. J Cardiovasc Pharmacol 25(4): 595-602.
- Heitzer T, Wenzel U, Hink U, Krollner D, Skatchkov M, et al. (1999) Increased NAD (P) H oxidase-mediated superoxide production in renovascular hypertension: evidence for an involvement of protein kinase C. Kidney Int 55(1): 252-260.
- Fleming I, Busse R (2003) Molecular mechanisms involved in the regulation of the endothelial nitric oxide synthase. American Journal of Physiology-Regulatory, Am J Physiol Regul Integr Comp Physiol 284(1): R1-R12.
- Frank PG, Woodman SE, Park DS, Lisanti MP (2003) Caveolin, caveolae, and endothelial cell function Arterioscler Thromb Vasc Biol 23(7): 1161-1168.
- Gratton JP, Fontana J, O'Connor DS, Garcia-Cardena G, McCabe TJ (2000) Reconstitution of an endothelial nitric-oxide synthase (eNOS), Hsp90, and caveolin-1 complex in vitro Evidence that Hsp90 facilitates calmodulin-stimulated displacement of eNOS from caveolin-1. J Biol Chem 275(29): 22268-22272.
- Sastry KV, Moudgal RP, Mohan J, Tyagi JS, Rao GS (2002) Tissue sulfhydryl groups. Arch Biochem Biophys 82(1): 70-77.
- Sastry KV, Moudgal RP, Mohan J, Tyagi JS, Rao GS (2002) Spectrophotometric determination of serum nitrite and nitrate by copper-cadmium alloy. Anal Biochem 306(1): 79-82.
- Khan SA, Onoue Y (1997) Neurotoxin production by a chloromonad Fibrocapsa japonica (Raphidophyceae). Oceanographic Literature Review 4(44): p. 345.
- Shah DI, Singh M (2007) Possible role of Akt to improve vascular endothelial dysfunction in diabetic and hyperhomocysteinemic rats. Mol Cell Biochem 295(1-2): 65-74.
- Vizioli EO, Spadin MD, Corrêa FM, Viaro F, Evora PR (2005) Acetylcholine-induced aortic relaxation studied in salbutamol treated rats. J Smooth Muscle Res 41(5): 271-281.






























