Preoperative Serum NT-proBNP levels; Can it be a Clue About Postoperative Clinical Outcome of Patients Undergoing to Coronary Artery Bypass Surgery?
Mustafa Kemal AVŞAR* and Hafize YALINIZ
Department of cardiovascular surgery, Medicana International Istanbul Hospital and Istanbul Gelisim University, Turkey
Submission: October 17, 2016; Published: October 31, 2016
*Corresponding author: Mustafa Kemal AVŞAR, Medicana International Istanbul Hospital Cardiovascular surgery department and Istanbul Gelisim University, Turkey, Tel: 9005324427701, Email: mustafakemalavsar@hotmail.com
How to cite this article: Mustafa K A, Hafize Y. Preoperative Serum NT-proBNP levels; Can it be a Clue About Postoperative Clinical Outcome of Patients 006 Undergoing to Coronary Artery Bypass Surgery? . J Cardiol & Cardiovasc Ther. 2016; 1(5): 555573. DOI: 10.19080/JOCCT.2016.01.555573
Abstract
Introduction:Brain natriuretic peptid (BNP) is a ventricular hormone that is sensitive and specific marker of changes in ventricular function. It is sample screening test for symptomless left ventricular failure. The aim of this study was examine there is a corelation between the preoperative plasma level of BNP and early morbidity in patients undergoing to coronary artery bypass. Materials and Method:During the 11 month period, we retrospectively evaluated 22 consecutive patients who was operated on for coronary artery bypass. Patients had not have other system and cardiac disease and had not EF ≤ 50. Preoperative plasma BNP values was statisticaly compired with early postoperative morbidity findings. BNP analysis was made by Electrohemoluminescent immunassay method and Roche Diagnostic Indianapolis, Indiana proBNP Elecsys 1010 autoanalyzer with tecnique and ≥125 pg/ml was accepted sign for cardiac function disorder. Postoperative morbidity criterias were accepted as; staying longer than 4 day in intensive care unit and longer than 10 days in hospital, mechanic ventilatory support longer than 48 hours, necessity for inotrops or IABP(intra aortic baloon pump) support. All analysies were done by using SPSS 9.0 statistical software pocket. One or more of above criterias for morbidity are established in 12 of 22(%54) patients. Results:There were no significant differance for demografic findings between the patients who morbidity were established and was not. Preoperative plasma BNP level was 763±53 pg/ml in 12 patients with morbidity while 113±47 pg/ml among 10 patients with no morbidity(P <0.05). Conclusion:n:With the results it is concluded that preoperative plasma BNP levels is a reliable indicator for early postoperative morbidity in patients undergoing coronary artery bypass. Keywords:Cardiopulmonarybypass; BNP(Brain Natriuratic Peptid); Postoperative morbidity Abbreviations:ANP: Atrial Natriuretic Peptide; BNP: Brain Natriuretic Peptide; CNP: C-type Natriuretic Peptidine; EF: Ejection Fraction
Introduction
It was raised about 50 years ago that heart had a natriuretic endocrine effect and in fact, it was stated that heart was an endocrine organ. Attention was drawn that this effect appeared as a result of the distention of atria [1], it was determined that there were intracellular granules similar to endocrine cells on the walls of atria by electron microscope [2], that the active substance was a peptide and this substance, which had the characteristics of a hormone, was named the “atrial natriuretic peptide” (ANP) [3]. Subsequently, in 1988, Sudoh et al. [4] demonstrating the existence of an ANP like natriuretic peptide have called it “brain natriuretic peptide” (BNP). In subsequent studies, it was demonstrated that BNP was a homologue of ANP, was synthesized in the ventricular myocard cells and shared the same periphery receptors as ANP [5].
“C-type natriuretic peptidine (CNP), on the other hand, which is yet another natriuretic peptide is believed to have a minimum effect on cardiac functions and operates by a different mechanism [5]. It has been demonstrated that natriuretic peptides decreased myocardial “preload” and “afterload”, improved ventricular functions, expanded the coronary arteries, reducing myocardial ischemia originating from exercise and that they had a protective effect on myocardial “remodeling” post-myocardial infarctus [5]. In consequence, it is known that myocardial origin peptides achieve natriuresis by an endocrine function and they have an effect on cardiac functions. Specifically, this effect of BNP which is secreted from ventricular myocardium has been proven. Still, the significance of the serum levels of this peptide, pre and post arterial bypass grafting is not yet clear.
