Evaluation of Diabetic Patients with Subclinical Coronary Arteries Disease by the Use of Coronary Calcium Score. Two-Year Study
Alexander Valdés Martín1*, Giorgis Carlos Reyes Navia2, Luis Roberto Llerena Rojas2, Manuel Alejandro Cabrera Fernández2, Dania Guzmán Marín2 and Lila Alicia Sifontes Echevarría2
1Fellow of the American Collegue of Cardiology (FACC), Cuba
2Institute of Cardiology and Cardiovascular Surgery, Cuba
Submission: April 14, 2017, 2017; Published: June 07, 2017
*Corresponding author: Alexander Valdés Martín, Fellow of the American Collegue of Cardiology (FACC), 94 A e/63 y 65 Marianao Apto 1 No 6303, Havana, Cuba, Tel: +53 53581702; Email: avaldes@infomed.sld.cu
How to cite this article: Alexander V M, Giorgis C R N, Luis R L R, Manuel A C F, Dania G M, et al. Evaluation of Diabetic Patients with Subclinical Coronary Arteries Disease by the Use of Coronary Calcium Score. Two-Year Study. J Cardiol & Cardiovasc Ther 2017; 6(1): 555677. DOI: 10.19080/JOCCT.2017.06.555677
Abstract
Introduction and objective: Coronary calcium score (CCS) determined through multiple detector computed tomography is an excellent non-invasive method for detecting coronary atherosclerosis in subclinical stages. In this study we evaluated the presence of coronary artery disease in the subclinical stage by means of the coronary calcium score in diabetic patients.
Methods: Cross-sectional descriptive study in diabetic patients with 10 years or more from it evolution and without coronary disease symptoms. We included different variables such as: demography (age, sex), clinics (smoking habit, alcoholism, and history of hypertension, type of diabetes and evolution's time), and anthropometrics (body mass index), hemoquimics (glycemia, total cholesterol and triglycerides) and imagenologhycs (total coronary calcium score and by artery).
Results: The extensive coronary artery calcification in diabetics patients is frequents. That is locates in the anterior descending artery for both sex. The increases level of glycemia, cholesterol and triglycerides as well as the patients aged are relating with a high coronary calcification in the diabetics patients. The last one is more frequents in diabetics type 1 especially in cases with longer evolution.
Conclusions: Calcium score is useful to diagnose coronary atherosclerosis in diabetic patients without coronary heart disease symptoms with more than 10 years of diagnosed their diabetes.
Keywords: Coronary calcium score; Diabetes mellitus; Coronary arterial disease; Multiple detector computed tomography
Abbreviations: CAC: Coronary Artery Calcification; CCS: Coronary Calcium Score; AU: Agatston Unit
Introduction
Intimal calcification of the coronary arteries is part of the evolutionary process of atherosclerosis at that level. It occurs almost exclusively in the arterial segments affected by this process, usually in small amounts during the initial stages of atherosclerotic lesions and more frequently in lesions and advanced ages [1,2]. Although there is a positive correlation between the site and the amount of the coronary calcium and percent coronary stenosis at the same anatomical site, the relationship is nonlinear and has large confidence limits. Not every coronary atherosclerotic plaque is calcified [3].
The technique described by Agatston [4] to quantify coronary calcium consists of measuring the total area of calcified coronary plaque in pixels, cut by cut, assigning a score. Agatston's calcium score is obtained as a result of the multiplication of the area of the calcified lesion by a factor dependent on the peak signal intensity of the lesion. Coronary artery calcification (CAC) has been shown to be an excellent measure of atherosclerotic load in epicardial vessels and its quantification is consistently higher in patients with clinical coronary disease [5-7].
Coronary calcium score (CCS) determined through multiple detector computed tomography is an excellent noninvasive method for detecting coronary atherosclerosis in subclinical stages. This technique establishes the presence of calcium in the wall of coronaries arteries predicting the risk of coronary events in the long term. Subjects without a CAC or low CCS are less likely to present cardiovascular events than those with elevated scores [8,9]. The prognostic value of CCS has been extensively investigated and very few patients with coronary events have had a calcium score of «0» [7,10-12]. However, this does not mean that there are individuals who have an acute coronary syndrome in whom there has been no evidence of coronary calcification [13].
