Time is Muscle” - Does Echocardiography Have a Role in STEMI 24/7?
Nachiket J Patel1 and Timothy E Paterick2*
1 Banner/University of Arizona College of Medicine, USA
2 Aurora Health Care, USA
Submission:May 16, 2018; Published: June 11, 2018
*Corresponding author: Timothy E Paterick, Aurora Health Care, Green Bay/Milwaukee, WI, USA, Email: tpaterick@gmail.com
How to cite this article: Nachiket J P, Timothy E P. Time is Muscle” - Does Echocardiography Have a Role in STEMI 24/7?. J Cardiol & Cardiovasc Ther. 2018; 11(1): 555805. DOI: 10.19080/JOCCT.2018.11.555805
Case Report
Transthoracic echocardiography is essential both for diagnosing acute coronary syndrome, zeroing in on the complications of acute myocardial infarction (AMI), and for ruling out other etiologies of acute chest pain including Takotsubo cardiomyopathy, acute pericarditis, aortic dissection, and pulmonary embolism [1,2].
Echocardiography is a vital, non-invasive, and readily available tool in the diagnosis and evaluation of patients with the mechanical complications of AMI [1,2]. Unfortunately, the mechanical complications of AMI are often fatal and, without immediate surgery, patients shortly experience death. The major mechanical complications of AMI are ventricular free wall rupture, ventricular septal rupture, and papillary muscle rupture with severe mitral regurgitation, each of which is capable of triggering cardiogenic shock [3].
Cardiology commentators emphasize that “time is muscle” in acute coronary syndromes and that the time to reperfusion is of utmost importance in salvaging heart muscle function and improving patient outcomes and prognosis. This tenet has made it imperative to minimize any steps that slow the process of door to balloon time [4].