The purpose of this retrospective study is to investigate whether the preoperative serum BNP level may be an indicator in terms of adverse clinical findings (morbidity) which may be faced in the early postoperative period in patients to undergo coronary bypass surgery, employing a pump. The values assumed to be normal for serum BNP level varies depending on the type of natriuretic peptide and the selected patient group. In cases where the measured serum NTproBNP value is under 125 pg/ml in patients evaluated in respect of chronic heart failure, the diagnosis of heart failure is doubtful and in great probability, cardiac dysfunction will be excluded (negative diagnostic value ≥% 97)[6,7]. (cardiac dysfunction must be considered if NTproBNP value is over 125 pg/ml) [6,7].
While for patients presenting to emergency units with shortness of breath, the diagnosis of heart failure is considered under 300 pg/ml, looking at the NT-proBNP serum level for diagnosis of acute heart failure, heart failure must be considered between 300-1800 pg/ml and the diagnosis of heart failure becomes conclusive over 1800 pg/ml [8]. There are certain cases where BNP is high although there is no chronic heart failure. These are advanced age, female gender, kidney failure, acute myocard infarctus, lung diseases affecting right heart functions and pulmonary embolism. However, there are times when the serum BNP level is normal despite the existence of heart failure. These conditions are flash lung eudema, NYHA class 1 patients with low EF and mitral stenosis, atrial myxoma and acute mitral failure which cause heart failure without ventricular dysfunction [9].
Currently, there are three different laboratory tests recommended for heart failure by FDA. The first one is the Triage BNP test determining BNP concentration in human plasma implemented in 2000 (Biosite Diagnostics, San Diego, CA). Result is achieved in 15 minutes by the Florescene method. This test was used in certain recent studies. The second test is Shionogi BNP test. This test has been used in previous studies but time of essay is as long as 20 hours. This method has been FDA approved in 2003 (Bayer Diagnostics)[10]. FDA has approved a new test measuring BNP’s N-terminal fragment in 2002 (Elecsys® proBNP, Roche Diagnostics). Under this measuring system, the NT-proBNP (1-76) reading is taken.
In studies performed, NT-proBNP reading and BNP reading have given similar results. BNP is eliminated rapidly from the serum with the aid of natriuretic peptide receptor-C and endopeptidase. NT-proBNP, on the other hand, has a longer lasting and stable serum level with no variations in day or night time. Furthermore, this test may be run quite rapidly. However, the most important problem with this test is that it is less useful compared to BNP in patients with poor kidney functions since NT-proBNP is mostly eliminated through the renal tract.
Patients and methods
Patient group:Twenty-two patients who underwent coronary bypass surgery due to coronary arterial disease between April 2004-March 2005 at Çukurova University School of Medicine Cardiovascular Surgery Main Scientific Discipline were included in the study; 16 patients were male, 6 patients werefemale with an average age of 58.7 ± 7.9 years. From amongst patients admitted for coronary bypass procedure, 22 patients with;
- Left ventricular ejection fraction (EF) is over 50%
- No advanced renal failure (serum creatinine<2.0mg/ dl)
- No thyroid dysfunction (hyperthyroidism, hypothyroidism)
- No chronic obstructive pulmonary disease, Chronic Bronchitis, no pulmonary embolism history, no primary pulmonary hypertension (normal respiratory function tests)
- no right or left heart failure or functional capacity restricting valve disease alongside of coronary arterial disease and no arrhythmia like atrial fibrillation or frequent ventricular ectopic beats were included in the study.