In Cuba, the introduction of the multiple detector computed tomography occurs in 2006 and although it is introduced in different territories of the country, the CCS has not been generalized enough in the evaluation of symptomatic patients (suspected ischemic heart disease) and even less in the asymptomatic patients risk stratification. There are only few national studies related to the association of CCS and risk factors [14-16], as well as with diabetes [17,18].
Taking into account the importance of achieving a better stratification of cardiovascular risk to guide the intervention strategies towards the most vulnerable population, we motivated to deepen the analysis of the risk of suffering a coronary event and that is why we proposed to evaluate the presence of coronary artery disease in the subclinical stage by means of the CCS in diabetic patients.
Methods
Study population
Cross-sectional descriptive study was lead in the institute of cardiology and Cardiovascular Surgery, in the period from February 2014 to January 2016. The universe involved all diabetic patients with 10 years or more from it evolution. The following inclusion criteria were adopted: age between 35 and 70 years, coronary disease symptoms absence and not previously diagnosis or treatment for this condition. Exclusion criteria were: physical, mental or limiting chronic diseases that impede an adequate communication with the researchers or the transfer to the institution responsible for the study, patients previously diagnosed or under treatment for cardiovascular, cerebrovascular or peripheral arterial disease. A random simple sampling was determined by 164 patients (n=164), who constituted the research sample. The primary variable involved were: demography (age, sex), clinics (smoking habit, alcoholism, and history of hypertension, type of diabetes and evolution's time), and anthropometrics (body mass index), hemoquimics (glycemia, total cholesterol and triglycerides) and imagenologycs (total CCS and by artery).
Methodology in the acquisition of the variables to be included in the study
A structured interview was conducted for each patient by two specialists in cardiology who give consultations at the national diabetes care center with experience in the subject for more than five years as well as a resident of cardiology previously trained by the aforementioned experts. The primary variables involved were collected in a model developed for this purpose. The Body mass index (BMI) was obtained in the same way: the patient was placed barefoot in light clothing, with his head in the Frankfort plane, on a weight-measuring device. The result was obtained in centimeters. The weight was calculated on the same equipment and was valued in kilograms. It was calculated according to Quetelet's formula: weigh in Kg/height (m)2.
The patients were also referred to the hospital's clinical laboratory for blood collection and determination of the hematologic variables of interest. In all participants, extraction (10ml) was done by puncture in the ulnar vein and the blood was deposited in a tube with EDTA, a tube with heparin and a tube with dry serum gel. The RapiGluco-Test, Colestest and Monotriglitest reagents, respectively, produced at the company «Carlos J. Finlay», La Habana, Cuba, were used for the determination of glycemia, total cholesterol and triglycerides. The glycemia was processed in an Eppendorf team using colorimetric enzymatic method and cholesterol and triglycerides in a Hitachi team. Subsequently, these subjects were referred to the Department of Computed Tomography for the determination of the CCS.
Coronary calcium score
The images were captured in a computerized tomography of 64 cuts (Somatom Sensation Cardiac, Siemens, Germany), using a spiral scanning protocol that uses the retrospective synchronization by electrocardiogram and a rotation time of 0.33 seconds for coronary calcium quantification studies. Topogram: anteroposterior, from the carina to the apex of the heart. The acquisition parameters used were: kilovolts: 120; Most effective product: 190; Window: mediastinum; Image order: cranium-caudal; Rotation time: 0.33 seconds; Collimation of cut: 1.2; Cutting width: 3mm; Advance / rotation: 4.8mm; Factor pitch: 0.2; Reconstruction increment: 1.5mm; Temporal resolution: 83ms; Filter: B 35f Heartv medium; CTDI vol: 12.9mGy. Retrospective reconstructions were performed, synchronized with the electrocardiogram and 55% of the cardiac cycle in diastole. The plate detection threshold used was 130UH (Hounsfield Units). The measurement of the coronary calcium score was performed using the Agatston method.
Statistic analysis
We determined the distribution and association of the general characteristics of the patients under study, expressing the categorical variables in absolute numbers and percentages and the continuous variables in mean values and standard deviation. The chi squrare test was applied for the qualitative variables and Student t for the quantitative variables in the univariate analysis, taking a 95% confidence interval for a significant association if p <0.05. The presentation of the results was done using tables, graphs and representative figures. This study complies with the Declaration of Helsinki. The review board of the Institute of Cardiology approved the study, and written informed consent was obtained from all patients.
