Thrombosis of the Left Main Stem following Steroid Abuse in a 21 Year Old Male Mimicking Spontaneous Dissection
Kaul P1*, Sivananthan M2 and Paniagua R3
1Consultant Cardiac Surgeon, Leeds General Infirmary, England
3Cardiac surgical registrar, Leeds General Infirmary, England
Submission: April 17, 2017; Published: June 06, 2017
*Corresponding author: Kaul P, Consultant Cardiac Surgeon, Leeds General Infirmary, Great George Street, Leeds, LS1 3EX, England, Tel: 0113 3925568; Fax: 0113 3925408; Email: pankaj.kaul@nhs.net
How to cite this article: Kaul P, Sivananthan M, Paniagua R. Thrombosis of the Left Main Stem following Steroid Abuse in a 21 Year Old Male Mimicking Spontaneous Dissection. J Cardiol & Cardiovasc Ther. 2017; 6(1): 555676. DOI:10.19080/JOCCT.2017.05.555676
Abstract
A 23 year old man presented with anterior ST elevation myocardial infarction while playing football and gave a 3 week history of recreational intravenous steroid abuse. Coronary angiogram showed a large persistent filling defect in left main stem extending into LAD and intermediate arteries. This was felt to be either spontaneous left main dissection precipitated by heavy exertion or left main stem thrombosis facilitated by intravenous steroid abuse over the previous 3 weeks. He was offered immediate surgical revascularisation but elected instead to have delayed surgery after 2 weeks unless symptoms worsened. Repeat coronary angiogram, two weeks later, however, showed considerable improvement with only a small amount of residual thrombus in left anterior descending artery and hence it was elected to continue with medical treatment. Following further 6 weeks, repeat coronary angiogram showed total resolution with normal coronary artery appearances. At 7 year follow up, patient is free of all cardiac symptoms and is leading a normal life.
We discuss the diagnostic dilemma in this 21 year old man with no risk factors for coronary artery disease, who had features that pointed towards both spontaneous coronary artery dissection (SCAD) and steroid facilitated thrombosis and in whom intravascular ultrasound underlined at least the facilitative role of atheromatous left main plaque. We also discuss the etiopathogenesis, presentation and the various treatment options of the rare spontaneous left main dissection and the steroid induced even rarer left main thrombosis and the quasi-facilitative role of at least mild atherosclerosis in this patient, and the relative rarity of spontaneous resolution with conservative management.
Background
Spontaneous acute dissection of left main stem artery is an extremely rare occurrence, with less than 40 cases documented in world literature. The clinical presentation of spontaneous left main stem dissection is similar to severe atherosclerotic disease, but the usual risk factors are absent. More than 70% of SCAD occurs in women and 30% occur during peripartum period and the mean age is 30-45 years. Other causes include connective tissue disorders, SLE vasculitis, substance abuse and vigorous exercise. However, varying degree of atherosclerosis has been increasingly described in many patients with SCAD. In one series when intravascular ultrasound was used routinely to evaluate SCAD, atherosclerosis was found in 83% patients. Atherosclerosis predisposes to SCAD especially when plaque rupture causes intraluminal thrombosisand creates a deep subintimal dissection followed by intramural hematoma formation, the intima underlying the plaque having either thinned out substantially or in many cases being non-existent. Besides, the inflammatory process associated with an atherosclerotic plaque increases microvessel density and propensity to rupture at the intima-media border and predisposes to a primary intramedial dissection and medial hematoma. Intravascular ultrasound may thus not visualise an intimal tear at all either because the process was primarily that of an intramedial microvessel rupture without intimal tear, or, alternately, because the deep sub-intimal tear associated with the plaque rupture quite often seals up as a result of intraluminal clotting and increased pressure.
Left main stem thrombosis as a result of short term intravenous abuse is even rarer and only a few cases have been reported anecdotally. Steroids are known to alter lipoprotein metabolism, alter endothelium-mediated vascular reactivity, promote platelet aggregation and directly compromise myocyte function.
