Vascular Plug Embolization Therapy for an Unusual Pelvic Arteriovenous Malformation in a Young Adult
Keyur Vora*
CARE Hospitals, Institute of Medical Sciences, India
Submission: January 27, 2016; Published:February 09, 2017
*Corresponding author: Keyur Vora, MD MSCR, CARE Hospitals, Institute of Medical Sciences, Surat, Gujarat, India, Email: drkeyurvora@gmail.com
How to cite this article:Keyur V. Vascular Plug Embolization Therapy for an Unusual Pelvic Arteriovenous Malformation in a Young Adult. J Cardiol & Cardiovasc Ther 2017; 3(1): 555608. DOI: 10.19080/JOCCT.2017.03.555608
Abstract
The management of pelvic arteriovenous malformations (AVMs) remains challenging due to extensive muscle plane involvement, higher probability of incomplete surgical resection and high recurrence rate. This report describes the case of a 24-year-old male with AVM in the left gluteal region. Vascular surgery would have involved widespread muscle debulking and extensive bleeding. So embolotherapy was preferred over surgical therapy to block the blood flow into the nidus of the AVM. The malformation was successfully treated with no recurrence after 1 year. Peripheral AVMs demands multidisciplinary approach that integrates surgical therapy with embolotherapy. However, embolotherapy can be exclusively developed to improve the outcomes in unusual pelvic AVMs with very low morbidity and no recurrence.
Keywords: Arteriovenous malformation; Embolotherapy; Amplatzer Vascular Plug
Abbrevations: AVMs: Arterio-Venous Malformations; AVP: Amplatzer Vascular Plugs; JR: Judkin’s Right
Introduction
Arteriovenous malformations (AVMs) are vascular anomaly characterized by abnormal connection between arteries and veins, bypassing the capillary system [1]. Peripheral congenital AVMs are uncommon clinical entities that can be progressive in nature, particularly during adolescence. Specifically, pelvic AVMs are rare vascular pathology that remains challenging to accurately diagnose and successfully treat [2]. Diagnostic problems include poor perception of visceral extension and precise localization [3]. Symptoms can become debilitating and fatal if not treated well advance [4]. The management of AVMs remains challenging because of their unpredictable behavior and high recurrence rate [2]. In view of high bleeding risk during surgery, numerous embolic materials have been developed, ranging from simple gelfoam pledgets to complex systems employing micro catheters and detachable coils [3]. However, thorough annihilation of the nidus of an AVM is the only potential cure. Newer embolic vascular devices like Amplatzer Vascular Plugs (AVP) are now being investigated as an adjunctive or alternative embolic therapy for treatment of unusual vascular pathologies like pelvic AVMs.
Clinical Summary
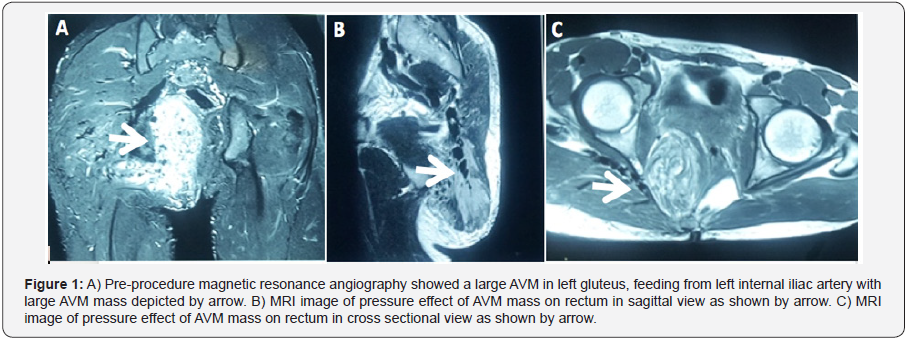
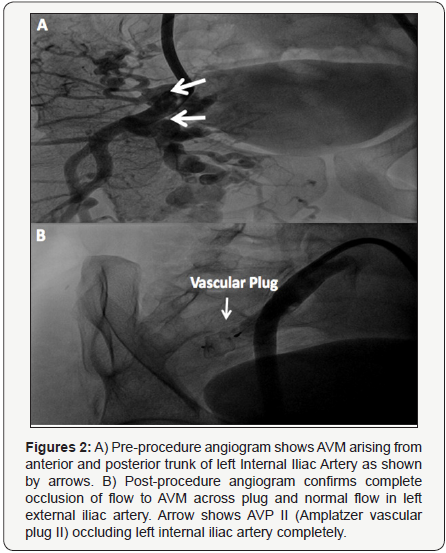
A 24-year-old male patient presented with a large (appx. double the size of right gluteus) swelling at left gluteus. Swelling was present since birth but increased since early adolescence. In addition to cosmetic deformity, patient also experienced difficulty in defecation due to external compression from expanding swelling over rectum and anal canal. Auscultatory examination reveals soft continuous shuffling sound over swelling. With consideration of non-malignant vascular pathology, patient underwent Magnetic Resonance Angiography study which revealed large AVM originating from left internal iliac artery (Figure 1A) with direct pressure effect on rectum and anal canal as shown in sagittal sectional view (Figure 1B) and cross sectional view (Figure 1C). Additionally, peripheral angiogram confirmed arteriovenous malformation arising from anterior and posterior trunk of left internal iliac artery (Figure 2A). Vascular surgery was not considered as it would have involved widespread muscle debulking and extensive bleeding. Notably, high recurrence rate is also not uncommon for AVMs. So nontraditional embolization therapy with vascular plugging was considered.
