Prehypertension: A Study in Youth
Abhay Kumar Pandey1 and Abha Pandit2 *
1Department of Physiology, Government Medical College, Banda, India
2Department of Medicine, Index Medical College, India
Submission: July 18, 2017; Published: August 28, 2017
*Corresponding author: Abha Pandit, Associate Professor, Department of Medicine, Index Medical College, India, Email: drabhaindore@gmail.com
How to cite this article: Abhay K P,Abha P. Prehypertension: A Study in Youth. J Cardiol & Cardiovasc Ther 2017; 7(1): 555707DOI:10.19080/JOCCT.2017.06.555707
Abstrac
Background: Youth of 18 to 20 year age achieve medical college admission through tough competition. Genotype, phenotype and environmental interactions that drive cardiovascular and other lifestyle diseases may be meaningfully recognized at such stage. Early detection of lifestyle disease and its determinants can guide timely interventions and correction toward prevention/reduction of morbidity and mortality.
Objective: Screening of first year male and female medical students for pre-hypertension and a study of family history, clinicodemographic and biochemical characteristics in comparison with normotensive peers.
Method: In a cross sectional study, 23 subjects (16 males and 7 females) in 18-20 year age range found to be prehypertensive upon screening were compared with 15 mached normotensive peers(10 males and 5 females). Familial, psychological behavioral, clinicodemographic and biochemical parameters were examined do define relevant associated trait of prehypertension.
Result: History of maternal hypertension was significant determinant of prehypertension. Dietary and physical activity profiles did not differ but psychologic morbidity was more prevalent in prehypertensives as opposed to the normotensives. Obesity and activation of sympathetic nervous system were particularly associated with prehypertension group. Hyperinsulinaemia and insulin resistance was significantly associated. Lipid profile and level of inflammatory marker homocystein did not significantly differ between prehypertensive group and the normotensive controls.
Conclusion: Family history, obesity, and psychological morbidity had higher association with state of prehypertension. Screening is early age is important to unravel prehypertension and metabolic syndrome, especially in subjects with family history of such disorders. Such subjects can be investigated for risk factors and monitored for disease progression. Timely institution of measures for weight reduction, lifestyle modification, dietetics etc, should avert disease progression and complications.
Keywords: Familial cardiovascular disease; Prehypertension; Metabolic syndrome; Resting heart rate; Homocystein
Introduction
Hypertension is major health concern with rising prevalence world over [1]. Hypertension constitutes 5% of total global disease burden and is implicated in 20% to 50% of all deaths [2]. Hypertension frequently in heres familial atherosclerosis risk [3]. Blood pressure elevation frequently originates in childhood [4]. Overweight and obesity are common risk factors for development of hypertension. Obesity associates increased sympathetic autonomic activity and increased vascular tone [5,6]. Fetal growth retardation, common among the Asians, results in epigenetic aberrations making the offspring vulnerable to develop metabolic syndrome at much younger age upon exposure to adverse environmental determinants as lifestyle and diet [7]. Cardiovascular risk rises continuously across the whole range of blood pressure elevation and underlies coronary heart disease, stroke and other vascular complications. Hypertension is singularly responsible for 1.9% of life years lost and 1.4% disability adjusted life years of global humanity on average [8].
Amid such scenario hypertension and its likelihood need early detection for timely preventive and therapeutic address to avert serious cardiovascular consequences. Medical students from the first year 2009 admission batch at MGM Medical College Navi Mumbai (India), were screened for aberrant blood pressure profiles. Detected prehypertensive profiles merit study of causal issues in the specific population. Clinical evidence so generated, should guide appropriate individualized and general approaches to prevention of hypertension and associated morbidities and mortality.
Subjects and Method
The study protocol involved interview, anthropometry and blood sampling, which was approved by superior research authority. Informed consent of the students was obtained prior to their inclusion in study. Physically handicapped subjects and those on any long term medication were excluded. Those giving history of suffering any illness within a month requiring suspension of routine activities for 3 days or longer were also excluded. Finally 90 subjects (48 males and 42 females) in 18 to 20 year age range were examined.