Results
Coronary calcium score per patient and per artery
A total of 164 diabetic patients were included, 99 (60.4%) of the female sex, with a mean age of 55.5±8.6 years. Approximately half of the patients (n=83, 50.6%) had some degree of coronary artery calcification. Of these, 23.2% (n=38) had a CCS between 101-399 AU while, 13.4% (n=22) had a CCS greater than or equal to 400AU (Figure 1).
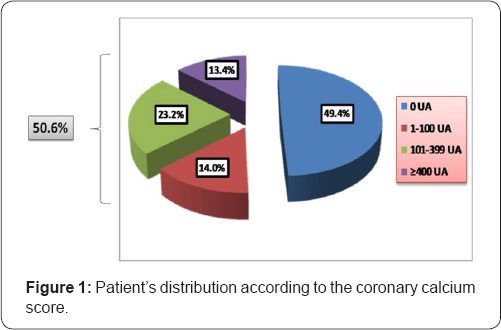
AU: Agatston Unit
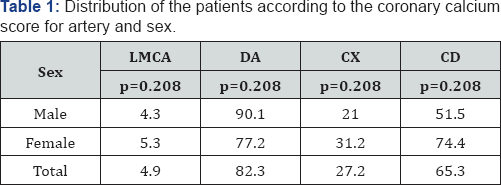
LMCA: Left Main Coronary Artery; DA: Anterior Descending Artery; Cx: Circumflex Artery; CD: Right Coronary Arter
In the Table 1 a major CCS is observed, so much for the population in study as for both sexes, in the anterior descending artery followed by the right coronary, the circumflex and finally left main coronary artery. In the distribution by sex, a higher CCS was observed in the anterior descending for men (90.1AU vs 77.2AU, respectively) while in women the CCS was higher for the right coronary (74.4AU vs 51.5AU) and circumflex arteries (31.2AU vs 21.0AU), although none of these differences were significant.
Relationship of cardiovascular risk factors with the presence and severity of coronary artery calcification
In the Table 2 is presented an analysis according to quartiles of coronary artery calcification, note that age, total cholesterol and triglycerides showed a proportional and significant increase with the advance of coronary artery calcification. On the other hand, the percentage of patients with a history of alcoholism is low. No significant differences were found between the two comparison groups for sex, skin color, smoking, alcoholism, hypertension and BMI. Blood glucose levels although showing a proportional rise with the CCS increase, showed no significant differences.
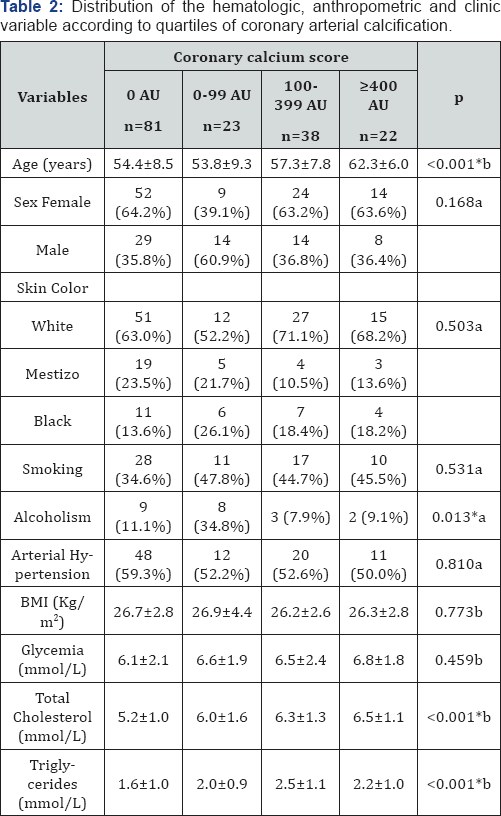
BMI: Body Mass Index; *significant association; aChi2 test; bStudent
Relationship between type and duration of diabetes with the CCS
*Significant association; achi2 test
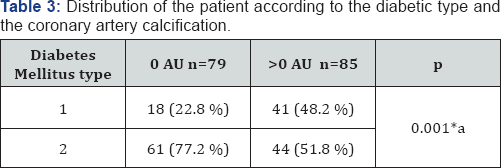
The Table 3 shows that 48.2% of type 1 diabetic patients presented a CCS >0AU establishing a significant association, not so with type 2 diabetic patients, with a predominance of patients with 0AU (77.2% vs 51.8%).
