Giant Ascending Aortic Aneurysm Presented with Acute Onset Superior Vena Cava Syndrome
Jorge Alcocer*, Nikita Mehta, María Ascaso, Eduard Quintana and Manuel Castellá
Department of Cardiovascular Surgery, ICCV, Hospital Clínic, Barcelona, Spain
Submission: July 30, 2019; Published: August 13, 2019
*Corresponding author: Jorge Alcocer, Hospital Clinic, University of Barcelona, Calle Villarroel 170, ZC 08036, Barcelona, Spain
How to cite this article:Jorge Alcocer, Nikita Mehta, María Ascaso, Eduard Quintana, Manuel Castellá. Giant Ascending Aortic Aneurysm Presented with Acute Onset Superior Vena Cava Syndrome. J Cardiol & Cardiovasc Ther. 2019; 14(4): 555891. DOI: 10.19080/JOCCT.2019.14.555891
Abstract
We present a case of a 50 year-old-male patient with past history of tissue aortic valve replacement presented at the emergency department with chest pain and acute onset superior vena cava syndrome. After physical examination and CT aortic angiogram a giant ascending aortic aneurysm complicated with aorta to superior vena cava fistula was identified. The patient underwent emergent surgery consisting of aortic root replacement with mechanical valve- conduit and total arch replacement under hypothermic cardiopulmonary bypass. The patient had an uneventful postoperative recovery and was discharged at postoperative day 8. Postoperative CT aortic angiogram showed an excellent surgical result.
Keywords: Aortic aneurysm; Ascending aorta; Superior vena cava syndrome; Aorto-caval fistula; Chest pain
Abbrevations: CT: Computed Tomography; CPB: Cardiopulmonary Bypass; SVC: Superior Vena Cava; PA: Pulmonary Artery; Asc Ao: Ascending Aortic Graft; LCCA: Left Common Carotid Artery; BCA: Brachiocephalic Artery
Introduction
The ascending aorta is the second most common localization of degenerative aortic aneurysms after infrarenal abdominal aorta. They represent a life-threatening condition since they can complicate with acute type A aortic dissection or rupture. According to clinical guidelines they must be surgically repaired when asymptomatic with diameter greater than 55mm or when symptomatic regardless their diameter. Aneurysms associated with elastopathies should be repaired with lower diameter (45-55mm) [1]. Computed Tomography (CT) aortic angiography, magnetic resonance imaging and echocardiography represent the preferred diagnostic methods as they allow to detect aortic complications and to plan the best surgical approach.
Here, we report a patient with previous aortic valve replacement surgery and a giant ascending aortic aneurysm complicated with aorta to superior vena cava fistula. This is a very rare complication that has been previously described in association with syphilitic aortitis [2,3], acute aortic dissection [4] and aortic pseudoaneurysms [5] but infrequently associated to degenerative ascending aortic aneurysms.
Case Report
A 50 year-old-male was admitted in the emergency department due to acute onset chest pain and hypotension. Clinical examination was remarkable for upper body cyanosis, severe jugular vein distension and signs of low cardiac output. The patient was HIV seropositive due to past intravenous drug abuse and he had previous history of tissue aortic valve replacement for native bicuspid aortic valve endocarditis in 2011. Previous surgery was performed in an outside hospital and no follow-up data were available at the time of admission.
Chest-X-ray showed a huge mediastinal widening and transthoracic echocardiogram revealed a massively dilated aortic root and ascending aorta with normal functioning aortic bioprosthesis as well as good systolic function of both ventricles. A severe compression of the right atrium by the aortic aneurysm was also identified.