When intravascular ultrasound is not used during the initial presentation, differentiation between SCAD, steroid-facilitated left main stem artery thrombosis or atherosclerotic plaque rupture can be difficult in a young 21 year old man with no risk factors for coronary artery disease. Even when IVU is used, typical features of SCAD, LMS thrombosis or plaque rupture may not be present, or there might be a combination of findings to confound etiology. Thus intimal dissection might have sealed due to intraluminal clot and pressure and medial hematoma may not be substantial in SCAD, intraluminal clot might be present in SCAD as well as plaque rupture and not just in steroid-provoked LMS thrombosis, and, finally, a ruptured intimal plaque might have distally embolised.
Case Presentation

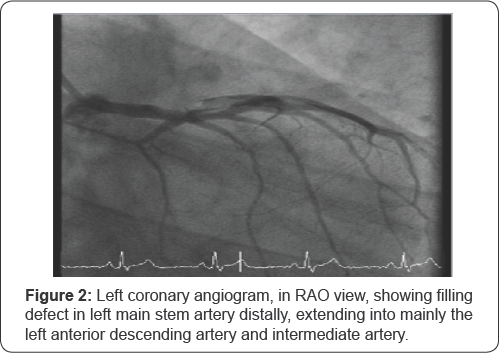
A 23 year old male and former cage fighter was admitted in a peripheral hospital with sudden onset chest pain while playing football. He had no previous history of cardiovascular or connective tissue disease. He smoked 20 cigarettes a day and admitted to the recreational use of steroids for the previous 3 weeks. Physical examination was unremarkable. ECG showed 4mm ST elevation in leads V2 to V6, incomplete RBBB, left posterior fascicular block and high level of troponin I. There was one episode of self- terminating short run of ventricular tachycardia. A diagnosis of anterior ST elevation myocardial infarction was made. He was commenced on aspirin, clopidogrel, bisoprolol and intravenous heparin and transferred for further management to our hospital. Coronary angiogram was done at transfer and this revealed what was initially thought to be a spontaneous coronary artery dissection (SCAD) involving left main stem artery which extended into the LAD and intermediate arteries, visualised as persistent filling defects (Figure 1 & 2). The circumflex and the dominant right coronary arteries were normal. Echocardiogram showed moderately impaired left ventricular function with akinesia of anterior wall and apex. Since the patient was pain-free, he was offered the option of a higher risk immediate surgical revascularisation or a two week delayed CABG, with immediate surgery if symptoms supervened. Patient refused to have immediate surgery. ReoPro bolus and infusion were therefore added with a view to surgery in two weeks' time.
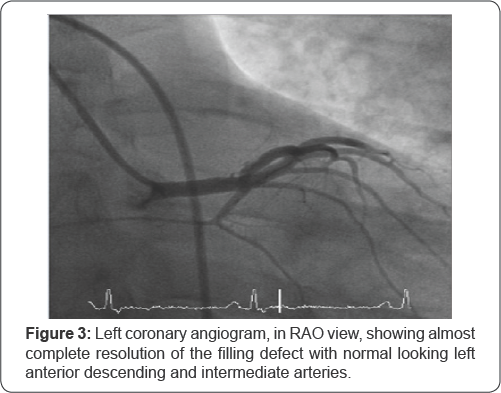

However, repeat angiogram done one week after the initial angiogram showed marked improvement in the appearances of the coronary arteries with only mild residual thrombus in LAD. Intravascular ultrasound (IVUS) confirmed ruptured plaque with intraluminal thrombus. Warfarin was added due to presence of left ventricular thrombus. Patient remained symptom free during his stay and, in view of angiographic findings, it was elected to continue with conservative treatment. He was discharged home 11 days after his initial admission. A repeat coronary angiogram 1 week after his initial presentation had shown significant improvement and 6 weeks later showed normal coronary arteries with no trace of dissection, thrombus or stenosis (Figure 3 &4). Left ventriculogram, however, showed localised apical akinesia and antero and inferobasal hypokinesia with an overall ejection fraction of 30%. There was a small left ventricular thrombus which required warfarinisation. MR scan 6 months later showed considerable improvement in left ventricular function to an ejection fraction of 54% with small localised akinesia in distal LAD territory. At 7 year follow up, patient remains gainfully employed and free of all symptoms.
