Cardiac Arrest as a First Presentation of Chronic Total Occlusion of Left Main Coronary Artery- Case Report and Literature Review
Habib Habib1, Amer Hawatmeh2*, Zaid Altheeb3, Dema Shamoon1 and Fayez Shamoon1
1Department of Cardiology, St. Joseph medical center, USA
2Department of Cardiology, Saint Michael's Medical Center, USA
Submission: March 19, 2017; Published: June 05, 2017
*Corresponding author: Amer Hawatmeh, Department of Cardiology, New York Medical College, Saint Michael's Medical Center, 111 Central Avenue, Newark, New Jersey 07102, USA, Tel: +1 (973) 877 5000; Fax: +1 (973) 877-5124; Email: amer_hawatmeh@hotmail.com
How to cite this article: Habib H, Amer H, Zaid A, Dema S, Fayez S. Cardiac Arrest as a First Presentation of Chronic Total Occlusion of Left Main Coronary Artery- Case Report and Literature Review. J Cardiol & Cardiovasc Ther 2017; 5(5): 555672. DOI: 10.19080/JOCCT.2017.05.555672
Abstract
Complete occlusion of left main coronary artery (LMCA) is an unusual manifestation of coronary atheromatous disease. Most patients with chronic total occlusion of the LMCA presents with angina, some presents with myocardial infarction or congestive heart failure, but they rarely present with cardiac arrest and survive. Here, we report a rare case of chronic total occlusion of the LMCA who presented with cardiac arrest as a first manifestation of coronary artery disease. Our case is interesting as this patient didn't have any risk factors for coronary artery disease, had no angina symptoms before presentation, and had normal left ventricular systolic function.
Keywords: Chronic total occlusion; Left main coronary artery; Cardiac arrest
Introduction
Complete occlusion of left main coronary artery (LMCA) is an unusual manifestation of coronary atheromatous disease. The incidence of total occlusion of LMCA has been reported to be 0.04-0.4% in angiography series [1]. In such patients, collaterals arising from right coronary artery are essential for patient survival.
Most patients with chronic total occlusion (CTO) of the LMCA presents with angina (stable or unstable), some presents with myocardial infarction or congestive heart failure, but they rarely present with cardiac arrest and survive.
Here, we report a very rare case of chronic total occlusion (CTO) of the LMCA who presented with cardiac arrest as a first manifestation of coronary artery disease. Our case is interesting as this patient didn't have any risk factors for coronary artery disease, and didn't have any angina symptoms before this presentation. In addition she was found to have normal LV function.
Case Presentation
A 50 year-old female with a past medical history significant only for uterine fibroids presented to the emergency department (ED) after a sudden cardiac arrest. She was resuscitated in the field, and one shock was delivered by automated external defibrillator after that she had return of spontaneous circulation and was transferred to our hospital.
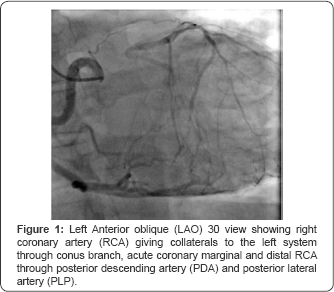
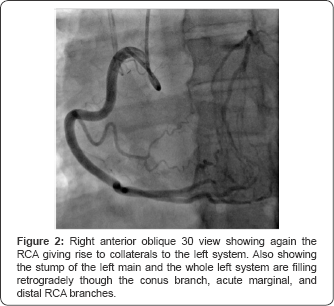
In the ED physical examination revealed blood pressure of 105/54mmHg, heart rate of 90 beats/min, normal heart sounds without any murmur or additional sounds. Lungs were clear to auscultation and there was no peripheral edema. Electrocardiogram revealed sinus tachycardia at ventricular rate 103 beats/min with no ST segment deviations or T-wave inversions. Serial troponins were elevated (highest was 1.13ng/ mL) and chest X-ray was unremarkable. Patient was extubated the following day with return to baseline cognitive function, reported no anginal symptoms prior to cardiac arrest, nor any cardiovascular risk factors. On echocardiogram ejection fraction was estimated at 55-60% without diastolic dysfunction, abnormal wall motion or significant valvular findings. During her hospital stay the patient underwent left heart catheterization through the radial approach. Angiography revealed 100% occlusion of the left main coronary artery at its stump, with collaterals provided by a dominant right coronary artery (Figure 1 & 2).
Given these findings in the setting of sudden cardiac arrest, the patient was deemed a candidate for coronary revascularization. During hospitalization her hemoglobin level dropped to 5.9g/dl secondary to bleeding uterine fibroids, and she refused blood transfusions based on her religious beliefs. Coronary artery bypass graft surgery (CABGS) was discussed with the patient; however patient was deemed unsuitable by cardiothoracic surgery given the severity of anemia. Patient underwent a successful uterine artery embolization and her vaginal bleeding was controlled thereafter. She was treated with intravenous iron infusion, erythropoietin, multivitamin, folic acid and cyanocobalamin. Bloodless medicine measures were taken in attempt to raise hemoglobin to optimize patient for CABGS, and successfully raised her hemoglobin to >13g/dl. Patient subsequently was transferred for CABGS in a bloodless surgical facility, underwent the procedure without complications, and discharged home.
