Pulmonary Vascular Resistance (PVR) Late after Heart Transplant in Patients with Higher Preoperative Pulmonary Hypertension and Influence on Survival-A Study from India
Ratnagiri Ravi Kumar* and Prabhat Dutta
Department of Heart and Lung Transplantation, Gleneagles Global Hospital Chennai, India
Submission: January 18, 2019; Published: February 26, 2019
*Corresponding author: R Ravi Kumar, Department of Heart and Lung Transplantation. Gleneagles Global Hospital, 439, Cheran Nagar, Chennai, India J
How to cite this article: Ratnagiri R K, Prabhat D. Pulmonary Vascular Resistance (PVR) Late after Heart Transplant in Patients with Higher Preoperative Pulmonary Hypertension and Influence on Survival-A Study from India. J Cardiol & Cardiovasc Ther. 2019; 13(1): 555855. DOI: 10.19080/JOCCT.2019.13.555855
Keywords: Pulmonary vascular resistance; Pulmonary hypertension; Pulmonary compliance; Pulmonary heamodynamic; Heart transplantation; Right heart failure
Introduction
The Impact of Higher pre-operative Pulmonary vascular resistance and persistent Post-operative Pulmonary Arterial Hypertension (PAH) or pulmonary Compliance (Pca) on the Early Mortality or late Morbidity and Survival after a Successful Heart Transplantation is not well defined.
Methods
We studied 12 Patients who underwent Successful heart Transplant with High Pre-operative Pulmonary pressures – defined as PA systolic pressure more than 50 mm Hg but with Transpulmonary Gradient less than 16 mm hg after Vasodilator testing, for analysis of Pulmonary heamodynamic parameters like Pulmonary Vascular Resistance, (PVR) and Pulmonary Compliance(Pca) early (one month) and one Year after Heart Transplantation along with Survival at 6 months and one year. These 12 patients were statistically compared with 25 patients who had preoperative PA systolic pressures less than 50mm hg 11 of above patients were on both Sildenefil and Ambrisentan for PAH [1].
Results
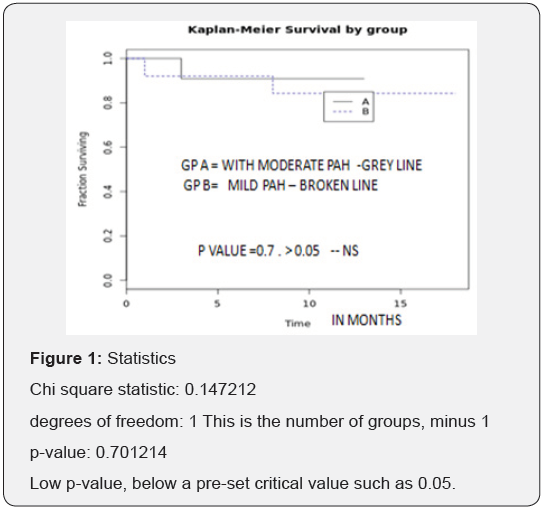
Age range was, Females = 1, Males = 17, Mean CPB time in These high PAH patients = 140 minutes, Mean Preoperative PA Systolic pressures = 58.80 mm (78-50 mm hg), Mean Pre-operative PVR = 4.1 wood units, Mean preoperative PA compliance = 1.02 (1.47-0.79). At three Months Mean PA Sytolic pressures = 38 MM HG, mean PVR =3.5 WU, Mean PA compliance =0.9. Of the 8 patients who completed 1 year of study, Mean PA systolic pressures = 35 MM HG, mean PVR = 3.5, Mean PA compliance = 0.85 UNITS. 87% of the Total patients were alive at 1 year. 93 % of the High PAH group were alive at 6 months after Transplantation [2,3]. There was No incidence of Clinical RV failure after Heart Transplant. There was 1 early Mortality related to Sepsis. Kaplan Meier analysis showed No difference in event free survival between the High PVR and Normal PVR group (p value = 0.7; NS) [4,5] Figure 1.