Discussion
ST elevation myocardial infarction in a 21 year old body builder during a football match, with a recent history of intravenous recreational steroid abuse, in the absence of any known history of risk factors for coronary artery disease, can be due to spontaneous coronary artery dissection [SCAD], primary steroid provoked coronary artery thrombosis or rupture of an unsuspected atherosclerotic plaque, or a combination of the above with even a mild degree of coronary atherosclerosis playing a facilitative role.
Coronary artery dissections can be primary or secondary. Primary dissections occur spontaneously whereas secondary dissections occur either as extensions of aortic dissections [13] or following coronary angiography, coronary intervention, cardiac surgery, or chest trauma [4]. Macroscopically, coronary dissection can take place between intima and media or media and adventitia. Haemorrhage into the false lumen followed by thrombosis results in compromise of the distal blood flow followed by coronary ischaemia [4].
Pretty described the first case of a dissecting aneurysm of a coronary artery in a 42 year old woman in 1931 [5]. Although more than 300 cases have been reported since, majority of cases (70-75%) are diagnosed post mortem [6- 8]. However, as coronary angiography is performed more frequently in acute coronary syndrome, the incidence of spontaneous coronary artery dissection (SCAD) has risen to 0.07% -1.1% in patients referred for coronary angiography [9-15].
The mean age of presentation is 30-45 years and more than 70% patients are women. The prevalence of SCAD, in women below 50 years of age, presenting with acute coronary syndrome and ST elevation myocardial infarction has been described in as many as 8.7% and 10.8% patients respectively [14].
SCAD involves LAD most frequently, in as many as 60% cases, multiple vessels in 20% cases and left main stem in 12% cases [6,9,11,12,15,16]. Spontaneous left main dissection occasionally extends into multiple proximal vessels. Coronary dissections are graded from A to F according to National Heart, Lung and Blood institute classification system as described by the Coronary Angioplasty Registry [16]. Type A represents radiolucent areas with minimal or no persistence after the contrast has cleared. Type B have double lumina with minimal or low persistence. Type C appears as extravasated contrast which persists and Type D as spiral luminal filling defects with extensive contrast staining. Type E dissections appear as new persistent filling defects and Type F cause total occlusion.
The most common pathologies associated with SCAD are coronary atherosclerosis, occurring in 8-28% patients [12,13,17-19] and vascular changes associated with peripartum period in approximately 1/3 of all female patients [9,20,21]. Other conditions include connective tissue disorders like Marfan disease [22], type IV Ehlers-Danlos syndrome [4], Osler-Weber- Rendu disease [23], cystic median necrosis [24], SLE vascultis [4], hypertensive crises [25], intense physical activity [9,25-27], skiing at altitude [28], prolonged sneezing [4], contraceptive usage [29], polycystic kidneys [30], substance abuse including cocaine [4], amphetamines [31], cannabis [32] and alcohol [33,34].
Clinical presentation ranges from incidental angiographic finding, unstable angina, acute myocardial infarction, ventricular arrhythmia to sudden cardiac death [12,15,35]. Badmanaban et al. [35] reported successful surgical revascularisation in a 59 year old man who presented with cardiac tamponade and spontaneous left main dissection [36]. Abdurrahman described thrombotic occlusion of the main stem in a neonate in cardiogenic shock with no left ventricular output and a systemic circulation dependent on flow from a patent arterial duct [37]. Whenever a young patient without major coronary risk factors or a woman in postpartum period presents with unstable angina, acute myocardial infarction or sudden death, SCAD should be kept in mind and coronary angiography undertaken [4].
