Infective Endocarditis of the Superior Vena Cava and Right Atrium in Chronic Renal Failure
Leonel Avendaño-Pérez and Nilda Espinola-Zavaleta*
Laboratorio de Ecocardiografíay Hemodinámica No-invasiva, Instituto Nacional de Cardiología Ignacio Chávez, México
Submission: September 08, 2017; Published: September 26, 2017
*Corresponding author: Nilda Espinola-Zavaleta, Instituto Nacional de Cardiología Ignacio Chávez, Juan Badiano N2 1, Colonia Sección XVI, Tlalpan, C. P. 14030, Ciudad de México, México, Email: niesza2001@hotmail.com
How to cite this article: Leonel Avendaño-Pérez , Nilda Espinola-Zavaleta. Infective Endocarditis of the Superior Vena Cava and Right Atrium in Chronic Renal Failure. J Cardiol & Cardiovasc Ther 2017; 8(1): 555727. DOI: 10.19080/JOCCT.2017.08.555727
Abstract
Infective endocarditis is a life threatening disease if not treated; high incidence is found in patients with immune system compromised and prolonged time with intraluminal catheter. We present a case of a patient with renal chronic disease and an acute gout attack with cardiovascular symptoms and further diagnosed with infective endocarditis.
Keywords: Infective endocarditis; Renal failure; Echocardiography; Transesophageal
Background
Infective endocarditis has an estimated annual incidence of 3 to 9 cases per 100,000 persons in industrialized countries [1]. The highest rates are observed among patients with prosthetic valves, intracardiac devices, unrepaired cyanotic congenital heart diseases, or a history of infective endocarditis, although 50% of cases of infective endocarditis develop in patients with no known history of valve disease. Other risk factors include hemodialysis, and coexisting conditions [2]. More than one third of the cases of infective endocarditis in the United States in recent years were reported to be health care-associated (nosocomial or nonnosocomial) [3]. More than 200 cases of Pseudomona aeruginosa endocarditis have been reported [4,5].
Case
A 69 years-old woman with history of diabetes mellitus type 2 and arterial hypertension diagnosed over 30 years ago who has presented microvascular complications of diabetes retinopathy and nephrotic, in renal failure stage V in hemodialysis 1 per week for 3 hours with catheter in right jugular vein. She presented 3 weeks prior her hospitalization with pain in right knee, she came to the emergency room for edema, erythema, redness, warmth, swelling and disability in the right knee, reason why she was hospitalized and evaluated by the service of rheumatology who decided to perform arthrocentesis, finding intracellular monosodium urate crystals in synovial fluid compatible with acute gout, a part of the liquid was sent for culture, reporting sensible strain of Pseudomona aeruginosa, so it was decided to start levofloxacin. During her staying a supraventricular tachycardia was evidenced, with heart rate of 150b.p.m. and remitted with single dose of adenosine I.V. Through her reevaluation a temperature of 38.5oC and a mitral heart murmur grade II/IV were detected. New laboratories were performed, detecting CK-MB of 1.47UI/I. BNP >25.000pg/mL, leukocytes 8.7/L, c-protein reactive 40mg/dL, globular sedimentation rate 122mm/hr and 2 blood cultures with Pseudomona Aeruginosa strain sensible as the one in the arthrocentesis culture. Thoracic radiography showed cardiomegaly.