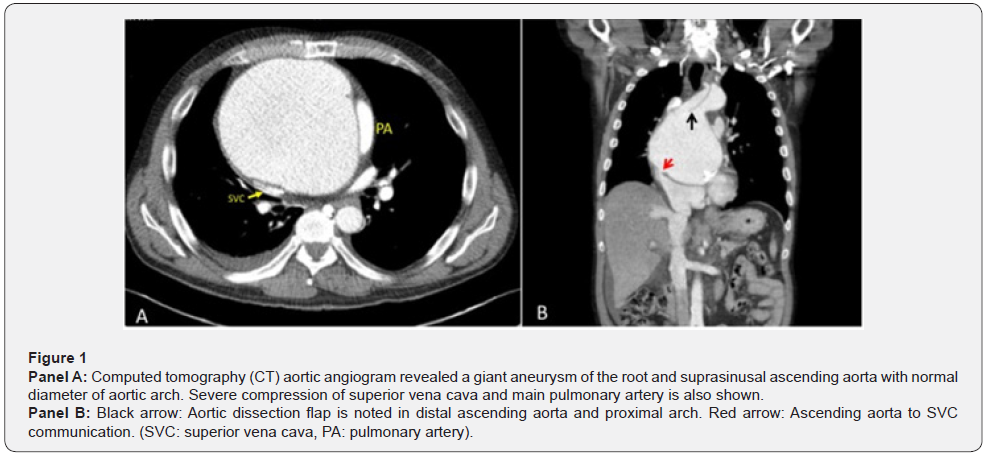
A CT aortic angiogram revealed a 14,7 x 13cm giant ascending aortic aneurysm (Figure 1, panel A) with a type A aortic dissection compressing the superior vena cava and right atrium. The CT also showed a fistula between the aneurysmal sac and superior vena cava (Figure 1, panel B, red and black arrows, respectively).
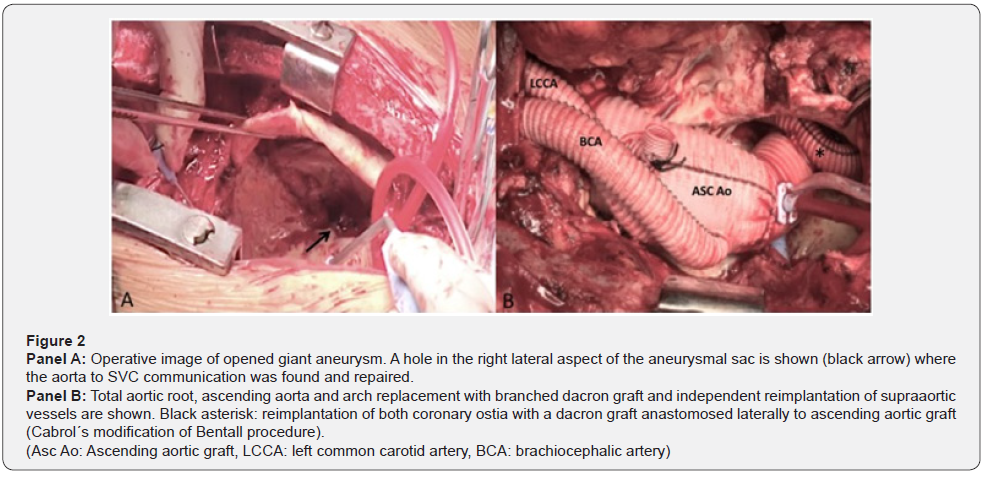
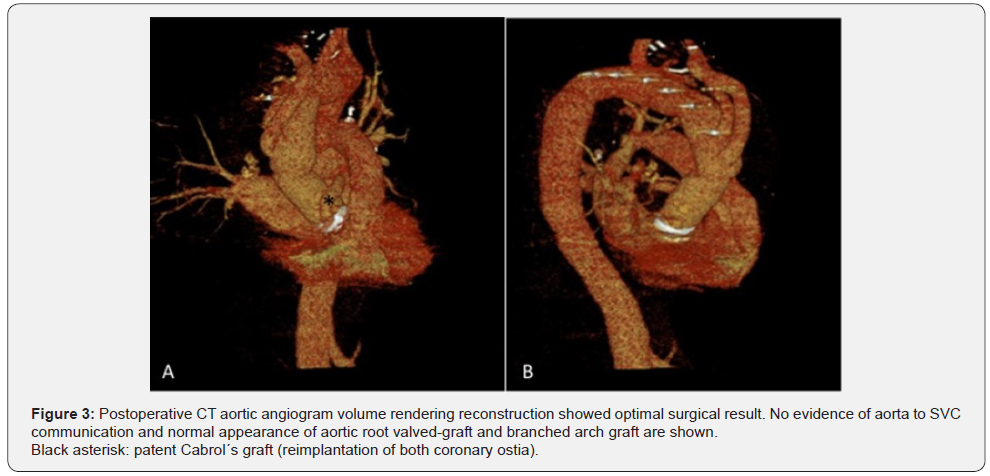
The patient underwent emergent surgery. Cardiopulmonary Bypass (CPB) was established after right axillary artery and right femoral vein cannulation. The re-sternotomy was performed under hypothermic CPB. Redo extensive aortic reconstruction was performed under deep hypothermic circulatory arrest with antegrade selective cerebral perfusion. Myocardial protection and cardiac standstill were obtained with selective antegrade intermittent cold blood cardioplegia. Once the aneurismal sac was incised, a communication between it and the superior vena cava was confirmed (Figure 2, panel A, black arrow) and was repaired with interrupted pledgeted 4/0 polypropilen sutures. After closing the fistula, an open distal anastomosis with a 30mm branched dacron graft was performed in arch zone 2 (just at the level of the origin of left common carotid artery). Both brachiocephalic trunk and left common carotid artery were independently reimplanted (Figure 2, panel B). Since the anastomotic site was slightly dilated, an elephant trunk technique was performed. After completion of arch replacement and supraaortic vessels reconstruction, systemic perfusion and rewarming were initiated. Proximally, the previous aortic bioprosthesis was resected and aortic root replacement was performed with 25mm mechanical valved conduit (Bentall procedure). The great dilatation and severe displacement of the aortic sinuses made coronary ostia mobilization impossible for independent reimplantation in the aortic root graft. Reimplantation of both ones with a separate 6mm dacron graft anastomosed laterally to the aortic graft was needed, according to Cabrol´s modification of Bentall procedure (Figure 2 & 3, black asterisk). The patient had an uneventful postoperative course and was discharged in postoperative day 8. Postoperative CT aortic angiogram confirmed the excellent surgical result (Figure 3, panel A & B). The patient is doing well and remains asymptomatic 6 month after surgery.