Coronary angiography, however, needs to be undertaken with great care once SCAD is suspected owing to the risk of further extension of the dissection. The angiographic appearances range from intimal flap with two lumen streaming, intraluminal haziness and filling defects, eccentric narrowing without intimal flap or appearances indistinguishable from an atherosclerotic stenosis. When a typical atherosclerotic stenosis is seen without an intraluminal flap, haziness or filling defects in a young person, in general, and a peripartum female, in particular, an intravascular ultrasound (IVUS) or the newer optical coherence tomogram (OCT) might point towards SCAD. IVUS typically shows little atherosclerosis and intramural hematoma in outer media, intimal tear with its direction and extent, and also helps in the optimal geographical placement of any stents, if required. The newer OCT, on the other hand, provides higher resolution imaging of the intimal tear and intramural hematoma [4]. Coronary CT angiography provides a non-invasive but low resolution assessment of SCAD, in terms of wall thickness or any associated plaques, and, therefore, is better used to follow up patients after SCAD [38].
When there is no evidence of ongoing ischaemia or hemodynamic instability, conservative management with aspirin, clopidogrel, glycoprotein IIb/IIIa inhibitors, anti-ischaemic therapy with beta blockers and nitrates and anti-thrombotic therapy with heparin or low molecular weight heparin has been generally successful [6,11,18,38-40]. Treatment with fibrinolytics is generally avoided because of occasional reports of fibrinoytic induced bleeding into the dissected vessel wall [4]. However, Karaahmet et al. [41] reported regression of spontaneous left main stem dissection with thrombolytic therapy as evaluated by multislice computed tomography angiography. Similarly, Rohit et al. [42] reported conservative management of left main dissection in a 14 year old boy with acute myocardial infarction with left ventricular dysfunction, but with no evidence of reversible ischaemia on myocardial perfusion imaging. Having noticed eosinophilic periadventitial inflammation in 42 cases of peripartum SCAD (in a literature review of peripartum SCAD), Koller et al. [43] added prednisone and cytotoxan to the conventional medical treatment of a 35 year old postpartum woman with SCAD in five non-contiguous coronary arteries. Again, use of a potent anti-thrombotic medication in SCAD might expand the intramural hematoma [4].
PCI or CABG is indicated when significant dissection persists in a major vessel causing marked narrowing or ischaemia. Single vessel dissections of major arteries are managed by PCI. PCI restores flow, seals dissection and relieves ischaemia, although one has to be mindful of advancing the guidewire in the true lumen and not the false lumen and preventing distal dissection or propagation of intramural hematoma, ensured usually by deploying the first stent across the distal border, thus providing adequate coverage of this important area [4].
Left main dissections, multivessel involvement or failed percutaneous interventions are treated with CABG. Unal et al. [44] reviewed the records of 5000 surgical patients over a 6 year old period, and found 6 patients with SCAD. Five patients had LMS dissection and one had right coronary dissection. The patient with right coronary dissection underwent CABG after failed PCI and died 30 days later. Others underwent CABG in the first instant and had good result on short and intermediate term follow up [44]. When SCAD involves a long segment, CABG can be challenging [14]. Conraads et al. [45] described bridging to transplantation after SCAD. Hinojal et al. [46] reported a 31 year old woman with four week postpartum LMS spontaneous coronary dissection with extensive myocardial infarction, severe left ventricular dysfunction and cardiogenic shock who did not improve after urgent coronary revascularisation and required temporary left ventricular support and heart transplantation [46]. Keon et al. [47] successfully treated a 41 year old woman with spontaneous dissection of left main stem artery complicated by myocardial infarction and cardiogenic shock by Jarvik 7-70 artificial heart to sustain life until an orthotopic heart transplant was performed.
