Research Article
Hybrid and Robotic-Assisted Coronary Artery Revascularization Compared to Conventional Coronary Artery Bypass Graft Revascularization
R Todd Drexel1*, Kenneth Liao2, Samit Roy1 and Gladwin S Das1
1Department of Cardiovascular Medicine, University of Minnesota, USA
2Department of Cardiothoracic Surgery, University of Minnesota, USA
Submission: April 18, 2016; Published: April 25, 2016
*Corresponding author: R. Todd Drexel, University of Minnesota, Department of Cardiovascular Medicine, Minnesota, Minneapolis-55455, Canada, Tel: 612-626-2451; Email: drexe001@umn.edu
How to cite this article: R Todd D, Kenneth L, Samit R, Gladwin S D. Hybrid and Robotic-Assisted Coronary Artery Revascularization Compared to Conventional Coronary Artery Bypass Graft Revascularization. J Cardiol & Cardiovasc Ther. 2015; 1(2): 555559. DOI: 10.19080/JOCCT.2016.01.555559
Abstract
Objectives: Data were evaluated to compare hybrid and robotic revascularization procedures with conventional coronary artery bypass grafting for the treatment of multi vessel coronary artery disease.
Background: Hybrid coronary revascularization provides an alternative approach to conventional coronary artery bypass graft and percutaneous intervention revascularization therapies. Data comparing the two strategies are limited.
Methods: A retrospective evaluation was conducted on patients who underwent coronary revascularization by hybrid, robotic alone or conventional coronary artery bypass grafting from 2003 through 2014 at the University of Minnesota medical center by a single operator
Results: A total of 399 patients were included in the comparison with 31 hybrid, 68 robotic-only and 300 conventional coronary bypass patients. Mean OR times and hospital stay durations were decreased for hybrid and robotic-only procedures in comparison to conventional bypass procedures. Peri-operative blood product requirements were also decreased in the hybrid group and robotic-only groups. Post-operative stroke events occurred in 3 patients (1%) in the conventional bypass group, but did not occur in the hybrid or robotic-only groups. Similarly, post-operative death occurred in 5 patients (1.7%) in the conventional bypass group, but did not occur in the hybrid or robotic-only groups.
Conclusion: Hybrid and robotic-assisted coronary revascularization are both effective therapies for multi vessel coronary artery disease. The hybrid and robotic-assisted strategies allow for minimal invasion, which translates into shorter operative and hospital length of stay durations, decreased blood product requirements and seemingly fewer stroke and death events.
Keywords: Minimally invasive; Off-pump; Percutaneous coronary intervention
Abbreviations: HCR: Hybrid Coronary Revascularization; LAD: Left Anterior Descending Artery, LIMA: Left Internal Mammary Artery; PCI: Percutaneous Coronary Intervention; LCx: Left Circumflex; RCA: Right Coronary Arteries; CABG: Coronary Artery Bypass Grafting; CAD: Coronary Artery Disease; STS: Society of Thoracic Surgeons
Introduction
Hybrid coronary revascularization (HCR) is a technique used to minimize patient invasion while obtaining excellent restoration of blood flow to the myocardium. The procedure involves a robotic take-down of the left internal mammary artery (LIMA) for revascularization of the left anterior descending artery (LAD) by a small lateral thoracotomy and percutaneous coronary intervention (PCI) for significant lesions in the left circumflex (LCx) and right coronary (RCA) arteries. Robotic coronary artery bypass grafting (CABG) is a technique that has traditionally only been an option for high-risk patients with comorbidities that prohibited a conventional median sternotomy approach. The improvement in off-pump techniques and reduction in peri-procedural complications compared to on-pump procedures has broadened the use of robotic and minimally invasive procedures to now include patients with all risk profiles [1].
Previous studies have examined the utilization of hybrid procedures for coronary artery revascularization and have shown this approach to be a feasible option [2]. Hybrid revascularization patients have similar or fewer post-operative complications when compared to conventional CABG patients [3,4] as well as shorter durations of intubation, intensive care unit and hospital stays [3,5-7]. Patients undergoing HCR have similar 30-day MACE rates of around 1% and three year survival of approximately 94% [8]. This study was performed to compare hybrid, robotic-assisted alone (i.e., without PCI as in hybrid procedures) and conventional CABG at a single center to further evaluate the use of hybrid and robotic-assisted procedures in revascularization and to provide additional data to help expand the number of observations in this growing field.