Resting blood pressure was recorded as per standard method [9], in sitting position after 5 minute rest by mercury sphygmomanometer in right hand, in the quiet clinical physiology room in the Physiology Department in morning between 9am to 10am. Further two measurements were taken at 5 minute intervals to compute average value as data. Students having systolic blood pressure above 120mm Hg to 139mm Hg and/or diastolic blood pressure above 80mm Hg to 89mm Hg were identified as prehypertensives. The hypertensive cutoff was 140/90mm Hg [9,10]. The examination yielded 16 males (33.3%) and 7 females (16.7%), exhibiting prehypertension range of blood pressure. These formed the prehypertensive study group. Control group of normotensives was chosen randomly by toss from the rest comprising 10 males and 5 females.
Detailed interview to elicit history of high blood pressure illness in mother/father or both was conducted. Anthropometric measurements (weight, height, waist and hip circumference) were performed using standardized techniques and the body mass index (BMI), was calculated as body weight in kg/ height in m2. All subjects were screened on a 6 point Centre of Epidemiological Studies Depression (CESD) questionnaire [11]. An assessment of anxiety on 5 point scale [12], was made by grading feeling of nervousness (i.e. never; occasionally; now and then; frequently; daily some time; most of the time). Frequency of exercise in a week was enquired. Using a 24 hour dietary recall, approximate daily calorie consumption was estimated using chronometer software (http/cron-o-meter.com), and % fraction of calories derived from saturated fat consumption was derived as relevant for Indian patients [13].
All participants were examined under fairly similar conditions of October and November. They were instructed to come without consuming coffee or tea and maintain activity as routine over the antecedent 24 hours. Systolic and diastolic blood pressure were measured a fresh, after the subjects have been seated quietly with back supported, feet on the floor and right arm supported for five minutes. Radial pulse rate was then counted in right hand for 30 seconds as per standard procedure [14].
Blood biochemistry tests included, fasting blood sugar, plasma insulin level, and lipid profile and homocystein level. Blood sugar and lipids were analyzed by central investigation lab of the college while insulin and homocystein analyses were outsourced from M/s Jariwala labs, Borivali, Mumbai. Glucose was estimated by glucose oxidase method and plasma lipids determined using enzymatic method. HDL-cholesterol measurement involved homogeneous colorimetric method. LDL- cholesterol was calculated using Friedwalds formula [15]. Serum insulin measurement was by radioimmunoassay technique [16] and homocystein by high performance liquid chromatography (HPLC) technique [17]. The serum separated within an hour of withdrawing blood was frozen at -20 °C and transported in dry ice for distant estimation.
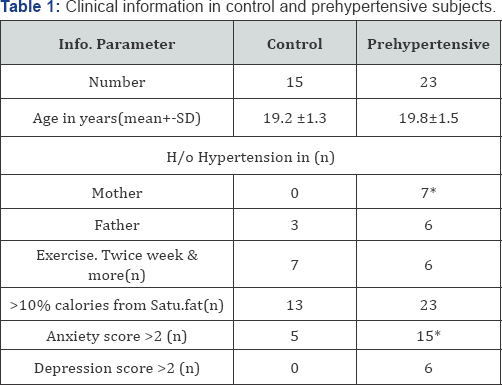
* P<0.05 (Chi square/Fishers Tests)
As shown in Table 1, prehypertensives have significant history of maternal hypertension while paternal history was indifferent from normotensive control. Neither exercise pattern nor dietary saturated fat consumption significantly differ between two groups. Higher anxiety and depression prevailed among the prehypertensives in contrast to controls.