Discussion
Giant ascending aortic aneurysm, defined as an aneurysm with more than 10cm diameter, is a rare condition. There is a rapid increase in the risk of dissection or rupture when the aortic diameter is > 6cm for the ascending aorta and > 7cm for the descending aorta [1,6]. Most of the ascending aortic aneurysms are asymptomatic at the time of diagnosis. However, giant aneurysms are more frequently revealed by clinical signs of compression or erosion of adjacent structures such as superior vena cava as in this case, pulmonary artery, chest wall, oesophagus and trachea [7,8].
Superior Vena Cava (SVC) syndrome is the clinical presentation derived from stenosis or obstruction of superior vena cava. Head, face and upper body swelling is the most common sign, but clinical presentation can be variable depending on the velocity of instauration. In this case, the acute onset of chest pain, hypotension and upper body cyanosis suggest aneurysmal expansion with rupture to superior vena cava and aortocaval fistula formation. Sudden increase in central venous pressure and acute left to right shunt explain the rapid clinical presentation and the poor hemodynamic tolerance.
The most frequent cause of SVC syndrome is a thoracic malignancy (pulmonary and lymphoid neoplasms) while, nowadays, cardiovascular disease is very unusual [9]. It´s been previously published its association with thoracic aortic pathologies such as aortic dissection, aortic pseudoaneurysm, giant ascending aneurysm and previous cardiac surgery [10].
Ascending aortic aneurysms in the setting of syphilitic aortitis are inflammatory and often very large, therefore clinical presentation related to compression and erosion of adjacent structures are not uncommon in this clinical scenario. There are previous reports of syphilitic aortic aneurysms presenting with compression of surrounding structures as pulmonary artery, right atrium, superior vena cava and trachea [7,8]. Sekine et al. [2] reported SVC syndrome with aorta to superior vena cava fistula in a patient with syphilitic aortitis [2].