Method
Routine procedures were implemented in the preoperative period for all coronary artery patients: The medical histories of patients were compiled and their physical exams were performed. Risk factors like hypertension, diabetes mellitus, hyperlipidemia, smoking and history of heart disease in the family were noted, electrocardiograms, telecardiograms and echocardiograms (M mode and tissue Doppler) of patients were taken and full blood count, urine analysis, fasting blood sugar, serum electrolytes, serum lipids and renal and liver function tests were performed.
For identifying any adverse clinical findings (morbidity) after operation, the patients were monitored 30 ± 5 days on the average during the post-operative period. In the study, the preoperative BNP values were compared to the preoperative echocardiogram findings and surgery data (cardiopulmonary bypass time spans, cross clamp period and number of anastomosis). In this study, morbidity was taken as stay over 4 days in intensive care and more than 10 days in hospital, mechanical ventilator need over 2 days, inotropic support, intra-aortic balloon pump need and recurring hospital admission. From all patients after a resting period of twenty minutes, 10 ml blood specimen was taken from the antecubital vein into EDTA tubes for measuring NT-proBNP.
Right after the conclusion of symptom limited stress test (within first 1-2 minutes), blood specimens were taken once again similarly for measurement of NT-proBNP. Specimens were centrifuged for 5 minutes at + 4 Co at 1500 rpm and the upper phase plasma segment was transferred into another tube for NTproBNP measurement. The NT-proBNP level was measured from the separated serum by the electrochemoluminescent immunoassay method and Roche Diagnostics (Indianapolis, Indiana) proBNP commercial kits using Elecsys® 1010 autoanalyzer. All patients and controls were advised about the study and their approved consent forms were collected. The study was certified by Çukurova University School of Medicine Board of Ethics.
Anaesthesia and coronary by-Pass technique:
anaesthesia procedure, after EKG, pulse oximeter, peripheric vein and invasive arterial monitorization, induction was performed and intubation carried out with 0.1 mg/kg diazepam, 0.1 mg/ kg pancuronium ve 8-10 μg/kg fentanyl and a central venous catheter was placed in V. Jugularis Interna. Maintenance of anaesthesia was achieved by 60% 02 and air mixture sevoflurane, pancuronium and where necessary, fentanyl. After 3 mg/kg heparin was given, CPB was started. Following application of the aortic cross clamp, heart was stopped by blood cardioplegia (30 mEq K+, 10 mEq NaHCO3, 12 mEq Mg++ in 1000 cc blood). Slight hypothermia was achieved. Myocardial protection was provided by antegrade isothermic blood cardioplegy. Neutralization was done by protamine during exit from CPB. The patients were taken to the intensive care unit in intubated state.
Statistical analyses:All analyses were performed using the SPSS 9.0 statistical software package. The continuous variables in group data were expressed as average ± standard deviation (avg. ± SS). Categorical variables, on the other hand, were given in numbers and percentages. In intergroup univariate comparisons, in independent groups, parametric tests, t tests and variance analyses and non-parametric tests Mann Whitney U test and Kruskall Wallis tests were employed depending on the distribution of continuous variables. In comparison of categorical variables, the Chi-Square test was employed.
In determining the factors affecting morbidity, multivariate logistic regression analysis was performed with variables found to be significant as a result of univariate analyses. The increase or decrease in the risk was stated with Odds Ratio according to the unit increase in the variables found to be significant as a result of this analysis. ROC analysis was used for determining the “cut off” for parameters identifying the progression of cardiac incident independently. p<0.05 was used for statistical significance.
Morbidity related findings:In the postoperative 30 ± 5 day monitoring of the 22 patients who underwent coronary arterial by-pass, postoperative morbidity and incidents were observed in 12 patients (54.5%). IABP need was 2, need for mechanical ventilator over 2 days was 4, positive inotropic support need was 2, discharge after 10 days was 7, and more than 4 day intensive care stay was in 8 patients. In more than one patient, two or three parameters were observed together.