We believe that collaboration between the interventionalist and the echocardiography laboratory is critical to optimal care of patients presenting with STEMI or a simulacrum. We have established a team of echocardiographers and interventionalists that provide immediate care to the STEMI patient presenting to the emergency room 24/7. The echocardiogram is a standard tool in the management of patients with acute myocardial infarction, establishing the diagnosis, location, and extent of MI, diagnosing mechanical complications of infarction, and in providing prognostic information that is important for risk stratification [2].
We present a case where the integration of echocardiography and catheterization lab teams led to a prompt diagnosis and living saving treatment.
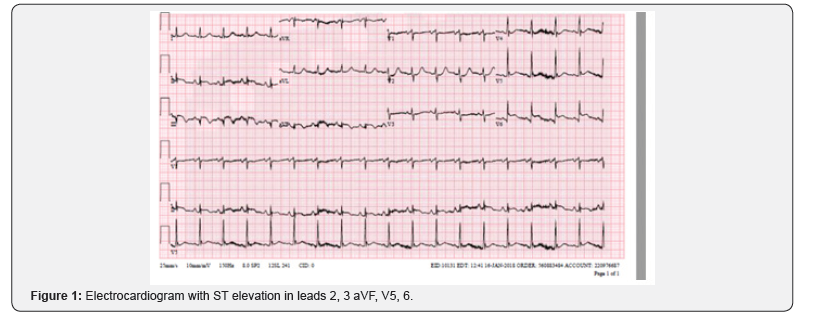
The emergency department calls for a STEMI in a 58 year old female presenting with chest pain and ST elevation inferiorly and laterally (Figure 1).
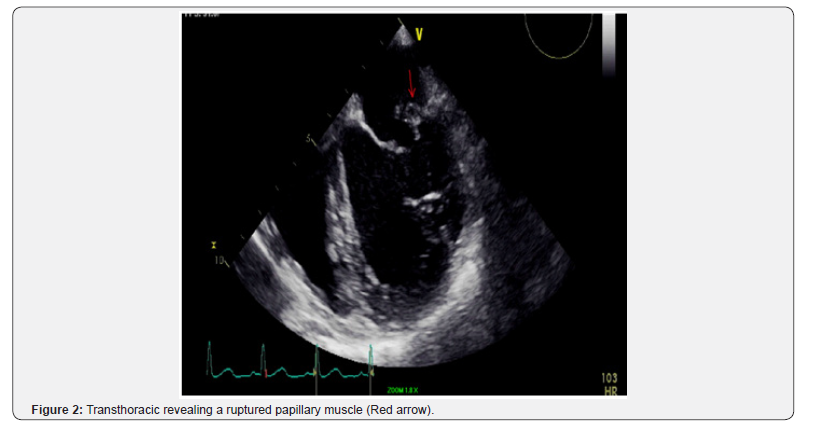
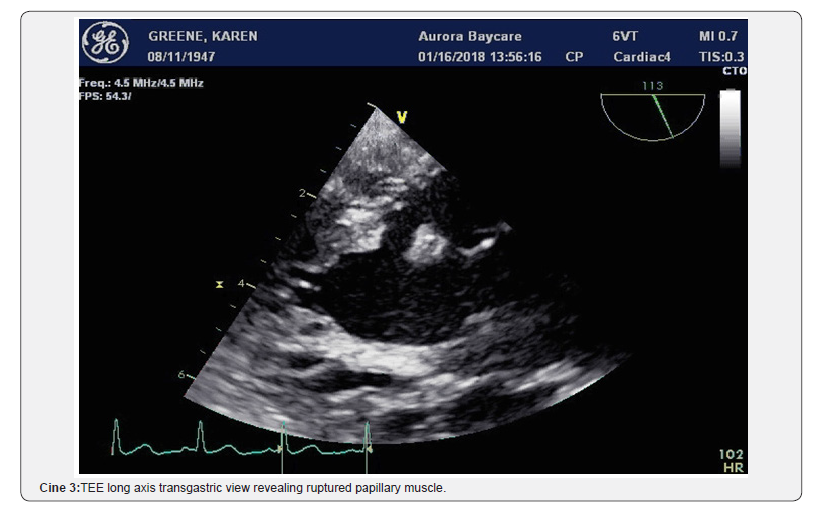
The echocardiographer went immediately to the emergency room as the catheterization laboratory prepared for the patient’s transition to the catheterization lab. The echo was performed to evaluate for wall motion, heart function, and the potential of mechanical complications. This examination can be performed in 5 minutes. The examination revealed an inferolateral wall infarct with a mechanical complication of papillary muscle rupture and severe mitral regurgitation (Figure 2) (Cine 1).

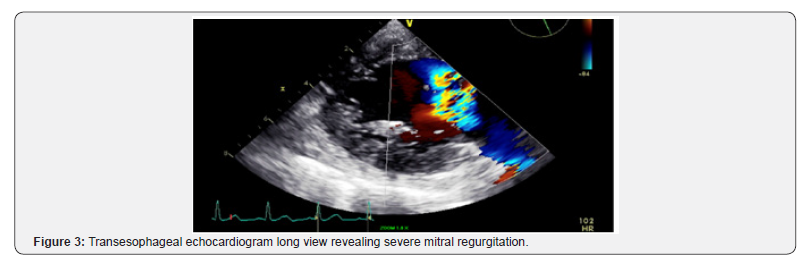
The interventionalist and heart surgeon were immediately notified. A tranesophageal echocardiogram (TEE) is arranged in the catheterization laboratory prior to the heart catheterization as the team recognized this patient needs immediate revascularization and mitral valve surgery.
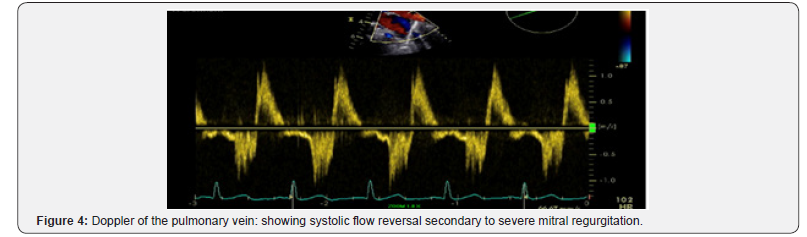
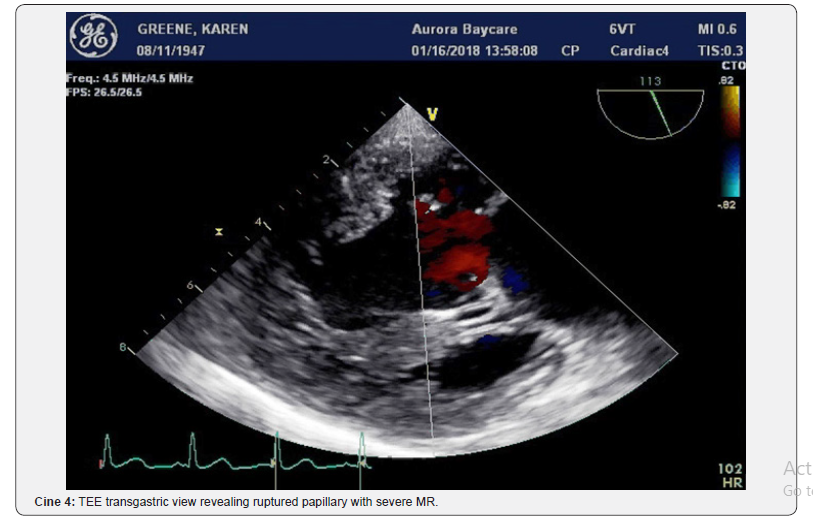
The patient was transported to the catheterization laboratory where the TEE defined the mechanical complications the surgeon will face in the operating room. The TEE revealed a ruptured papillary muscle with wide-open mitral regurgitation and Doppler of the pulmonary vein revealed marked systolic flow reversal (Figure 3 & 4) and (Cine 2-4).