Discussion
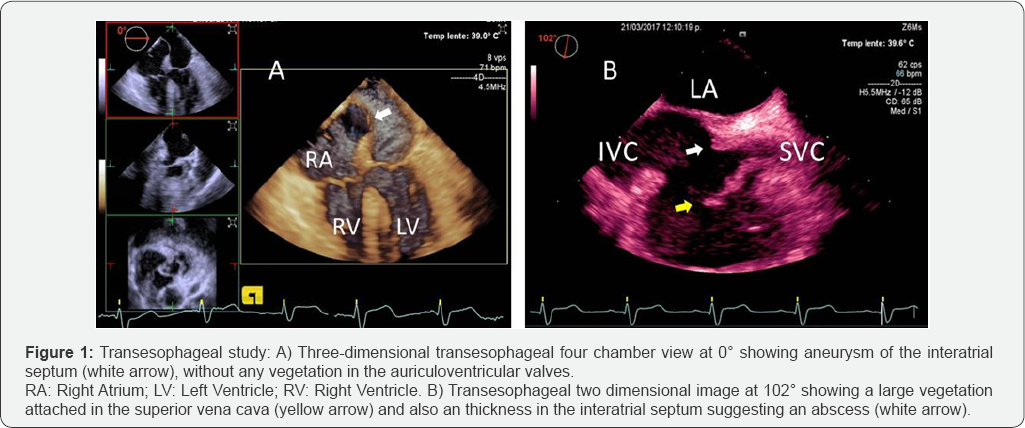
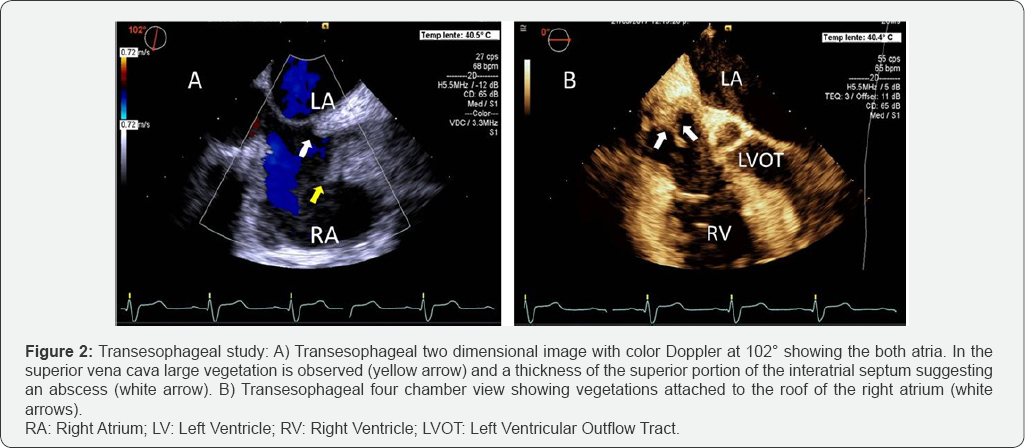
Based on the duke criteria the decision for transesophageal echocardiogram was made, multiple vegetations were found in right atrial and superior vena cava (Figure 1 & 2) and the diagnosis of infective endocarditis was made. Based on her chronic kidney disease stage and hypertension a multidisciplinary group conformed by cardiology, cardiovascular surgery, internal medicine, infectology and nephrology decided that the surgical approach wasn't appropriate and she underwent with antibiotic cephalosporin of 4th generation.
Patient remained with cefepime I.V. in high dose for 8 weeks and allopurinol for her gout event, with clinical improvement of her right knee and no further cardiovascular events, she was discharged. She is still in vigilance in the out-patient nephrology clinic with alarm signs in case of fever or cardiovascular symptoms.
Conclusion
This is a very interesting case of a woman with secondary renal failure in treatment with hemodialysis, who developed infective endocarditis of the superior vena cava and right atrium. In this patient, the clinical judgment and echocardiogram played a very important role in her diagnosis and treatment.
References
- Correa de Sa DD, Tleyjeh IM, Anavekar NS, Schultz JC, Thomas JM, et al. (2010) Epidemiological trends of infective endocarditis: a population- based study in Olmsted County, Minnesota. Mayo Clin Proc 85(5): 422- 426.
- Hoen B, Duval X (2013) Clinical practice. Infective Endocarditis. N Engl J Med 368(15): 1425-1433.
- Benito N, Miro JM, de Lazzari E, Cabell CH, del Ri'o A, et al. (2009) Health care-associated native valve endocarditis: importance of non- nosocomial acquisition. Ann Intern Med 150(9): 586-594.
- Komshian SV, Tablan OC, Palutke W, Reyes MP (1990) Characteristics of left-sided endocarditis due to Pseudomonas aeruginosa in the Detroit Medical Center. Rev Infect Dis 12(4): 693-702.
- Baddour LM, Wilson WR, Bayer AS, Fowler VG, Bolger AF, et al. (2005) Infective Endocarditis: Diagnosis, Antimicrobial Therapy, and Management of Complications: A Statement for Healthcare Professionals From the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, and the Councils on Clinical Cardiology, Stroke, and Cardiovascular Surgery and Anesthesia, American Heart Association: Endorsed by the Infectious Diseases Society of America. Circulation 111(23): e394-e434.






