The proportional rise of the arterial coronary calcification was associated in a significant mode with an increase in the percentage of patients with diabetes type 1 (22.2% [0 AU] vs 47.8% [1-100AU] vs 36.8% [101-399AU] vs 72.7% [=400AU], respectively, p <0.001) (Table 4).
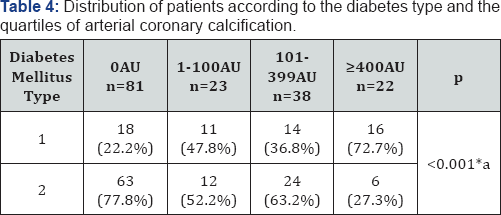
*Significant association; achi2 test
*Significant association; achi2 test

*Significant association; achi2 test
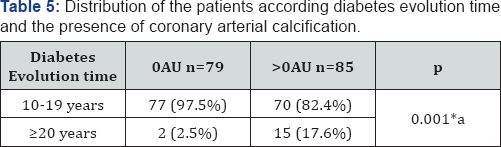
The patients with some degree of arterial coronary calcification proved to be a significantly major percentage of patients with time of evolution of the major diabetes of 20 years in comparison to those with CCS in 0UA (17.6% vs 2.5%, p=0.001) (Table 5). The proportional increase of the arterial coronary calcification was associated in a significant way with an rise in the percentage of patients with time of evolution of the disease ≥20 years (2.5% [0AU] vs 0.0% [1-100AU] vs 13.2% [101-399AU] vs 45.5% [=400AU], respectively, p <0.001) (Table 6)
Discussion
Coronary calcium score per patient and per artery
In the present study, about half of the diabetic patients had some degree of coronary artery calcification, of which 36.6% had a CCS greater than 100AU. In the general population, Blaha et al. [19] in a study with asymptomatic patients report 45% with CCS=0 and 12% with CCS values of 1-10AU. In Cuba, Cabrera-Rego et al. [20] included 300 asymptomatic adults taken from the general population, in which 65.7% had a CCS between 0-10AU, 17.4% CCS between 11-99AU, 12.6% CCS between 100- 399AU and only 4.3% CCS greater than 400AU.In a recent study of 1123 patients with diabetes, the prevalence of coronary atherosclerosis was greater than that found in this study, since 86.0% of patients had a CCS greater than 10AU, while 53.0% had a CCS greater than 300 AU [21]. The PREDICT study [22] which included 589 patients with diabetes without a history of cardiovascular disease showed a CCS lesser than 10AU in 23.4% and a CCS greater than 400AU in 25.5%. Anand et al. [23], reported a higher prevalence in asymptomatic diabetics since 46.3% had a CCS greater than 10AU. In another report of 478 asymptomatic type 2 diabetics, Leem et al. [24], found that 32.8% of patients had a CCS=0AU while 31.6% had CCS between 1-100AU, 19.2% between 101-400AU and remaining 16.3% a CCS greater than 400AU. In a recent comparative study conducted in Cuba by Peix et al. [25], the CCS in diabetic patients was 74.1±168.8AU vs 5.2±14.6AU in controls, p <0.01. In the diabetic group, 13.6% had a CCS greater than 100AU. On the other hand and regarding the distribution of CCS by artery, a higher CAC was found for the anterior descending. However, gender differences were interesting, as calcium deposition was greater in women in the circumflex and right coronary arteries. Arjmand et al. [26], found similar results as CAC was higher for the anterior descending one. In a recent study by Sabour et al. [27], which included 566 postmenopausal women, 15.8% had CAC in the left main coronary artery, 43.9% in the anterior descending artery, 23.1% in the right coronary artery, and the remaining 19.4% in the left coronary artery circumflex.