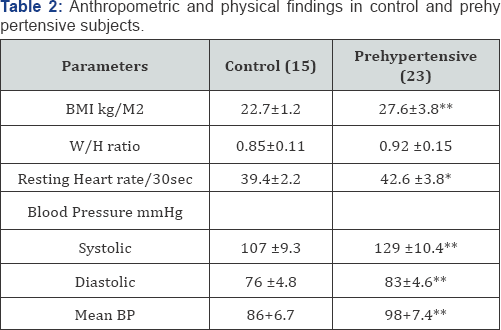
*P<0.01;** P<0.0001 (paired t test)
Table 2, shows significantly higher BMI and W/H ratios in the prehypertensives. The W/H ratio of prehypertensives was above the cut off for central obesity pattern. The systolic and diastolic blood pressures were obviously higher, even resting heart rates were significantly higher in prehypertensives.
Table 3 displays biochemical profiles. Although values of fasting blood glucose and serum homocystein were higher in prehypertensives than in controls, differences were not statistically significant. Fasting serum insulin levels were significantly raised in prehypertensives. This indicates relative insulin resistance among the prehypertensives.
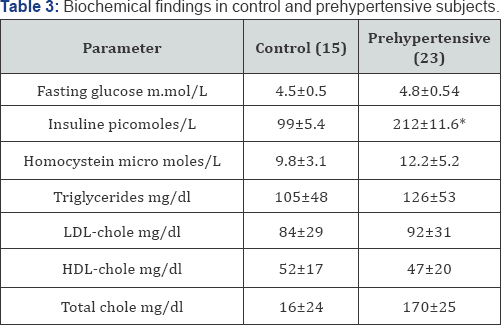
*P<0.0001 (paired t test
Discussion
Urbanization of lifestyle with nutrition transition that involves increased consumption of processed energy dense food are blamed for spread of lifestyle diseases as diabetes and hypertension [7-17]. Prehypertension as such, does not constitute disease but leads to two fold increase in risk of mortality due to coronary artery disease and cerebrovascular accidents [18]. Without lifestyle modification or pharmacologic intervention the prehypertensives are twice as likely to suffer hypertension in few years [19]. 34% to 46% population prevalence of prehypertension is reported in other societies [20-22]. Very different prevalence observed in present study may partly be accounted to the restricted age and socioeconomic group.
Family history of cardiovascular ailment encompasses genetic, biochemical and behavioral contexts and has shown influence on lipids [23], inflammatory markers [24] and haemostatic markers [25]. Individuals with family history of premature atherosclerosis are at higher risk of developing atherosclerosis [26]. Greater risk associated with maternal cardiovascular disease history, may reflect phenotypic evidence that birth weights affect subsequent hypertension [27], insulin resistance [28], and diabetes [29]. The complex mechanisms implied in family history warrant personalized elucidation to discover worthwhile targets for manipulation for disease prevention/reduction [30].
Dietary and physical activity perspectives play role in development of metabolic syndrome wherein, hypertension may be a component. Dietary and physical activity patterns did not differ between compared groups. The prehypertension group exhibited significantly higher prevalence of anxiety and depression that cause adverse biological impact leading to systemic inflammation, endothelial and platelet dysfunction. They also disturb sympathovagal balance leading to impaired protective vagal regulation and increased heart rate [31-33].
The average BMI among prehypertensive group, 27.6kg/ m2 is obesity range by Indian standards [34]. Frequent high W/H ratio is indicative of central obesity selectively associating prehypertension. The insulin levels are significantly higher in prehypertensive group as compared to control, suggesting insulin resistance.
Obesity associate increased sympathetic activity [5,6] and obese adolescents are at increased risk of developing hypertension in adulthood [35]. The findings are in agreement with reported association of insulin resistance in prehypertension [36]. Excess visceral fat reduces hepatic clearance of insulin resulting in Hyperinsulinaemia [37]. Prehypertension is therefore, suggestive of impending metabolic syndrome wherein hypertension occurs early rather than than late.