SCAD is a lethal disease 75% patients are diagnosed post-mortem [7,8], as the immediate mortality is 50%, with a 20% mortality over the hours following the acute event [11]. However, in-hospital mortality is low, around 3% [6,10,14] and the recurrence rate of SCAD, acute coronary syndrome and mortality after initial survival is low [6,13,14]. In a multivariate analysis of 222 patients, female sex and lack of early, appropriate treatment were the strongest predictors of death, with overall peripartum mortality of 38% [9,35].
Steroids can cause a number of cardiovascular complications including hypertension, cardiomyopathy, stroke, pulmonary embolism, arrhythmias, polycythemia and the resultant increase in plasma viscosity and myocardial infarction [48]. Abdurrahman described thrombotic occlusion of the main stem in a neonate in cardiogenic shock with no left ventricular output and a systemic circulation dependent on flow from a patent arterial duct [37]. There have been a few case reports of myocardial infarction in young adults with anabolic steroid abuse [48-52]. Stergiopoulos et al. [48] reported inferior ST elevation myocardial infarction in a patient with traditional risk factors as well as polycythemia, using supraphysiological doses of supplemental intramuscular testosterone, treated by PCI and phlebotomy.
Halvorsen et al. [49] described acute myocardial infarction due to LAD occlusion in a 27 year old male body builder, treated by PCI with stent and IABP. Again, a 2 year stanzolol abuse seemed to be the only precipitating factor in a young body builder who presented with ventricular tachycardia and stenotic lesions in LAD and right coronary arteries, suggesting an atherogenic response to long term steroid use, in the absence of other risk factors [50]. Godon et al. [51] presented the case of a top class body builder who developed ischaemic cardiomyopathy and inferior wall myocardial infarction following prolonged use of two types of anabolic steroids. Luderwald et al. [52] reported a 2001 German study which showed that 39% of bodybuilders misused anabolic androgenic steroids. Based on 15 autopsies at the Institute of Legal Medicine of the University of Munich, atherosclerotic and thrombotic changes of the heart were especially noticeable. Steroids have been shown to facilitate interstitial endocardial and myocardial fibrosis [49], increase platelet aggregation, promote coronary spasm and exert a direct toxic effect on myocytes [51]. Steroids alter the lipoprotein metabolism by reducing HDL levels and increasing the LDL levels [53]. They increase sympathetic activity [54], compromise flow- mediated, endothelium-dependent vasodilatation [55], promote structural changes including ectasia in coronary arteries and promote intracoronary and ventricular thrombosis and systemic embolism [56].
Our patient, who was a body builder and cage fighter, presented suddenly with ST elevation myocardial infarction while playing a football match. He also gave history of recreational use of intravenous steroids for the previous 3 weeks. Coronary angiogram showed a persistent filling defect in the left main stem extending into the LAD and the intermediate arteries. An intravascular ultrasound was not considered essential at the initial angiogram and the appearances were considered pathognomonic of NHLBI type E dissection characterised by a persistent filling defect. Presence of intraluminal clot and absence of an intimal dissection on intravascular ultrasound may not necessarily have clinched a diagnosis of steroid induced thrombosis of left main stem artery because quite often the intimal or subintimal dissection seals due to intraluminal pressure and clot [4]. Although he was offered surgical revascularisation, he preferred to have delayed surgery and this was acceptable in the presence of resolution of pain and stabilised ECG. Repeat coronary angiography 3 weeks later showing considerable improvement and IVS appearance of primarily intraluminal clot without any significant medial hematoma, albeit in the presence of an atherosclerotic plaque rupture suggested a primary left main thrombosis with some contribution of atherosclerotic plaque rupture, both occurrences perhaps facilitated by the recent intravenous steroid usage.
References
- Kaul P, George R, Paniagua R, Petsa A, Congiu S (2012) Innominate truncal dissection and rupture into right pleural cavity following acute type A dissection of aorta with right coronary ostial avulsion and inferior STEMI. Perfusion 26(5): 435-440.