Clinical and demographic characteristics of patients with and without morbidity:No significant difference could be found between the clinical and demographic characteristics of patients with and without morbidity. Upon evaluation of medications received by patients in the preoperative period, it was found that use of beta blockers and statin was low in patients in whom morbidity was observed and that inotropic support need was greater although this was not significant. It was found that only the rate of use of beta blockers was statistically significant between the two groups out of these parameter
Upon evaluation of the preoperative laboratory data of the patients, it was found that in patients with morbidity, the urea and creatinine values were significantly higher than that of the control group and the hemoglobin, hemotocrite and HDL cholesterol values were significantly lower. Evaluation of the postoperative laboratory data of the patients showed that similarly to preoperative values, in patients with morbidity; urea, creatinine and CRP values were significantly higher compared to the control group and hemoglobin, hemotocrite and HDL cholesterol values were significantly lower
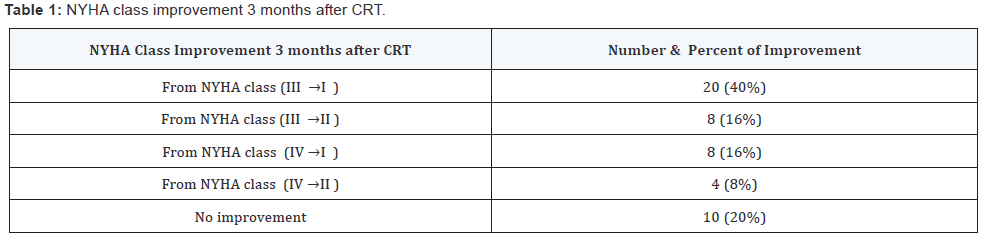
In comparison of the NT-proBNP values of patients with and without morbidity, it was found that in the patient group with morbidity, the preoparative NTproBNP levels were found to be significantly higher statistically compared to those with no morbidity. Postoperative NT-proBNP, absolute and relative NTproBNP difference values, on the other hand, were found to be similar in the two groups. The preoperative and postoperative values of patients with and without morbidity and the absolute and relative NTproBNP difference values derived from such value differences are shown (Table 1).
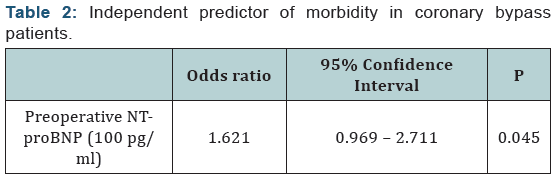
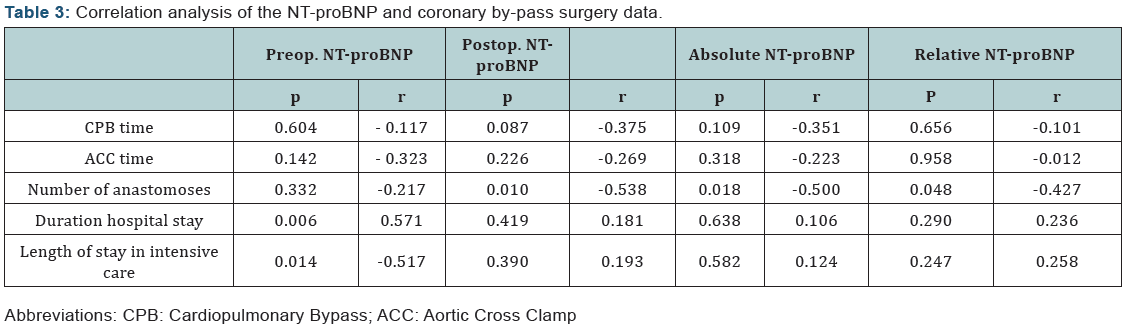
coronary bypass patients by logistic regression analysis, it was found that only the preoperative NT-proBNP level was related to morbidity independent of other parameters (Table 2). Based on Odds ratios, it was determined that each 100 pg/ml increase in preoperative NT-proBNP increased the morbidity risk of the individual by 62.1%. In the ROC analysis performed for the relationship between the preoperative NT-proBNP level and morbidity of coronary bypass patients, it was found that the area under the line in the ROC curve was 75.7%. In this analysis, it was found that the “cut-off” value of 180 pg/ml which is the average NT-proBNP value of all patients predicted morbidity at 73% sensitivity and 69% specificity. No significant relationship could be determined between the coronary by-pass CPC and ACC times and the Nt-proBNP serum levels. There was a negative and significant relationship between the number of anastomosis and all three NT-proBNP levels other than the preoperative NTproBNP. Positive significant relationship was found between the time of stay in hospital and intensive care and only the preoparative NT-proBNP level (Table 3).