Relationship between cardiovascular risk factors with the CAC's presence and severity
In the present study, age was not only significantly higher in diabetics with some degree of CAC, but a proportional increase in age was found with increasing quartiles of CCS. On the contrary, although in the patients with some degree of CAC a slightly higher percentage of males were found, these differences were not significant. In a recent report by Rodriguez et al. [28], that included 100 patients with diabetes, patients with CAC were significantly older than those with a CCS=0 (47±9 vs 37±9), although the percentage of men did not had differences between both comparison groups (67.7% vs 55.1%). In that study, the odds of increased CAC were 2.73 times greater for every additional 10 years of age. The Heinz Nixdorf Recall Study [29], which included 4814 people from the general population who were followed for a period of 5.1 years, found that CAC was present in men in 23.3% and in women in 15.3% in the group of 45 -49 years increased to 66.7% in men and 42.9% in women in the 70-74 age group. As can be seen, the percentage of calcification is consistently lower in women, and these results have been reported in other studies [30].
On the topic of the rest of the clinical variables analyzed, in this study neither skin color, smoking, history of alcoholism, hypertension and BMI were related to the presence of CAC. In the CCS quartile analysis, only the percentage of patients with a history of alcoholism was significantly lower in those with a higher CCS. In the report by Rodríguez et al. [28], the color of the skin, smoking and BMI also did not show a significant relationship with CAC in diabetic patients. In a study by Wade et al. [31], in type 2 diabetics, African Americans showed significantly lower CCS values than non-Hispanic whites for both sexes. On the other hand, Wagenknechty et al. [32] also found significantly lower values of CAC in blacks versus whites. Regarding skin color, it should be taken into account that the data obtained only by the phenotypic appearance can lead to misunderstandings, because there are patients classified with white skin that are not due to the wide miscegenation of the Cuban population.
In relation with the smoking, it is well-known that this habit promotes the atheroma's plate formation especially for the free radical derivate of cigar smoke that increases the oxidative stress and the concentration of inflammatory scoreboards. This effect is major in the smokers' diabetic population which was demonstrated in the ARIC study [33].
In an interesting way, in the study of Leem et al. [24], though the precedent of smoking did not show the relation with the increase of the CAC, one found a significant relation between this habit and the presence of plates not calcified in diabetics with CCS=0, aspect that agrees with other studies in which there it has been demonstrated that smoking is a fort predictor of not calcified obstructive plates [34]. More than half of the diabetic patients suffer from hypertension and the last one is been recognized as the most important cardiovascular risk scoreboard since there is evidence of which the pressure elevation increase the possibility of suffering ischemia heart disease. In regard to the arterial hypertension, in another study realized by Rodríguez et al. [35], in 261 diabetics type 1, the hypertense patients had to probability twice major with regard to the not hypertense ones in having to major CCS of 0 AU. In fact the HTA was the only component of the metabolic syndrome in showing relation with the CAC.
In the report of Leem et al. [24], the age, the percentage of patients of the masculine sex and of patients with arterial hypertension, increased in to proportional and significant way with the increase of CAC’s quartiles in diabetic type 2. On the contrary the BMI was a variable that did not show differences with the progression of the CAC in the present study. However other author like Rodríguez et al. [36], reported in 621 diabetics' type 1, a significant relation between the corporal overweight and the obesity with major risk of suffer CAC.
In the present study, the numbers of glycemic, total cholesterol and triglycerides were significantly major in the patients with some degree of atherosclerosis coronary whereas the total cholesterol and the triglycerides related to the progression of the CAC according to increase of CCS’s quartiles. In Rivera’s et al. [37], in 906 asymptomatic individuals without diabetes a significant relation was demonstrated between the values of glycosilated hemoglobin (HbAlc) and number of coronary segments by plate atherosclerotic. On the other hand,Schindler et al. [38], there demonstrated in diabetic type 2 that the reduction supported of the glycemic correlates with a slower progression of the CAC.
In Rodríguez et al. [28], the values of total cholesterol, triglycerides, HDL-C, LDL-C and HbAlc did not show significant differences between the diabetic patients with and without CAC. Equally; in the study of Wagenknecht et al. [32], the levels of triglycerides and HDL-C was similar between both groups of comparison. Jaechan et al. [24], did not find relation between the precedent of dyslipidemia, as well as the values of total cholesterol, LDL-C, HDL-C and triglycerides with the severity of the CAC either.