Methods
Data from patients undergoing surgical revascularization by a single operator from September 2, 2003 through December 18, 2014 at the University of Minnesota medical center were collected from the electronic medical record. Revascularization procedures were categorized as hybrid procedures if a minimally invasive LIMA to LAD bypass was performed and additional coronary artery stenoses were treated with PCI either during the same hospitalization or within a reasonably soon time period. In addition to hybrid and conventional CABG revascularization procedures, data regarding robotic-only revascularization procedures (not associated with additional PCI or vein grafts) were also collected. The hybrid population was designated as Group A, the robotic-only population was designated as Group B and the conventional CABG population was designated as Group C.
Indications for HCR included favorable LIMA and LAD anatomic locations for a robotic approach as well as additional coronary artery disease (CAD) lesions deemed treatable by PCI. Patients were selected for a HCR approach based on comorbidities, prior surgical complications, and projected poor wound healing and patient preference. The decision to proceed with HCR was made after careful consideration of other options including conventional CABG by the surgeon, interventional cardiologist, referring physician and patient. Contraindications to HCR included diffuse CAD that was not amenable to PCI and inability to undergo a robotic harvest of the LIMA. Factors limiting robotic harvesting of the LIMA included body habitus, unstable CAD and severe pulmonary disease that would be unlikely to tolerate single-lung ventilation.
The minimally invasive bypass method involved a robotic LIMA harvest followed by a small anterior or lateral thoracotomy. The da Vinci Surgical System (Intuitive Surgical Incorporation, Sunnyvale, California) was used for LIMA harvest, to access the pericardium and to identify the optimal LAD graft site. A small anterior thoracotomy incision of 5 cm is then made for grafting of the LIMA to the LAD. Exposure of the LAD graft site is obtained with a soft tissue retractor and the LIMA to LAD anastomosis is completed with an 8-0 polypropylene suture. The procedures were performed without need for rib spreading or cardiopulmonary bypass. The PCI portion was generally performed after the robotic bypass to limit bleeding risk given the requirement of dual anti-platelet therapy following PCI. Timing of robotic and PCI procedures were determined by acuity, disease severity, patient comorbidities (e.g., staged PCI to limit risk of contrast induced nephropathy) and availabilities of the patient and procedural teams. Drug eluting stents were implanted unless a contraindication for longer term dual antiplatelet therapy existed.
Peri-operative hospital requirements and complications were the outcomes evaluated for this study. Hospital requirements included OR time, intubation time, ICU time and hospital duration. Complications included post-operative cerebrovascular accidents, atrial fibrillation, bleeding requiring a blood transfusion, death and readmission within 30 days. The robotic revascularization group was separated into HCR and robotic-only revascularization groups. The robotic-only group refers to patients that only underwent revascularization with a LIMA to LAD graft by robotic LIMA harvest and did not have vein grafts or PCI. Statistical analyses were conducted using SAS 9.3 (SAS Institute Inc. Cary, NC, USA.). Differences in the distribution of baseline characteristics and outcomes between groups were assessed using chi-square tests for categorical variables and t-tests for continuous variables. Given the exploratory nature of this analysis, if the expected cell count for any chi-squared test was below 5, Fisher’s exact test was used in lieu of a chi-squared test.
The study included a total of 399 patients with 31 hybrids, 68 robotic-only and 300 conventional CABG revascularization strategies. Baseline characteristics were generally similar between groups and are displayed in (Table 1). The PCI portion was completed after the robotic CABG portion in all but three cases, occurred during the robotic CABG hospitalization in 18 patients and was performed an average of within 38 days of the robotic procedure. The mean age, gender distribution (male 68% to 73%) mean BMI values were similar across groups. Risk factors of diabetes, hyperlipidemia, hypertension, family history and tobacco use were similar. Pre-operative medication regimens were similar for aspirin, beta blocker, angiotensin converting enzyme inhibitor/angiotensin receptor blocker and lipid-lowering therapy. A greater proportion of patients with prior coronary bypass revascularization were identified in the conventional bypass group. The hybrid patient group was composed of patients with single-vessel disease (3%), twovessel disease (45%) and three-vessel disease (52%); whereas, the conventional bypass group had patients with single-vessel disease (4%), two-vessel disease (18%) and three-vessel disease (78%). Average surgical mortality risks, based on Society of Thoracic Surgeons (STS) Adult Cardiac Surgery Risk Calculator estimates, were similar across groups with 2.2% to 2.8% risk estimates.