- Zegers ES, Gehlmann HR, Verheugt FW (2007) Acute myocardial infarction due to an acute type A aortic dissection involving the left main stem coronary artery. Neth Heart J 15(7-8): 263-264.
- Vianna CB, Puig LB, Vieira ML, Shiozaki AA, Dauar ID, et al. (2007) Spontaneous aortic dissection limited to sinus of Valsalva and involving the left main stem artery. Int J Cardiovasc Imaging 23(4): 455-458.
- Vrints CJM (2010) Spontaneous coronary artery dissection. Heart 96(10): 801-809.
- Pretty HC (1931) Dissecting aneurysm of coronary artery in a woman aged 42. BMJ 1: 667.
- De Maio SJ, Kinsella SH, Silverman ME (1989) Clinical course and long-term prognosis of spontaneous coronary artery dissection. Am J Cardiol 64(8): 471-474.
- Jorgensen MB, Aharonian V, Mansukhani P, Mahrer PR (1994) Spontaneous coronary artery dissection: a cluster of cases with this rare finding. Am Heart J 127(5): 1382-1387.
- Thayer JO, Healy RW, Maggs PR (1987) Spontaneous coronary artery dissection. Ann Thorac Surg 44(1): 97-102.
- Thompson EA, Ferraris S, Gress T, Ferraris V (2005) Gender differences and predictors of mortality in spontaneous coronary artery dissection: a review of reported cases. J Invasive Cardiol 17(1): 59-61.
- Pasalodos Pita J, Vazquez Gonzalez N, Perez Alvarez L, Vazquez Rodriguez JM, Castro Beiras A (1994) Spontaneous coronary artery dissection. Cathet Cardiovasc Diagn 32(1): 27-32.
- Zampieri P, Aggio S, Roncon L, Rinuncini M, Canova C, et al. (1996) Follow up after spontaneous coronary artery dissection: a report of five cases. Heart 75(2): 206-209.
- Hering D, Piper C, Hohmann C, Schultheiss HP, Horstkotte D (1998) Prospective study of the incidence, pathogenesis and therapy of spontaneous, by coronary angiography diagnosed coronary artery dissection. Z Kardiol 87(12): 961-970.
- Celik SK, Sagcan A, Altintig A, Yuksel M, Akin M, et al. (2001) Primary spontaneous coronary artery dissections in atherosclerotic patients. Report ofnine cases with review of the pertinent literature. Eur J Cardiothorac Surg 20(3): 573-576.
- Vanzetto G, Berger-Coz E, Barone-Rochette G, Chavanon O, Bouvaist H, et al. (2009) Prevalence, therapeutic management and medium-term prognosis of spontaneous coronary artery dissection: results from a database of 11,605 patients. Eur J Cardiothorac Surg 35(2): 250-254.
- Mortensen KH, Thuesen L, Kristensen IB, Christiansen EH (2009) Spontaneous coronary artery dissection: a Western Denmark Heart Registry study. Catheter Cardiovasc Interv 74(5): 710-717.
- Huber MS, Mooney JF, Madison J, Mooney MR (1991) Use of a morphologic classification to predict clinical outcome after dissection from coronary angioplasty. Am J Cardiol 68(5): 467-471.
- Maehara A, Mintz GS, Castagna MT, Pichard AD, Satler LF, et al. (2002) Intravascular ultrasound assessment of spontaneous coronary artery dissection. Am J Cardiol 89(4): 466-468.
- Aqel RA, Zoghbi GJ, Iskandrian A (2004) Spontaneous coronary artery dissection, aneurysms, and pseudoaneurysms: a review. Echocardiography 21(2): 175-182.
- Angelini P (2007) Spontaneous coronary artery dissection: where is the tear? Nat Clin Pract Cardiovasc Med 4(12): 636-637.
- Kolodgie FD, Gold HK, Burke AP, Fowler DR, Kruth HS, et al. (2003) Intraplaque hemorrhage and progression of coronary atheroma. N Engl J Med 349(24): 2316-2325.