Discussion
Total left main coronary artery occlusion can be either acute or chronic. Acute total LMCA occlusion is usually associated with higher mortality, presenting with extensive acute myocardial infarction, cardiogenic shock or sudden cardiac death [2]. Chronic total LMCA occlusion is typically associated with exertional angina pectoris, myocardial infarction or congestive heart failure.
The largest analysis of patients with complete occlusion of the left main coronary artery was performed by Kanjwal et al. [3] and included 60 cases described between 1966 and 1998. In this series, 85% of patients were male, and their ages ranged from 25 to 74 years. The most common presenting complaint was also chronic or unstable angina. However, the analysis did not elucidate specific risk factors that would increase a patient's likelihood for developing total occlusion of the left main coronary artery [3].
In patients with total occlusion of the LMCA, collaterals arising from right cor-onary artery are essential for both patient survival and maintenance of left ventric-ular global function [4]. In an angiographic study of 6 patients with LM-CA occlusion, 13 specific collateral chan-nels were identified. The conus branch and anterior and posterior septal branch-es were the most common vessels partic-ipating in the formation of collaterals [5]. Clearly, these patients are candidates for massive myocardial infarction and sudden death, and most of them require urgent or emergency coronary bypass surgery. Although some of the patients with this lesion may require balloon counter pulsation during the perioperative period, many can be managed without such support, as long as hemodynamics are carefully monitored and adjusted with aggressive pharmacologic support, as in the case we present [6].
Since the first clinical description of LMCA disease by Herrick in 1912 [7], numerous studies have shown that stenosis of LMCA is of critical prognostic importance, and reports of medically and surgically treated patients support the widely accepted belief that CABG surgery decreases patients' symptoms and significantly prolong their survival [8]. Joong et al. [9] reported two cases of chronic LMCA total occlusions and their long-term survival after successful surgical management. However, the latest European Society of Cardiology (ESC) and the European As-sociation for Cardio-Thoracic Surgery (EACTS) guide-lines on myocardial revascularization ac-cept percutaneous coronary intervention (PCI) as a reasonable alternative for stable pa-tients with suitable coronary anatomy but additional large clinical trial data are required to more definitively determine CTO revascularization guidelines [10].
In Japanese literature there are a few reports of chronic total occlusion of LMCA in patients with normal LV motion and minimal symptoms on presentation [11]. Our case is interesting because this patient had no risk factors for cardiovascular disease, had no angina symptoms and her initial presentation was a cardiac arrest. Her coronary angiography showed isolated chronic total occlusion of LMCA. Furthermore, our case was challenging as the patient was profoundly anemic and had to be managed without using donated blood products.
References
- Zimmern SH, Rogers WJ, Bream PR, Chaitman BR, Bourassa MG, et al. (1982) Total occlusion of the left main coronary artery: the Coronary Artery Surgery Study (CASS) experience. Am J Cardiol 49(8): 20032010.
- Yamane M, Inoue S, Yamane A, Kinebuchi O, Yokozuka H (2005) Primary stenting for left-main shock syndrome. Eurolntervension 1(2): 198-203.
- Kanjwal MY, Carlson DE, Schwartz JS (1999) Chronic/Subacute total occlusion of the left main coronary artery; a case report and review of the literature. Angiology 50(11): 937-945.
- Goldberg S, Grossman W, Markis JE, Cohen MV, Baltaxe HA, et al. (1978) Total occlusion of the left main coronary artery. A clinical, hemodynamic and angiographic profile. Am J Med 64(1): 3-8.
- Topaz O, DiSciascio G, Cowley MJ, Lanter P, Soffer A, et al. (1991) Complete left main coronary artery occlusion: angiographic evaluation of collateral vessel patterns and assessment of hemodynamic correlates. Am Heart J 121(2 Pt 1): 450-456.
- Trnka KE, Febres-Roman PR, Cadigan RA, Crone RA, Williams TH (1980) Total occlusion of the left main coronary artery: clinical and catheterization findings. Clin Cardiol 3(5): 352-355.
- Herrick JB (1912) Clinical features of sudden obstruction of the coronary arteries. JAMA 23: 2015-2020.
- Caracciolo EA, Davis KB, Sopko G, Kaiser GC, Corley SD, et al. (1995) Comparison of surgical and medical group survival in patients with left main coronary artery disease. Circulation 91(9): 2325-2334.
- Choh JH, Wang T, Golbus GA, Leskovac TM, Nazarian A, et al. (1984) Survival with Total Occlusion of Left Main Coronary Artery. Tex Heart Inst J 11(1): 64-68.
- Sugishita K, Shimizu T, Kinugawa K, Harada K, Ikenouchi H, et al. (1997) Chronic total occlusion of the main coronary artery. Intern Med 36: 471-478.
- Wijns W, Kolh P, Danchin N, Mario CD, Falk V, et al. (2010) Task force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS); European Association for Percutaneous Cardiovascular Interventions (EAPCI), Guidelines on myocardial revascularization. Eur Heart J 31(2): 2501-2555.






