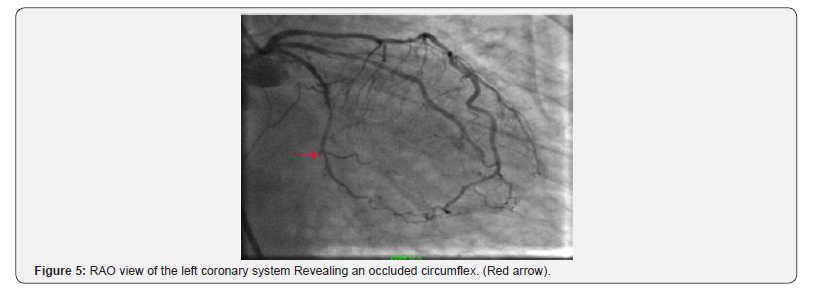
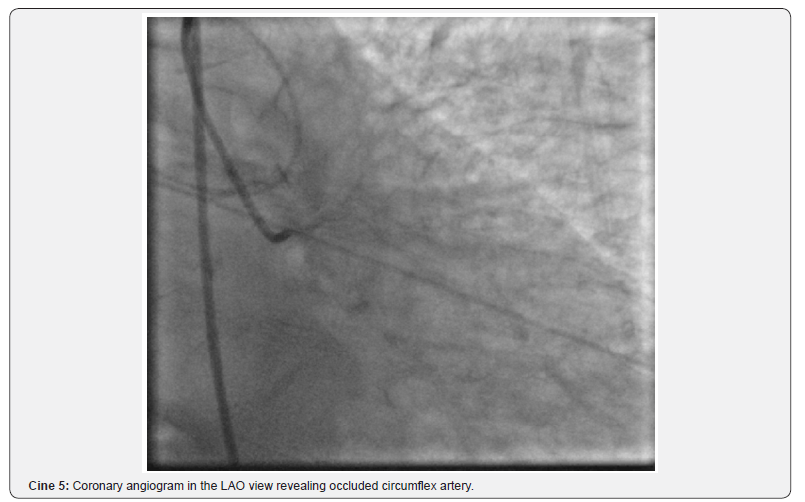
The patient then immediately underwent cardiac catheterization revealing occluded circumflex and diffuse coronary artery disease. (Figure 5) (Cine 5) The mid left anterior coronary had a 70% stenosis. The patient was transferred from the catheterization laboratory where she underwent a mitral valve replacement and LIMA to the LAD. She recovered and was discharged home on day 7.
Discussion
The time from presentation to the emergency room to the operating room was one hour and ten minutes. That time from presentation to operation was achieved due to an infrastructure that maximizes collaboration between he echocardiographer, interventionalist, and heart surgeon. This integrative approach allows for survival in conditions such as ventricular free wall rupture, ventricular septal rupture, papillary muscle rupture with severe mitral regurgitation, aortic dissection, ventricular aneurysm, right ventricular failure, and pulmonary embolism.
Echocardiography is the primary diagnostic tool for detection of potentially life-threatening complications of acute myocardial infarction. Its immediate availability and the detailed information it provides both on the heart’s mechanical function and blood flow is critical in the management of patients with mechanical complications [3,5]. The echocardiography-based decision of referring such patients for immediate surgery makes this diagnostic modality a life-saving procedure. We believe there should be a strong consideration to developing STEMI teams that allow maximum collaborations between the echocardiographer and interventionalist 24/7 because that collaboration and synergy will allow us to safe lives in people that would otherwise succumb to the downward spiral of cardiogenic shock. Collaboration and synergy results in “time is lives” when presented with the mechanical complications of myocardial infarction.
References
- Cheitlin MD, Armstrong WF, Aurigemma GP, Beller GA, Bierman FZ, et al. (2003) ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography-summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice. Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines on the Clinical Application of Echocardiography). Circulation 108(9): 1146-1162.
- Cheitlin MD, Alpert JS, Armstrong WF, Aurigemma GP, Beller GA, et al. (1997) ACC/AHA guidelines for the clinical application of echocardiography. A report of the American College of Cardiology/ American Heart Association Task Force on Practice Guidelines (Committee on Clinical Application of Echocardiography). Developed in collaboration with the American Society of Echocardiography. Circulation 95(6): 1686-1744.
- Kutty RS, Jones N, Moorjani N (2013) Mechanical complications of acute myocardial infarction. Cardiol Clin 31(4): 519-531.
- Antman EM (2008) Time is muscle: translation into practice. J Am Coll Cardiol 52(15): 1216-1221.
- Flachskampf FA, Schmid M, Rost C, Achenbach S, DeMaria AN, et al. (2011) Cardiac imaging after myocardial infarction. Eur Heart J 32(3): 272-283.






