In this case, the giant ascending aneurysm is probably associated with bicuspid aortic valve aortopathy as this patient had previous history of aortic valve replacement for native bicuspid valve endocarditis. Moreover, pathologic analysis revealed a medial degeneration with loss of smooth muscle cells instead of endarteritis obliterans of adventitia, suggesting a connective tissue disorder more than syphilitic histology changes [11]. Serologic testing performed after surgery was negative in our patient. Although ascending aorta to superior vena cava fistula has been previously published in association with syphilitic aneurysm, our case is the first reported in a patient with bicuspid aortic valve related aneurysm.
The large size of the aneurysm, which was very close to the sternum, as well as the previous cardiac surgery made the surgical approach very challenging. Peripheral cannulation, establishment of cardiopulmonary bypass prior to chest opening and hypothermia play an important role in surgical approach of giant aortic aneurysms, especially in redo cases.
According to previously published similar cases, we decided to initiate cardiopulmonary bypass prior to sternotomy in order to decompress the aneurysm avoiding aortic injury during chest re-entry [12].
Conclusion
This case demonstrates the potential of giant ascending aortic aneurysms to cause superior vena cava syndrome and right heart failure in the acute setting. Although improvements in cardiovascular imaging and early detection of thoracic aortic pathologies have decrease the incidence of giant thoracic aneurysms, we have to consider aortic diseases as possible cause when a patient, especially with previous cardiac surgery, presents with this clinical conundrum.
References
- Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, et al. (2014) ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur H J 35(41): 2873-2926.
- Sekine Y, Yamamoto S, Fujikawa T, Oshima S, Ono, M, et al. (2015) Surgical repair for giant ascending aortic aneurysm to superior vena cava fistula with positive syphilitic test. Gen Thorac Cardiovasc Surg 63(10): 576-578.
- Phillips PL, Amberson JB, Libby DM (1981) Syphilitic aortic aneurysm presenting with the superior vena cava syndrome. Am J Med 71(1): 171-173.
- Fukui T, Ro D, Takanashi S (2010) Superior vena cava syndrome secondary to chronic dissecting aortic aneurysm after aortic valve replacement. Interact Cardiovasc Thorac Surg 11(2): 192-193.
- Vydt T, Coddens J, Wellens F (2005) Superior vena cava syndrome caused by pseudoaneurysm of the ascending aorta. Heart 91(4): e29.
- Elefteriades JA (2002) Natural history of thoracic aortic aneurysms: indications for surgery, and surgical versus nonsurgical risks. Ann Thorac Surg 74(5): S1877-S1880.
- Dayan V, Michelis V, Lorenzo A (2008) Giant Aortic Aneurysm as a Rare Cause of Superior Vena Cava Syndrome. Ann Thorac Surg 86(4): 1383.
- Lorusso R, Coletti G, Totaro P, Maroldi R, Zogno M (2000) Treatment of giant aortic aneurysm with tracheal compression and sternal erosion without circulatory arrest. Ann Thorac Surg 69(1): 275-278.
- Straka C, Ying J, Kong FM, Willey CD, Kaminski J, et al. (2016) Review of evolving etiologies, implications and treatment strategies for the superior vena cava syndrome. Springerplus 5: 229.
- Dedeilias P, Nenekidis I, Hountis P, Prokakis C, Dolou P, et al. (2010) Superior vena cava syndrome in a patient with previous cardiac surgery: what else should we suspect? Diagn Pathol 5: 43.
- Grewal N, Franken R, Mulder BJ, Goumans MJ, Lindeman JH, et al (2016) Histopathology of aortic complications in bicuspid aortic valve versus Marfan syndrome: relevance for therapy? Heart Vessels 31(5): 795-806.
- Srivastava V, AlHadid K, Saravanan P, Zacharias J, Bittar MN (2011) Giant aneurysm of the ascending aorta. BMJ Case Rep 2011: bcr1120103504.






