Table 1: Baseline Patient Characteristics for Hybrid, Robotic-Only, Hybrid/Robotic Combined and Conventional Coronary Revascularization. Note that “n” refers to the number of patients. P-values marked with (†) indicate rank-sum test was used for data comparison. P-values marked with (‡) indicate that Fisher’s exact test was used for data comparison. Values listed following a “±” are standard deviation values. Single values listed in parentheses represent the percentage of patients within each category.
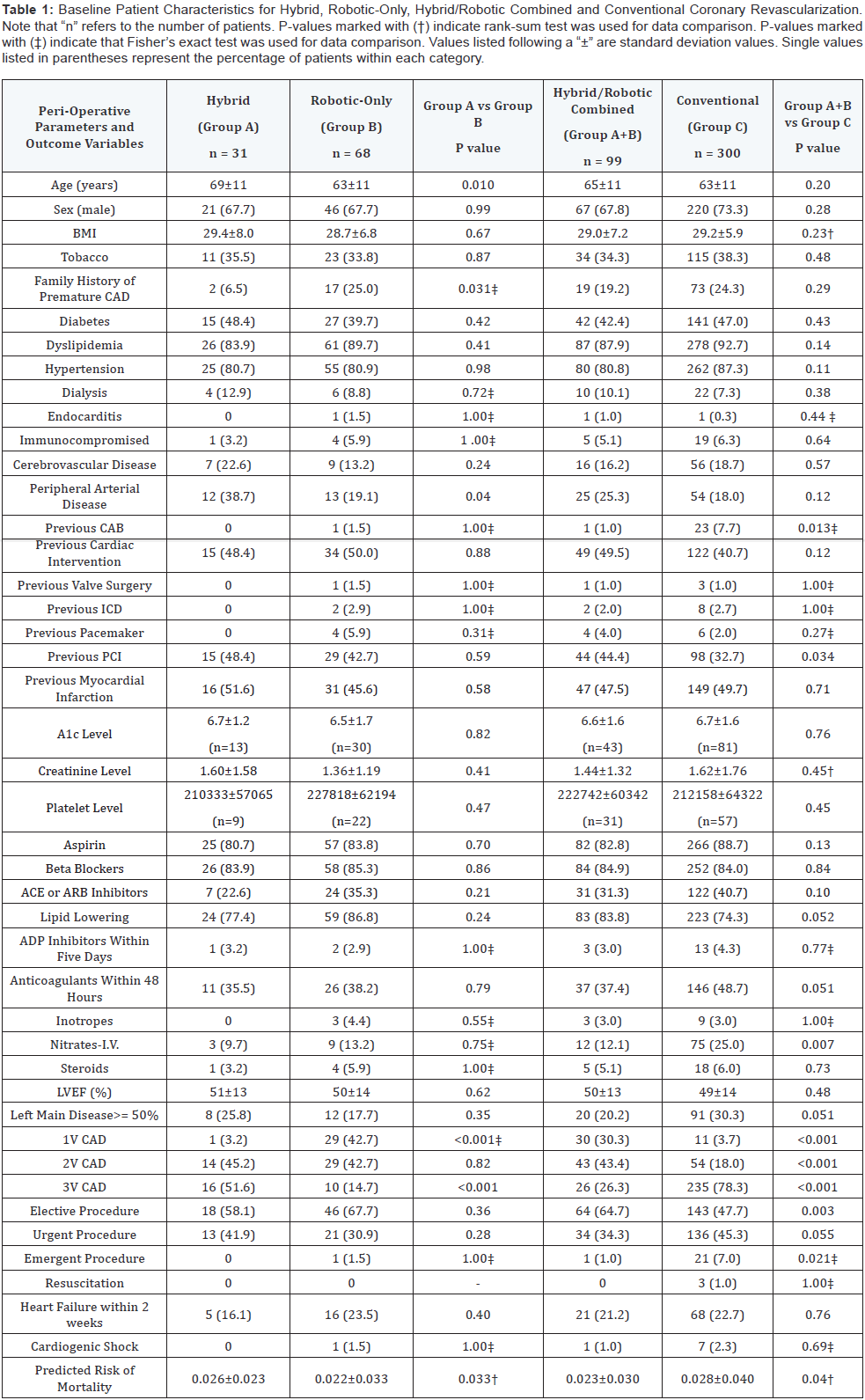
Table 2: Outcomes Data for Hybrid, Robotic-Only, Hybrid/Robotic Combined and Conventional Coronary Revascularization. Note that “n” refers to the number of patients. P-values marked with (†) indicate rank-sum test was used for data comparison. P-values marked with (‡) indicate that Fisher’s exact test was used for data comparison. Values listed following a “±” are standard deviation values. Single values listed in parentheses represent the percentage of patients within each category.