- Rahman S, Abdul-Waheed M, Helmy T, Huffman LC, Koshal V, et al. (2009) Spontaneous left main coronary artery dissection complicated by pseudoaneurysm formation in pregnancy: role of CT coronary angiography. J Cardiothorac Surg 4: 15.
- Thistlethwaite PA, Tarazi RY, Giordano FJ, Jamieson SW (1998) Surgical management of spontaneous left main coronary artery dissection. Ann Thorac Surg 66(1): 258-260.
- Miegham CA, Ligthart JM, Cademartiri F (2006) Images in cardiology. Spontaneous dissection of the left main coronary artery in a patient with Osler-Weber-Rendu disease. Heart 92(3): 394.
- Hirose H, Matsunga I, Anjun W, Strong MD (2009) Spontaneous left main coronary artery dissection, possibly due to cystic medial necrosis found in the internal mammary arteries. Interact Cardiovasc Thorac Surg 9(4): 725-727.
- Iyisoy A, Agac MT, Celik T, Jata B (2010) Spontaneous dissection of left main stem coronary artery associated with hypertensive crises: a probable fatal complication detected by intravascular ultrasound. Int J Cardiol 139(1): e5-e7.
- Marijon E, Fressonet R, Haggui A, Mousseaux E, Redheuil A (2008) Spontaneous coronary dissection of the left main stem after intense physical activity -regression under conservative strategy. Int J Cardiol 128(1): e16-e18.
- Justice LT, Dauterman K, Smedira NG, Moliterno DJ (2005) Left main dissection and thrombosis in a young athelete. Cardiol Rev 13(5): 260262.
- Dworakowski R, Desai J, Maccarthy P (2009) Spontaneous left main coronary artery dissection while skiing at altitude. European Heart Journal 30(7): 868.
- Azam MN, Roberts DH, Logan WF (1995) Spontaneous coronary artery dissection associated with oral contraceptive use. Int J Cardiol 48(2): 195-198.?
- Lee CC, Fang CY, Huang CC, Ng SH, Yip HK, et al. (2011) Computed tomography angiographic demonstration of an unexpected left main coronary artery dissection in a patient with polycystic kidney disease. J Thoracic Imaging 26(1): W4-W6.
- Kanwar M, Gill N (2010) Spontaneous multivessel coronary artery dissection. J Invasive Cardiol 22(1): E5-E6.
- Dwivedi S, Kumar V, Aggarwal A (2008) Cannabis smoking and acute coronary syndrome: two illustrative cases. Int J Cardiol 128(2): e54-e57.
- Pamplona D, Barduca M, Vieira ML, Forlenza L, Cesar LA (1997) Thrombosis in normal coronary arteries causing acute myocardial infarction in an alcoholic patient. Arquivos Brasileiros de Cardiologia 69(3): 185-188.
- Williams MJ, Restieaux NJ, Low CJ (1998) Myocardial infarction in young people with normal coronary arteries. Heart 79(2): 191-194.
- Koul AK, Hollander G, Moskovits N, Frankel R, Herrera L, et al. (2001) Coronary artery dissection during pregnancy and the postpartum period: two case reports and review of literature. Catheter Cardiovasc Interv 52(1): 88-94.
- Badmanaban B, McCarty D, Mole DJ, McKeown PP, Sarsam MA (2002) Spontaneous coronary artery dissection presenting as cardiac tamponade. Ann Thorac Surg 73(4): 1324-1326.
- Abdurrahman L, Scwartz SM, Beckman RH (1999) Thrombotic occlusion of the main stem of the left coronary artery in a neonate. Cardiol Young 9(2): 189-191.
- Satoda M, Takagi K, Uesugi M, Morishima I, Mukawa H, et al. (2007) Acute myocardial infarction caused by spontaneous postpartum coronary artery dissection. Nat Clin Pract Cardiovasc Med 4(12): 688692.