Conclusion
The main finding of our study was the ability of RRI to predict CI-AKI with a high level of sensitivity and specificity at an early stage after cardiac catheterization, which is within the first 24 hours following cardiac catheterization. This parameter outperformed conventional serum creatinine, which rise was shown to be delayed after the procedure.
The overall occurrence of CI-AKI in the development set of Mehran risk score for patients undergoing PCI was 13.1%.10 In our study subjects; the incidence of AKI was 19%, with 2% requiring dialysis and mean value of Mehran risk score in our study subjects was 7.5. These results are comparable with Mehran study.
Pathophysiology of CI-AKI and its link to renal resistive index.
Renal vasoconstriction resulting in medullary hypoxia, possibly mediated by alterations in nitric oxide, endothelin, or adenosine is considered to play a significant role in the pathogenesis of CI- AKI [12,13]. RRI can be used for assessing these renal perfusion changes, which only subsequently results in accumulation of serum Creat and overt CI-AKI. The RRI has recently been suggested for assessing changes in renal perfusion in post TAVI setting,7 cardiac surgery patients8 and in critically ill patients admitted to the intensive care unit [14-16].
Post procedural RRI and contrast induced AKI
In present study the post procedural RRI threshold of >0.744 achieved 94% sensitivity and 92% specificity closely matching values found in similar studies which investigated potential role of RRI in predicting AKI. Reviewing recently published studies, there is an interesting work presented by Bossard et al. [8], who studied 65 patients after cardiac bypass graft surgery with risk factors for AKI and indicated that in the immediate postoperative period RRI value >0.74 predicted the occurrence of delayed AKI with a sensitivity of 85 % and a specificity of 94%. Moreover, in a study of 51 critically ill patients hospitalized in an intensive care unit, Darmon et al. [15] showed that RRI >0.795 identified patients with persistent AKI (>3 days) with a sensitivity of 92% and a specificity of 85 %, in line with these results, Sinning et al. [7] studied 132 high risk subjects undergoing TAVI and indicated that RRI > 0.85 predicted post interventional AKI with a sensitivity of 58% and specificity of 86%. This high RRI threshold in contrast to our study might be explained by significantly higher mean subject age in this study (80.9±6.6 years) in comparative to our study mean age (57.6±8 years). Hence, our data closely match those of published literature, supporting the use of a threshold value of RRI >0.74-0.85 in predicting AKI in different clinical scenarios.
Clinical Implications
Based on our analysis, RRI allows the diagnosis of CI-AKI to be anticipated by few days. Routine evaluation of RRI in subjects at risk of CI- AKI could encourage clinicians to increase duration and frequency of conventional renal markers monitoring and to maximize renal-sparing actions. Such a prompt response to CIAKI would not be possible if the therapeutic strategy is based on delayed criteria, such as the increase in serum creat.
References
- Lindelöw B, Andersson B, Waagstein F, Bergh CH (1999) High and low pulmonary vascular resistance in heart transplant candidates. European Heart Journal 20: 148-156.
- Ghio S, Crimi G, Pica S, Temporelli PL, Boffini M, et al. (2017) Persistent abnormalities in pulmonary arterial compliance after heart transplantation in patients with combined post-capillary and precapillary pulmonary hypertension. PLoS One 12(11): e0188383.
- De Santo LS, Romano G, Maiello C, Buonocore M, Cefarelli M, et al. (2012) Pulmonary artery hypertension in heart transplant Recipients. How much is too much? Eur J Cardiothorac Surg 42(5): 864-869.
- Klotz S, Wenzelburger F, Stypmann J, Welp H, Drees G, et al. (2006) Reversible Pulmonary Hypertension in Heart Transplant Candidates: to Transplant or not to transplant. Ann Thorac Surg 82(5): 1770-1773.
- Shumway SJ, Baughman KL, Traill TA, Cameron DE, Fonger JD, et al. (1989) Persistent pulmonary hypertension after heterotopic heart transplantation: a case report. J Heart Transplant 8(5): 387-390.






