Discussion
After it was established that the heart also has an endocrine function, playing a role in secretion of natriuretic peptide, broad studies were performed on the effects of natriuretic peptides. Chello et al. [11] have stated that in patients with left ventricular dysfunction, the preoperative BNP values are correlated with the severety of the left ventricular dysfunction and were the predictors of to what level the left ventricular functions can improve after a coronary artery by-pass procedure. In this study, a reduction in parallel with the improvement in the left ventricular function has been determined in the BNP levels in the postoperative period.
It was stated that the preoperative BNP plasma level is an indicator for the postoperative left ventricular systolic function in patients who will undergo coronary artery by-pass, in other words, that the high preoperative BNP values are indicators of high risk for patients to undergo coronary by-pass [3,12-15]. In our study, it was found that in patients to undergo coronary artery bypass, the preoperative BNP values will indicate postoperative morbidity at 73% sensitivity and 69% specificity with a cutoff value of 180 mg/dl and furthermore, that each increase of 100pg/dl in BNP raise morbidity by 62.1%.
It was posited that high preoperative BNP values may be an indication of the pervasiveness of the disease and whether there was a significant relationship between the preoperative BNP level and the cross clamp and perfusion times was investigated by Saribülbül et al. [15]; Avidan et al. [16]; Georges et al. [9], Morimoto et al. [17] who found data giving support to this hypothesis. It was hypothesized that both the preoparative high BNP level and also extended cross clamp times are related to the pervasiveness of the coronary arterial disease. Yet, in our study, no relationship could be established between the cross clamp and cardiopulmonary bypass durations and the preoperative BNP level in coronary bypass operations.

A negative and significant relationship was found between the number of anastomosis and all three NT-proBNP levels other than the preoperative NTproBNP. Song et al. [14], in their study on patients on whom they performed open heartsurgery, have published that in case of coronary by-pass, BNP levels were significant indicators for pleural effusion. Although the relationship between BNP and pleural effusion has not yet been figured out entirely, progression of pleural effusion as a complication of myocard failure may be considered (Figure 1). In our study, since there was no pleural effusion requiring thoracentesis, this finding could not be evaluated. Development of postoperative atrial fibrillation in patients undergoing heart surgery and therefore, coronary artery by-pass increases the time of stay in hospital and the risk of onset of morbidity. Wazni OM et al. [18] have published that high preoperative values in heart surgery patients constitute an independent risk factor for onset of postoperative atrial fibrillation.
The incidents of atrial fibrillation in coronary artery by-pass surgery are 16-33% with the etiology not yet fully resolved. Song et al. [14], in their study, have found the BNP peak to be over 450 pgr/mL in all patients in whom atrial fibrillation developed. In the study by Albage et al. [19], statistically significant decrease was determined in BNP levels in patients they administered the isolated Maze procedure. The drop in BNP levels is an indicator of the development of ventricular function post Maze operation. At the same time, high BNP levels are also indicators of thromboembolic incidents as atrial fibrillation increases such thromboembolic incidents. However, no post-operative atrial fibrillation was observed in our series of 22 subjects.
Conclusion
We believe based on our clinical study that preoperative BNP levels is a useful parameter in determining the morbidity and prognosis in the early postoperative period of patients with no left ventricular dysfunction to undergo cardiopulmonary bypass or coronary artery bypass graft surgery. However, we are also aware that a much greater number of findings and clinical studies are needed.
References
- Henry JP, Gauer Oh, Reeves JL (1956) Evidence of the atrial location of receptors influencing urine flow. Circ Res 4(1): 85-90.
- KISCH B (1956) Electron microscopy of the capillary wall. Exp Med Surg 14: 113-121.
- Wei CM, Heublein DM, Perrella MA, Lerman A, Rodeheffer RJ, et al. (1993) Natriuretic peptide system in heart failure. Circulation 88(3): 1004-1009.