Resting heart rate was significantly elevated among prehypertensives. High sympathetic tone indicated by raised resting heart rate, contributes to worsening of risks relating blood pressure, glucose metabolism and plasma lipids [38]. Resting heart rate monitoring has long term prognostication value among hypertensive [12,39]. In the present study elevated resting heart rate in prehypertensives is not found associated with worsened blood sugar and lipid profiles. It may simply indicate too early stage of the disorder [40].
Homocystein is formed from dietary amino acid methionine and plays pivotal role in folate metabolism and methyl group transfer. Its concentrations are influenced by genetic and environmental factors, especially vitamins folate, B12, B6 as well as certain lifestyle factors and medications. Significance of homocystein as a cardiovascular risk factor depends on synergistic cardiovascular risk factors such as, nutrition and genetic polymorphisms.
Homocystein plasma levels are shown to directly relate to BMI in boys [41]. Metabolic syndrome with hypertension generally accompanies raised blood homocystein levels that correlate directly to prevalence of cardiovascular complications [42]. Based on studies in adolescents, 90th percentile level of homocystein (found as 8.23micro moles/l), was proposed to be treated as cutoff for hyper-homocysteinaemia [43]. Low HDL- cholesterol was considered to substantiate the cardiovascular risk of hyper-homocysteinaemia. In the present study, homocystein levels were also higher than above proposed cut off 8.23micro moles/l. Atherogenic hyperhomocysteinaemia and dyslipidaemia were not significantly in excess of that in controls, suggesting prehypertension as early stage of metabolic disorder.
Study limitation
The limited study sample drawn from a single admission batch of medical students represents only 18 to 20 year age group that belongs to high socioeconomic class of society. The prevalence of findings is not generallizable beyond such specification even for the purely Indian population sample.
Recommendations for early prevention
There is a graded increase in risk moving from optimal blood pressure (<120/80mm Hg) through normal blood pressure (120-129/80-84mm Hg) to high normal blood pressure (130139/85-89mm Hg), as per Framingham population study [44]. People with higher normal blood pressure levels frequently develop hypertension in a decade or two. Hence the potential risk category of prehypertension was proposed [45]. Around 40% adult population in US was found to be prehypertensive [46]. Group of people at high risk of developing hypertension include those with family history of hypertension, overweight or obese, consuming excess sodium and/or insufficient potassium, alcoholics and with sedentary lifestyle [47].
Screening and detection of prehypertension at early stage should facilitate chances to institute such simple measures of disease prevention and health promotion. Prevention of adult hypertensive disease needs to start early in life by identifying families with history of heart diseases and case detection in youngsters in population. Secondary prevention would include screening for disease progression and taking preventive measures to limit complications. The measures include assessment of other risk factors; weekly monitoring of blood pressure; screening for co-morbidities, as obesity, diabetes, hyperlipidaemia. Short term studies support recommendation of lifestyle modification in such subjects [48,49]. Risk factor modification and behavioral change particularly in diet, physical activity, smoking and drinking cessation are found relevant in hypertension.
The lifestyle modification for primary prevention are similar for prehypertension as for hypertension and include:
A. Engaging in regular aerobic physical activity, at least 30 minutes daily on most days [39,50].
B. Weight loss if overweight/obese to maintain BMI in 18.5 to 24.9kg/m2 [51,52].
C. Consumption of diet rich in fruits and vegetables and low in saturated and total fat [53].
D. Reduction of dietary sodium intake to less than 100mmol or 6gm table salt and adequate intake of potassium(90mmol) daily [48,54].
E. Limiting alcohol consumption if any, to under 60ml of 100-proof whisky per day [55].
Prehypertension in people with cerebrovascular or coronary heart disease qualify for anti hypertensive drug therapy [56]. In this context, baseline systolic blood pressure, diabetes and increased left ventricular mass have been used as predictors of risk score for hypertension development [57]. Early intervention for blood pressure control is associated with eventual better cardiovascular outcomes [58,59].