In Cuba, Buchaca et al. [18], brought in 59 patients with diabetes type 2, one major number of patients with hyperglycemia presented coronary hurt on having compared them with the patients with good glycemic control (p=0,024), relation that was more evident with the hyperglycemia postprandial. The hyperglycemia showed a probability 5.99 times major of detecting coronary injuries for tomography on having compared it with other major risk atherosclerotic factors.
Relationship between type and duration of diabetes with the CCS
In the present study, type 1 diabetes showed a greater relationship with the presence and extent of subclinical coronary atherosclerosis according to CCS. In patients with type 1 diabetes, the prevalence of CAC is 18% before age 30 and 50% at age 40, compared to 1% before age 30 and 27% at age 40 in non-diabetic adults. Contrary to our results, Djaberi et al. [39], included 135 asymptomatic diabetic patients divided into two groups according to type 1 diabetes (n=65) and type 2 (n=70). There were no significant differences in CCS between the two comparison groups in this study, although the mean CCS was higher in patients with type 1 diabetes (217 vs 174 UA). However, the prevalence of coronary atherosclerosis was slightly lower in this group than in patients with type 2 diabetes (65% vs 71%). Likewise, the prevalence of coronary obstruction was higher in patients with type 2 diabetes (34% vs 17%) as well as the percentage of patients with non-calcified plaques (66% vs 27%). Similarly, Scholte et al. [40], observed a higher prevalence of coronary atherosclerosis which generally involved more than one coronary artery in type 2 asymptomatic diabetics. On the other hand, as demonstrated in the present study, the evolution time of diabetes is one of the most important factors in the development of micro and macrovascular complications. Several studies have also reported a proportional and significant relationship between the duration of diabetes and the presence and extent of CAC [41].
Conclusion
In the investigation, it was observed that extensive coronary artery calcification is very frequent in diabetic patients especially in those with a long life; disorders of carbohydrate and lipid metabolism closely related to increased coronaryartery calcification in these patients, as well as those who have diabetes type 1 and have a longer duration of diabetes.
References
- Llerena R, Peix A, Valiente J (2011) Técnicas de imagen no invasiva en la valoración y la prevención de la enfermedad coronaria. Rev Cubana Cardiol Cir Cardiovasc 11(E): 36-44.
- Motoyama S, Sarai M, Harigaya H, Anno H, Inoue K, et al. (2009) Computed tomographic angiography characteristics of atherosclerotic plaques subsequently resulting in acute coronary syndrome. J Am Coll Cardiol 54(1): 49-57.
- Madder RD, Chinnaiyan KM, Marandici AM, Goldstein JA (2011) Features of disrupted plaques by coronary computed tomographic angiography correlates with invasively proven complex lesions. Circ Cardiovasc Imaging 4(2): 105-113.
- Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, et al. (1990) Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 15(4): 827-832.
- Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, et al. (2008) Coronary calcium as a predictor of coronary events in four racial or ethnic groups. New Engl J Med 358(13): 1336-1345.
- Erbel R, Möhlenkamp S, Moebus S, Schmermund A, Lehmann N, et al. (2010) Coronary risk stratification, discrimination, and reclassification improvement based on quantification of subclinical coronary atherosclerosis: the Heinz Nixdorf Recall study. J Am Coll Cardiol 56(17): 1397-1406.
- Polonsky TS, McClelland RL, Jorgensen NW, Bild DE, Burke GL, et al. (2010) Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA 303(16): 1610-1616.
- Coylewright M, Rice K, Budoff MJ, Blumenthal RS, Greenland P, et al.(2011) Differentiation of severe coronary artery calcification in the multiethnic study of atherosclerosis. Atherosclerosis 219(2): 616-622.
- Budoff MJ, Nasir K, McClelland RL, Detrano R, Wong N, et al. (2009) Coronary calcium predicts events better with absolute calcium scores than age-sex-race/ethnicity percentiles: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol 53(4): 345-352.
- Folsom AR, Kronmal RA, Detrano RC, O'Leary DH, Bild DE, et al. (2008) Coronary artery calcification compared with carotid intimamedia thickness in the prediction of cardiovascular disease incidence: the Multi-Ethnic Study of Atherosclerosis (MESA). Arch Intern Med 168(12): 1333-1339.