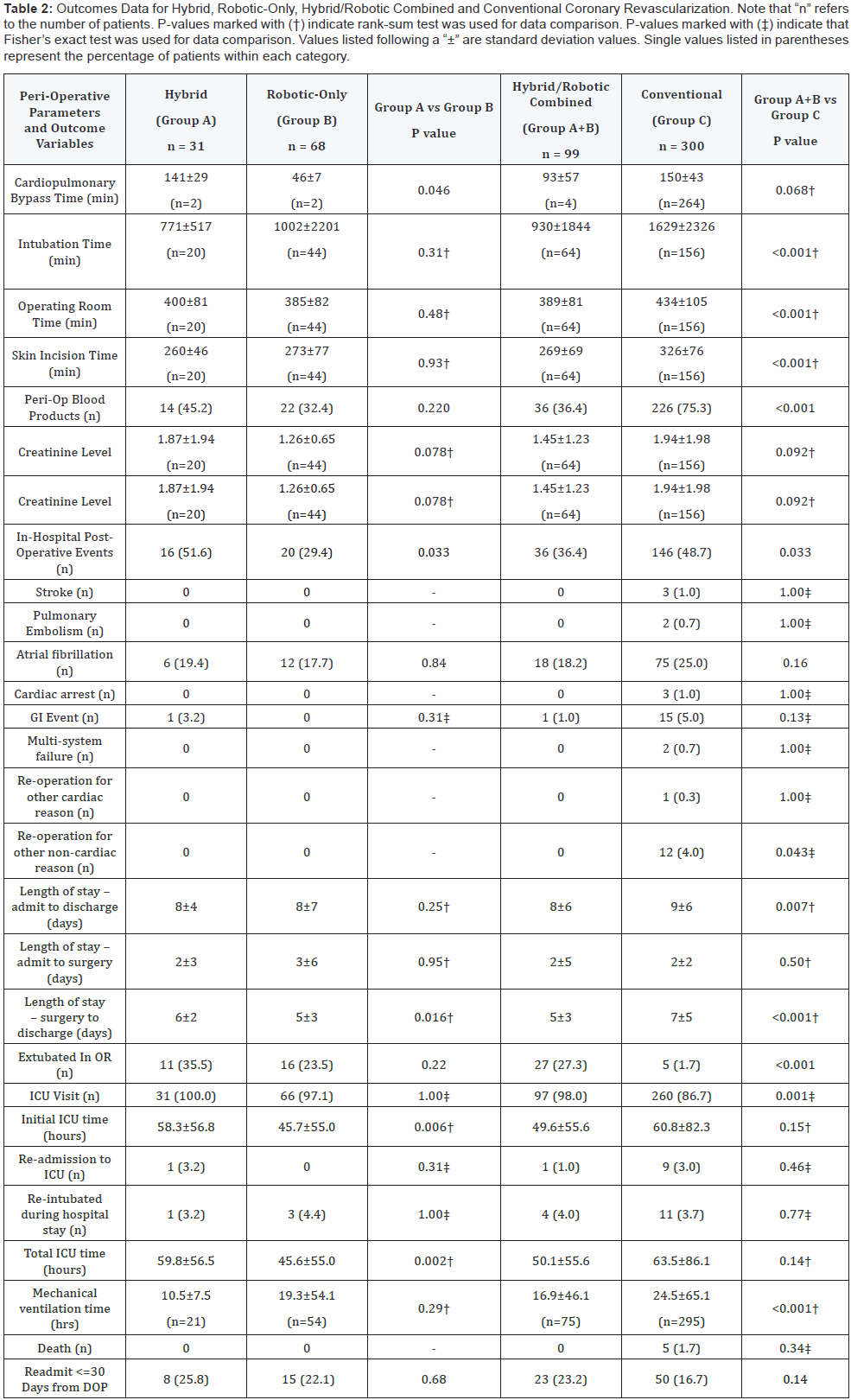
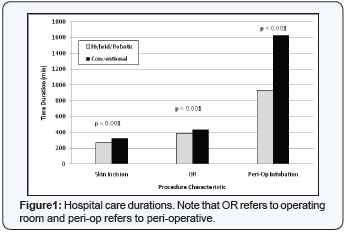
Outcomes of hospital care durations are listed in (Table 2) and displayed in (Figure 1). Mean OR times for hybrid, roboticonly and conventional bypass groups were 400 min, 385 min and 434 min, respectively. Mean ICU stays were 60 hours for hybrid, 46 hours for robotic-only and 64 hours for conventional bypass patients. Mean peri-operative intubation times were 12.9 hrs (771 min) in hybrid, 16.7 hrs (1,002 min) in robotic-only and 27.2 hrs (1,629 min) in conventional bypass patients. Mean lengths of hospital stays were 8 days in hybrid, 8 days in roboticonly and 9 days in conventional bypass patients.