Conclusion
Family history, obesity, and psychological morbidity had higher association with state of prehypertension. Screening is early age is important to unravel prehypertension and metabolic syndrome, especially in subjects with family history of such disorders. Such subjects can be investigated for risk factors and monitored for disease progression. Timely institution of measures for weight reduction, lifestyle modification, dietetics etc, should avert disease progression and complications
References
- Mohan B, Kumar N, Aslam N, Rangbulla A, Kumbkarni S, et al. (2004) Prevalence of sustained hypertension and obesity in urban and rural school going children in Ludhiana. Indian Heart J 56(4): 310-314.
- (2009) Park K Text Book of Preventive and Social Medicine (20th edn), M/s Banarsidas Bhanot Publ, Delhi, India, pp. 323-327.
- Munger RG, Prineas RJ, Gomez-Marin O (1988) Persistent elevation of blood pressure among children with a family history of hypertension: the minneapolis children's blood pressure study. J Hypertens 6(8): 647-653.
- Curro V, De Luca F, Giusti D, Bracaglia G, Buffetti A, et al. (1988) Correlations between blood pressure values, familial hypertension and anthropometric parameters in a sample of 3-year-old children. Pediatr Med Chir 10(3): 273-276.
- Sowers JR, Whitfield LA, Catania RA, Stern N, Tuck ML, et al. (1982) Role of the sympathetic nervous system in blood pressure maintenance in obesity. J Clin Endocrinol Metab 54(6): 1181-1186.
- Vaz M, Jennings G, Turner A, Cox H, Lambert G, et al. (1997) Regional sympathetic nervous activity and oxygen consumption in obese normotensive human subjects. Circulation 96(10): 3423-3429.
- Pandey AK, Pandey G, Pandey SS, Pandey BL (2013) Human biology of diet and lifestyle linked chronic inflammatory non communicable disease epidemic-a review. Human Biology Review 3(1): 25-42.
- Whitworth JA, World Health Organization, International Society of Hypertension Writing Group (2003) 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens 21(11): 1983-1992.
- Bimenya GS, Byarugaba W, Kalungi S, Mayito J, Mugabe K, et al (2005) Blood pressure profiles among Maker ere university undergraduate students. African Journal of Health Sciences 5(2): 99-106.
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, et al. (2003) The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 289(19): 2560-2572.
- Wassertheil-Smoller S, Shumaker S, Ockene J, Talavera GA, Greenland P, et al. (2004) Depression and cardiovascular sequelae in postmenopausal women. The Women's Health Initiative (WHI). Arch Intern Med 164(3): 289-298.
- Hsia J, Larson JC, Ockene JK, Sarto GE, Allison MA, et al. (2009) Resting heart rate as a low tech predictor of coronary events in women: prospective cohort study. BMJ 338: b219.
- Beegom R, Singh RB (1997) Association of higher saturated fat intake with higher risk of hypertension in an urban population of Trivandrum, in south India. Int J Cardiol 58(1): 63-70.
- (2016) Fitness Zone Online The Heart Rate Measuring Techniques- Taking Your Pulse Manually.
- Friedwalds WT, Levy RI, Fredrickson DS (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18(6): 499502.
- Albano JD, Ekins RP, Maritz G, Turner RC (1972) A sensitive, precise radioimmunoassay of serum insulin relying on charcoal separation of bound and free hormone moieties. Acta Endocrinol (Copenh) 70(3): 487-509.
- Araki A, Sako Y (1987) Determination of free and total homocysteine in human plasma by high-performance liquid chromatography with fluorescence detection. J Chromatogr 422: 43-52.
- Vasan RS, Larson MG, Leip EP, Evans JC, O'Donnell CJ, et al. (2001) Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med 345(18): 1291-1297.
- Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D (2001) Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: a cohort study. Lancet 358(9294): 1682-1686.
- Tsai PS, Ke TL, Huang CJ, Tsai JC, Chen PL, et al. (2005) Prevalence and determinants of pre-hypertension status in the Taiwanese general population. J Hypertens 23(7): 1355-1360.