- Budoff MJ, Hokanson JE, Nasir K, Shaw LJ, Kinney GL, et al. (2010) Progression of coronary artery calcium predicts all-cause mortality. JACC Cardiovascu Imaging 3(12): 1229-1236.
- Ioannidis JP, Tzoulaki I (2010) What makes a good predictor? the evidence applied to coronary artery calcium score. JAMA 303(16): 1646-1647.
- Cho I, Suh JW, Chang HJ, Kim KI, Jeon EJ, et al. (2013) Prevalence and prognostic implication of non-calcified plaque in asymptomatic population with coronary artery calcium score of zero. Korean Circ J 43(3): 154-160.
- Mendoza V, Llerena LR, Torres S, Olivares EW, Cabrera JO, et al. (2010) Utilidad del score de calcio en el diagnóstico de enfermedad coronaria obstructiva. Rev Invest Biomed 29(4): 1-14.
- Mendoza V, Llerena LR, Olivares EW, Cabrera JO, Armas NB, et al.(2010) Puntaje de calcio y severidad de la enfermedad coronaria. Rev Cubana Cardiol Cir Cardiovasc 16(1): 84-98.
- Olivares EW, Rodríguez Y, Mendoza V, Llerena LR, Cabrera JO, et al.(2012) Asociación entre algunos factores de riesgo cardiovascular y el puntaje de calcio coronario en pacientes sintomáticos. Rev Cubana Invest Biomed 31(4): 447-458.
- Vicente BM, Zerquera G, Jorrín FR, de la Cruz LE, Rivas EM (2011) Cuantificación del calcio coronario y riesgo cardiovascular en pacientes con diabetes mellitus tipo 2. Medisur 9(1): 73-78.
- Buchaca EF, Bencomo L, Bermúdez S, Hierro D, Mora I, et al. (2010) Aterosclerosis coronaria subclínica detectada por tomografía axial multicorte y su asociación con la hiperglucemia. Rev Cubana Med 49(2): 22-33.
- Blaha M, Budoff MJ, Shaw LJ, Khosa F, Rumberger JA, et al. (2009) Absence of coronary artery calcification and all-cause mortality. JACC Cardiovasc Imaging 2(6): 692-700.
- Cabrera-Rego JO, Iacobellis G, Sarmientos JC, Mustelier JV, Aquiles EW, et al. (2011) Epicardial fat correlates with ApoB/ApoA1 ratio, Coronary Calcium and Carotid Intima Media Thickness in asymptomatic patients. Int J Cardiol 151(2): 234-236.
- Agarwal S, Cox AJ, Herrington DM, Jorgensen NW, Xu J, et al. (2013) Coronary calcium score predicts cardiovascular mortality in diabetes. Diabetes Care 36(4): 972-977.
- Elkeles RS, Feher MD, Flather MD, Godsland IF, Nugara F, et al. (2004) The association of coronary calcium score and conventional cardiovascular risk factors in type 2 diabetic subjects asymptomatic for coronary heart disease (the PREDICT study). Diabet Med 21(10): 1129-1134.
- Anand DV, Lahiri A, Lim E, Hopkins D, Corder R (2006) The relationship between plasma osteoprotegerin levels and coronary artery calcification in uncomplicated type 2 diabetic subjects. J Am Coll Cardiol 47(9): 1850-1857.
- Leem J, Hee Koh E, Jeong E, Jang JE, Lee SW, et al. (2012) Prevalence of Angiographically Defined Obstructive Coronary Artery Disease in Asymptomatic Patients with Type 2 Diabetes According to the Coronary Calcium Score. Intern Med 51(21): 3017-3023.
- Peix A, Cabrera LO, Heres F, Rodríguez L, Valdés A, et al. (2011) Interrelationship between myocardial perfusion imaging, coronary calcium score, and endothelial function in asymptomatic diabetics and controls. J Nucl Cardiol 18(3): 398-406.
- Arjmand A, Akhlaghpoor S, Shadmani M, Ebrahini M, Shakiba M, et al. (2006) Agreement Determination between Coronary Calcium-Scoring and Coronary Stenosis Significance on CT- angiography. Iran J Radiol 3: 85-90.