Procedure Details
Angiograms were reviewed for identification of the target vessel and for other procedural details. Right SFA was cannulated using 6F sheath. Using Judkin’s right (JR) guide catheter (Cordis Corporation, Miami, FL) and 035 Terumo wire (Terumo Medical Corporation, Somerset, NJ, USA), the left internal iliac artery was selectively engaged. The 6F sheath was exchanged with long 9F sheath. The device size was selected based on the most restrictive diameter along the length of the left internal iliac artery. We oversized the AVP by 30-50%, relative to the size of the native vessel as an oversized AVP tends to lengthen significantly. 22 mm AMPLATZER Vascular Plug II (St. Jude Medical, Inc., Minnesota, USA) was deployed across left internal iliac artery after carefully measuring the diameter (16 mm) and length of vessel. An adequately oversized device that had deformed and produced a near complete occlusion of flow suggests a tight fit and negligible chance of embolization, even in very high flow situations [4]. Check angiogram showed no flow across the vascular plug with normal flow in external iliac artery (Figure 2B). Angiogram evidence of absence of flow in the AVM demonstrated total occlusion prior to the release of AVP. The ratio of thedevice-to-vessel diameter was 1.375.
Results

Immediate post procedure, approximately 75% swelling was reduced in 3 hours. Post-procedure angiogram reveals no visible vascular mass. Any signs of periprocedural complications including device deployment failure, device malposition, migration or embolization, stroke, bleeding or any other vascular complication related to the access site were closely monitored. Patient had constipation and mild per rectal bleeding for next 36 hours which could be due to capillary leak from immediate decompression post-procedure. Patient was kept on intravenous nutrition and frequent enema for 48 hours after procedure. Patient was discharged after 72 hours and kept on antibiotic and anti-inflammatory medication support for a week. Upon follow up after 2 weeks, 1, 3, 6 and 12 months, patient was asymptomatic and no signs of recurrence noted on examination.
Discussion
The current management of AVMs based on the new concept of a multidisciplinary approach can minimize the morbidity and reduce the recurrence of the lesion. All treatments, whether involving surgery, radiation, or drugs, have risks and side-effects. Total excision of AVMs leads to a cure; however, total excision is not adequate in cases of AVMs involving the joints and muscle planes [5]. Recurrence of the AVM is common with incomplete resection [6]. Especially, vascular malformations in pelvic region are challenging for therapeutic management. Surgical proximal ligation of a feeding vessel may in fact be contraindicated, because it can make subsequent transcathetertherapy impossible [7].
There has recently been further expansion of the limited role of embolotherapy as an adjunctive therapy for surgical resection. This approach has even been helpful in high-risk lesions with high-flow status [7]. Permanent occlusive agents like isobutyl cyanoacrylate, particles of polyvinyl alcohol foam, and coils have been used to embolize the multiple feeding vessels and even the nidus of the AVM, whenever possible. However, recurrence of symptoms and necessity for repeat embolization has been reported with these devices [8]. With expanding applications in embolotherapy, the Amplatzer series of vascular plugs are very advantageous in the closure of a wide spectrum of abnormal vascular communications with high technical success and low complication rates [9]. High efficiency, lower profile, diverse designs, reduced radiation exposure, reduced procedure times, controlled deliverability with high precision and costeffectiveness makes them an ideal choice for occluding various abnormal congenital vascular communications (St. Jude Medical, Inc. Minnesota USA).
Conclusion
The treatment of pelvic AVMs is a challenging topic for vascular surgeons. Multidisciplinary treatment may offer superior results. To minimize the complications associated with surgery, aggressive control of blood flow is vital, and could be pliable with a chance of cure. Our case experience of using Amplatzer Vascular Plug has shown that transcatheter embolization plays a substantial role in, and may be the treatment of choice for, symptomatic pelvic vascular malformations. Although it is demanding to outline indications, comprehensive and one-stage treatment is the ideal therapy. Extensive clinical trials are needed to understand the definitive role of vascular plug embolotherapy as a curative treatment of AVMs.
References
- Szajner M, Roman T, Markowicz J, Szczerbo-Trojanowska M (2013) Onyx® in endovascular treatment of cerebral arteriovenous malformations - a review. Pol J Radiol 78(3): 35-41.
- Lee BB, Do YS, Yakes W, KimDI, Mattassi R, et al. (2004) Management of arteriovenous malformations: a multidisciplinary approach. J Vasc Surg 39(3): 590-600.
- Laurian C, Leclef Y, Gigou F, Alzaoubi I, Riche MC, et al. (1990) Pelvic arteriovenous fistulas: therapeutic strategy in five cases. Ann Vasc Surg 4(1): 1-9.
- JC Palmaz, TH Newton, Reuter SR, JJ Bookstein (1981) Particulate intraarterial embolization in pelvic arteriovenous malformations. AJR Am J Roentgenol 137(1): 117-122.
- K Igari, T Kudo, T Toyofuku, Jibiki, YInoue (2013) Surgical Treatment with or without Embolotherapy for Arteriovenous Malformations. Ann Vasc Dis 6(1): 46-51.
- K Igari, T Kudo, T Toyofuku, Jibiki, YInoue (2012) Multidisciplinary Approach to a Peripheral Arteriovenous Malformation. European Journal of Vascular and Endovascular Surgery 23(2): e11-e13.
- Wang W, Li H, Tam MD, Zhou D, Wang DX, et al. (2012) The amplatzer vascular plug: a review of the device and its clinical applications. Cardiovasc Intervent Radiol 35(4): 725-740.
- Widlus DM, Murray RR, White RI, Osterman FA, Schreiber ER, et al. (1988) Congenital arteriovenous malformations: tailored embolotherapy. Radiology 169(2): 511-516.
- Parag B, Sivasubramanian R, Shyam SK, Anita S, Saurabh KG, et al. (2013) Amplatzer Vascular Plugs in Congenital cardiovascular Malformations. Ann Pediatr Cardiol 6(2): 132-140.






