- Sudoh T, Kangawa K, Minamino N, Matsuo H (1988) A new natriuretic peptide in porcine brain. Nature 332(6159): 78-81.
- Suga S, Nakao K, Hosoda K, Mukoyama M, Ogawa Y, et al. (1992) Receptor selectivity of natriuretic peptide family, atrial natriuretic peptide, brain natriuretic peptide, and C-type natriuretic peptide. Endocrinology 130(1): 229-239.
- Qi W, Mathisen P, Kjekshus J, Simonsen S, Bjørnerheim R, et al. (2001) Natriuretic peptides in patients with aortic stenosis. Am Heart J 142(4): 725-732.
- Gerber IL, Stewart RA, Legget ME, West TM, French RL, et al. (2003) Increased plasma natriuretic peptides reflect symptom onset in aortic stenosis. Circulation 107(14): 1884-1890.
- Bergler-Klein J, Klaar U, Heger M, Rosenhek R, Mundigler G, et al. (2002) Prognastic value of natriuretic peptides in asymptomatic and symptomatic severe aortic stenosis. Circulation (2): 640-647.
- Georges A, Forestier F, Valli N, Plogin A, Janvier G, et al. (2004) Changes in type B natriuretic peptide (BNP) concentrations during cardiac valve replacement. Eur J Cardiotharc Surg 25(6): 941-945.
- Munagala VK, Burnett JC Jr, Redfield MM (2004) The natriuretic peptides in cardiovascular medicine. Curr Probl Cardiol.; 29(12): 707- 769.
- M. Chello, P. Mastroroberto, F. Perticone, F. Cirillo, E. Bevacqua, et al. (2001) Plasma levels of atrial and brain natriuretic peptides as indicators of recovery of left ventriculer systolic function after coranary artery bypass. European Journal of Cardio-thoracic Surgery 20: 140-146.
- Akihiro Matsumoto, Yasunobu Hirata, Shin-ichi Momomura, Etsu Suzuki, Ikuo Yokoyama, et al. (1995) Effects of exercise on plasma level of brain natriuretic peptide in congestive heart failure with and without left ventricular dysfunction. Am Heart J 129(1): 139-145.
- Yasue H, Yoshimura M, Sumida H, Kikuta K, Kugiyama K, et al. (1994) Localization and mechanism of secretion of B-type natriuretic peptide in comparison with those of A-type natriuretic peptide in normal subjects and patients with heart failure. Circulation 90(1): 195-203.
- Song M, Kobayashie Y, Michi H (2004) Clinical implication of atrial and brain natriuretic peptide in coranary artery bypass grafting. Asian Cardiovasc Thorac Ann 12(1): 41-46.
- Saribulbul O, Alat I, Coskun S, Apaydin AZ, Yagdi T, et al. (2003) The role of brain natriuretic peptide in the prediction of cardiac performance in coronary artery bypass grafting. Tex Heart Inst J 30(4): 298-304.
- Avidan MS, Meehan M, Ponte J, El-Gamel A, Sherwood RA (2001) Change in brain natriuretic peptide concentrations following open cardiac surgery with cardioplegic cardiac arrest. Clin Chim Acta 303(1- 2): 127-132.
- Morimoto K, Mori T, Ishiguro S, Matsuda N, Hara Y, et al. (1998) Perioperative changes in plasma brain natriuretic peptide concentrations in patients undergoing cardiac surgery. Surg Today 28(1): 23-29.
- Wazni OM, Martin DO, Marrouche NF, Latif AA, Ziada K, et al. (2004) Plasma B-type natriuretic peptide levels predict postoperative atrial fibrilation in patients undergoing cardiac surgery. Circulation 110(2): 124-127.
- Albåge A, Kennebäck G, van der Linden J, Berglund H (2003) Improved neurohormonal markers of ventriculer function after restoring sinus rythm by the maze procedure. Ann Thorac Surg 75(3): 790-795.






