- Sabour S, Bartelink ML, Rutten A, Grobbee DE, Prokop M, et al. (2009) Cardiovascular Risk Factors and Specific Coronary Artery Calcification in Postmenopausal Women. J The Univ Heart Ctr 3: 171-176.
- Rodríguez TC, Biavatti K, Almeida FK, Gross JL (2010) Coronary artery calcification is associated with insulin resistance index in patients with type 1 diabetes. Braz J Med Biol Res 43(11): 1084-1087.
- Lehmann N, Möhlenkamp S, Mahabadi AA, Schmermund A, Roggenbuck U, et al. (2014) Effect of smoking and other traditional risk factors on the onset of coronary artery calcification: Results of the Heinz Nixdorf recall study. Atherosclerosis 232(2): 339-345.
- Olson JC, Edmundowicz D, Becker DJ, Kuller LH, Orchard TJ (2000) Coronary calcium in adults with type 1 diabetes: a stronger correlate of clinical coronary artery disease in men than in women. Diabetes 49(9): 1571-1578.
- Wade A, Fedyna S, Mehta N, St Clair C, Ginwala N, et al. (2011) Type 2 diabetes does not attenuate racial differences in coronary calcification. Diabetes Res Clin Pract 91(1): 101-107.
- Wagenknecht LE, Divers J, Bertoni AG, Langefeld CG, Carr JJ, et al. (2011) Correlates of coronary artery calcified plaque in blacks and whites with type 2 diabetes. Ann Epidemiol 21(1): 34-41.
- Howard G, Wagenknecht LE, Burke GL (1998) Cigarette smoking and progression of atherosclerosis: The Atherosclerosis Risk in Communities (ARIC) Study. JAMA 279(2): 119-124.
- Rivera JJ, Nasir K, Cox PR (2009) Association of traditional cardiovascular risk factors with coronary plaque sub-types assessed by 64-slice computed tomography angiography in a large cohort of asymptomatic subjects. Atherosclerosis 206(2): 451-457.
- Rodriguez TC, Canani LH, Schvartzman P, Gross JL (2011) Hypertension is the metabolic syndrome component most strongly associated with microvascular complications and coronary artery calcification in Type 1 diabetes. J Endocrinol Invest 34(3): e58-e63.
- Rodríguez TC, Veyna AM, Haarhues MD, Kinney GL, Rewers M, et al. (2011) Obesity and Coronary Artery Calcium in Diabetes: The Coronary Artery Calcification in Type 1 Diabetes (CACTI) Study. Diabet Technol Ther 13(10): 991-996.
- Rivera JJ, Choi E, Yoon Y, Chun E, Choi S, et al. (2010) Association between increasing levels of hemoglobin A1c and coronary atherosclerosis in asymptomatic individuals without diabetes mellitus. Coron Artery Dis 21(3): 157-163.
- Schindler T, Cadenas J, Li Y, Sayre J, Goldin J, et al. (2009) Effect of glucose lowering on coronary vascular function, carotid intima-media thickness and coronary artery calcification in type 2 diabetes mellitus. J Nucl Med 50(Suppl 2): 539.
- Djaberi R, Schuijf JD, Boersma E, Kroft LJM, Pereira AM, et al. (2009) Differences in Atherosclerotic Plaque Burden and Morphology Between Type land 2 Diabetes as Assessed by Multislice Computed Tomography. Diabetes Care 32(8): 1507-1512.
- Scholte AJ, Schuijf JD, Kharagjitsingh AV, Jukema JW, Pundziute G, et al. (2008) Prevalence of coronary artery disease and plaque morphology assessed by multi-slice computed tomography coronary angiography and calcium scoring in asymptomatic patients with type 2 diabetes. Heart 94(3): 290-295.
- Reinhard H, Hansen PR, Persson F, Tarnow L, Wiinberg N, et al.(2011) Elevated NT-pro BNP and coronary calcium score in relation tocoronary artery disease in asymptomatic type 2 diabetic patients with elevated urinary albumin excretion rate. Nephrol Dial Transplant 26(10): 3242-3249.






