- Lee JH, Hwang SY, Kim EJ, Kim MJ (2006) Comparison of risk factors between pre-hypertension and hypertension in Korean male industrial workers. Public Health Nurs 23(4): 314-323.
- Erem C, Hacihasanoglu A, Kocak M, Deger O, Topbas M (2009) Prevalence of prehypertension and hypertension and associated risk factors among Turkish adults: Trabzon Hypertension Study. J Public Health (Oxf) 31(1): 47-58.
- Hippe M, Vesto J, Bjerg AM, Borch-Johnsen K, Appleyard M, et al.(1997) Cardiovascular risk factor profile in subjects with familial predisposition to myocardial infarction in Denmark. Journal of Epidemiology and Community Healthjech.bmj.com J Epidemiol Community Health 51(3): 266-271.
- Margaglione M, Cappucci G, Colaizzo D, Vecchione G, Grandone E, et al. (2000) C-reactive protein in offspring is associated with the occurrence of myocardial infarction in first-degree relatives Arterioscler Thromb Vasc Biol 20(1): 198-203.
- Pankow JS, Folsom AR, Province MA, Rao DC, Eckfeldt J, et al. (1997) Family history of coronary heart disease and hemostatic variables in middle-aged adults, atherosclerosis risk in communities investigators and family heart study research group. Thromb Haemost 77(1): 87-93.
- De Backer G, Ambrosioni E, Borch-Johnsen K, Brotons C, Cifkova R, et al. (2003) European guidelines on cardiovascular disease prevention in clinical practice. Third joint task force of european and other societies on cardiovascular disease prevention in clinical practice. Eur Heart J 24(17): 1601-1610.
- Curhan GC, Chertow GM, Willett WC, Spiegelman D, Colditz GA, et al. (1996) Birth weight and adult hypertension and obesity in women. Circulation 15: 94(6): 1310-1315.
- Yarbrough DE, Barrett-Connor E, Kritz-Silverstein D, Wingard DL(1998) Birtweight, adult weight, and girth as predictors of the metabolic syndrome in postmenopausal women: the Rancho Bernardo Study. Diabetes Care 21(10): 1652-1658.
- Phillips D (1998) Birth weight and the future development of diabetes. A review of the evidence. Diabetes Care 21(Suppl 2): B150-B155.
- Silberberg JS, Wlodarczyk J, Fryer J, Robertson R, Hensley MJ (1998) Risk associated with various definitions of family history of coronary heart disease. The Newcastle Family History Study II. Am J Epidemiol 147(12): 1133-1139.
- Ohira T, Diez Roux AV, Prineas RJ, Kizilbash MA, Carnethon MR, et al. (2008) Associations of psychosocial factors with heart rate and its short-term variability: multi-ethnic study of atherosclerosis. Psychosom Med 70(2): 141-146.
- Kim CK, McGorray SP, Bartholomew BA, Marsh M, Dicken T, et al. (2005) Depressive symptoms and heart rate variability in postmenopausal women. Arch Intern Med 165(11): 1239-1244.
- Bleil ME, Gianaros PJ, Jennings JR, Flory JD, Manuck SB (2008) Trait negative affect: toward an integrated model of understanding psychological risk for impairment in cardiac autonomic function. Psychosom Med 70(3): 328-337.
- Snehalatha C, Viswanathan V, Ramachandran A (2003) Cutoff values for normal anthropometric variables in asian Indian adults. Diabetes Care 26(5): 1380-1384.
- Bao W, Threefoot SA, Srinivasan SR, Berenson GS (1995) Essential hypertension predicted by tracking of elevated blood pressure from childhood to adulthood: the Bogalusa Heart Study. Am J Hypertens 8(7): 657-665.
- Player MS, Mainous AG, Diaz VA, Everett CJ (2007) Pre-hypertension and insulin resistance in a nationally representative adult population. J Clin Hypertens (Greenwich) 9(6): 424-429.