- Arnold J, West N, van Gaal W, Karamitos TD, Banning AP (2008) The role of intravascular ultrasound in the management of spontaneous coronary artery dissection. Cardiovasc Ultrasound 6: 24.
- Sarmento-Leite R, Machado PR, Garcia SL (2003) Spontaneous coronary artery dissection: stent it or wait for healing? Heart 89(2): 164.
- Karaahmet T, Tigen K, Gurel E, Cevic C, Mutlu B, et al. (2009) Spontaneous dissection of the left main coronary artery regressed with thrombolytic therapy: evaluation with multislice computed tomography angiography. Anadolu Kardiyoloji dergisi 9(1): e2-e3.
- Rohit MK, Garg PK, Hariram V, Gupta A, Grover A (2008) Idiopathic spontaneous coronary artery dissection presenting as acute myocardial infarction in a young boy. Indian Heart Journal Indian Heart J 60(4): 346-348.
- Koller PT, Cliffe CM, Ridley J (1998) Immunosuppressive therapy for peripartum-type spontaneous coronary artery dissection: case report and review. Clinical Cardiol 21(1): 40-46.
- Unal M, Korkut AK, Kosem M, Ertunc V, Ozcan M, et al. (2008) Surgical management of spontaneous coronary artery dissection. Tex Heart Inst J 35(4): 402-405.
- Conraads VM, Vorlat A, Colpaert CG, Rodrigus IE, De Paep RJ, et al. (1999) Spontaneous dissection of three major coronary arteries subsequent to cystic median necrosis. Chest 116(5): 1473-1475.
- Hinojal YC, Di Stefano S, Florez S, Martinez G, de la Feunte L, et al. (2004) Spontaneous coronary dissection during postpartum: etiology and controversies in management. Italian Heart Journal 5(7): 563-565.
- Keon WJ, Koshal A, Boyd WD, Lramee L, Farrell E, et al. (1988) Survival after spontaneous primary left main coronary artery dissection. Acute surgical intervention with the Jarvik 7-70 artificial heart. J Cardiovasc Surg (Torino) 30(5): 786-789.
- Stergiopoulos K, Brennan JJ, Mathews R, Setaro JF, Kort S (2008) Anabolic steroids, acute myocardial infarction and polycythemia: a case report and review of the literature. Vasc Health Risk Manag 4(6): 1475-1480.
- Lyngberg KK (1991) Myocardial infarction and death of a body builder after using anabolic steroids. Ugeskr Laeger 153(8): 587-588.
- Mewis C, Spyridopoulos I, Kuhlkamp V, Seipel L (1996) Manifestation of severe coronary heart disease after anabolic drug abuse. Clin Cardiol 19(2): 153-155.
- Godon P, Bonnefoy E, Guerard S, Munet M, Velon S, et al. (2000) Myocardial infarction and anabolic steroid usage: A case report. Arch Mal Coeur Vaiss 93(7): 879-883.
- Luderwald S, Zinka B, Thieme D, Eisenmenger W (2008) Misuse of anabolic steroids. Fatal cases in recreational bodybuilding. Rechtsmedizin 18: 183-188.
- Glazer G (1991) Atherogenic effects of anabolic steroids on serum lipid levels: A literature review. Arch Intern Med 151(10): 1925-1933.
- Gauthier J (2001) Cardiovascular effects of doping. Ann Cardiol Angeiol (Paris) 50(5): 293-298.
- Ebenbichler CF, Sturm W, Ganzer H, Bodner J, Mangweth B, et al. (2001) Flow-mediated, endothelium-dependent vasodilation is impaired in male body builders taking anabolic steroids. Atherosclerosis 158(2): 483-490.
- Tischer KH, Heyney-Von Haussen R, Mall G, Doenecke P (2003) Coronary thrombosis and ectasia of coronary arteries after long term use of anabolic steroids. Z Kardiol 92(4): 326-331.






