- Bjorntorp P (1991) Metabolic implications of body fat distribution. Diabetes Care 14(12): 1132-1143.
- Palatini P, Julius S (1997) Heart rate and the cardiovascular risk. J Hypertens 15(1): 3-17.
- King DE, Everett CJ, Mainous AG, Liszka HA (2006) Long-term prognostic value of resting heart rate in subjects with prehypertension. Am J Hypertens 19(8): 796-800.
- Rocha NG, Templeton DL, Greiner JJ, Stauffer BL, DeSouza CA (2014) Metabolic syndrome and endothelin-1 mediated vasoconstrictor tone in overweight/obese adults. Metabolism 63(7): 951-956.
- Chang JB, Chu NF, Shen MH, Wu DM, Liang YH, et al. (2003) Determinants and distributions of plasma total homocysteine concentrations among school children in Taiwan. Eur J Epidemiol 18(1): 33-38.
- Catena C, Colussi G, Nait F, Capobianco F, Sechi LA (2015) Elevated homocysteine levels are associated with the metabolic syndrome and cardiovascular events in hypertensive patients. Am J Hypertens 28(7): 943-950.
- Gil-Prieto R, Hernandez V, Cano B, Oya M, Gil A (2009) Plasma homocysteine in adolescents depends on the interaction between methylenetetrahydrofolate reductase genotype, lipids and folate: a seroepidemiological study. Nutr Metab (Lond) 6: 39.
- Vasan RS, Larson MG, Leip EP, Evans JC, O'Donnell CJ, et al. (2001) Impact of high normal blood pressure on the risk of cardiovascular disease. N Engl J Med 345(18): 1291-1297.
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, et al. (2003) The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA 289(19): 2560-2572.
- Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, et al. (2009) Heart disease and stroke statistics-2009 update: a report from the American heart association statistics committee and stroke statistics subcommittee. Circulation 119(3): e21-e181.
- Whelton SP, Chin A, Xin X, He J (2002) Effect of aerobic exercise on blood pressure: A meta analysis of randomized controlled trials. Ann Intern Med 136(7): 493-503.
- Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, et al. (1997) A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med 336(16): 1117-1124.
- Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, et al. (2001) Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med 344(1): 3-10.
- (2016) National physical activity guidelines for Australians.
- He J, Whelton PK, Appel LJ, Charleston J, Klag MJ (2000) Long-term effects of weight loss and dietary sodium reduction on incidence of hypertension. Hypertension 35(2): 544-549.
- Stevens VJ, Obarzanek E, Cook NR, Lee IM, Appel LJ, et al. (2001) Longterm weight loss and changes in blood pressure: results of the Trials of Hypertension prevention, phase II. Ann Intern Med 134(1): 1-11.
- Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, et al. (2001) Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med 344(1): 3-10.
- Cutler JA, Follmann D, Allender PS (1997) Randomised trials of sodium reduction: an overview. Am J Clin Nutr 65(2 Suppl): 643S-651S.
- Xin X, He J, Frontini MG, Ogden LG, Motsamai OI, et al. (2001) Effects of alcohol reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension 38(5): 1112-1117.
- Messerli FH, Williams B, Ritz E (2007) Essential hypertension. Lancet 370(9587): 591-603.
- De Marco M, de Simone G, Roman MJ, Chinali M, Lee ET, et al. (2009) Cardiovascular and metabolic predictors of progression of prehypertension into hypertension: the Strong Heart Study. Hypertension 54(5): 974-980.
- Julius S, Kjeldsen SE, Weber M, Brunner HR, Ekman S, et al. (2004) Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomised trial. Lancet 363(9426): 2022-2031.
- Weber MA, Julius S, Kjeldsen SE, Brunner HR, Ekman S, et al. (2004) Blood pressure dependent and independent effects of antihypertensive treatment on clinical events in the VALUE Trial. Lancet 363(9426): 2049-2051.






