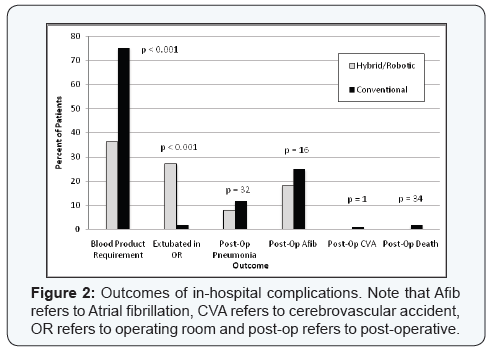
Outcomes of in-hospital complications are listed in (Table 2) and displayed in (Figure 2). Peri-operative blood product requirements were increased in the conventional bypass group with approximately 75% of patients in the conventional bypass group requiring a blood transfusion compared to 45% of hybrid and 32% of robotic-only groups. Peri-operative atrial fibrillation occurred in 19% of hybrid, 18% of robotic-only and 25% of conventional bypass patients. Post-operative stroke events occurred in 1.0% of the conventional bypass group, but did not occur in the hybrid or robotic-only groups. Similarly, postoperative death occurred in 1.7% of the conventional bypass group, but did not occur in the hybrid or robotic-only groups. Re-admission rates within 30 days from the date of surgery were 26% in the hybrid group, 22% in the robotic-only group and 17% in the conventional bypass group.
Discussion
The results of this study confirm that hybrid and roboticonly procedures provide an excellent option for coronary revascularization. The data reflect outcomes of a single operator so there are no possibilities for inter-operator variability. Hybrid and robotic revascularization procedures are associated with shorter durations of OR time, ventilator management, ICU care and overall hospital length of stay as well as fewer requirements for blood transfusions. Previous studies have also identified substantially shorter durations of OR time, ventilator management, ICU care and overall hospital length of stay for hybrid procedures in comparison to conventional CABG procedures [6,7,9]. Although most patients undergo LIMA to LAD revascularization prior to PCI, as was the case in this study, the sequence of revascularization has been shown to have no impact on outcomes [10]. However, performing the PCI before or at the same time of robotically assisted revascularization did relate to shorter durations of ICU and hospital lengths of stay compared to a surgery-first approach [10].
The hybrid and robotic-only groups were found to have lower rates of peri-operative blood transfusions as well as fewer stroke and death events, but myocardial infarction events occurred more frequently in the hybrid group. Although there were no CVA or death events in the hybrid and robotic-only groups, the lack of events possibly reflects the relatively smaller number of patients available for evaluation, but may also be related to the avoidance of both aortic cross clamping as well as the heart-lung machine. There was a trend toward greater prevalence of PAD in the hybrid and robotic-only groups, but, even though PAD is a predictor of poor operative outcomes, the hybrid and roboticonly groups had no CVA or death and generally had better outcomes. The improved outcomes identified in the hybrid and robotic-only combined group may relate to the decreased use of intravenous nitroglycerin during the surgical procedure as this may result in decreased blood pressure variability.
Prior studies have found no difference in rates of in-hospital CVA or death between hybrid and conventional CABG groups with both CVA and death rates less than 1%; however, there is a trend of fewer events in the hybrid group [3,7-9,11]. Overall in-hospital MACE rates have been similar between hybrid and conventional CABG groups [7-9] with the exception of one study that found higher MACE rates in the conventional CABG group [3]. This study identified higher rates of peri-operative myocardial infarction in the hybrid group in comparison to both the roboticonly and conventional bypass groups. Peri-operative myocardial infarction with resultant Q wave development complicates up to 10% of conventional bypass operations [12,13]. Peri-procedural myocardial infarction as defined by a biomarker increase greater than three times the upper limit of normal complicates approximately 22% of PCI procedures [14].
Patients with complex CAD and low to intermediate surgical risk assessments based on SYNTAX (score < 33) and Euro Score (score < 6) have been shown to have similar 30 day rates of MACE, changes in renal function and bleeding events between hybrid and conventional CABG groups [15]. Longer-term monitoring has shown similar results at 3 years with similar MACE rates in low, intermediate and high-risk groups, based on SYNTAX and Euro Score estimates [16]. Revascularization is one endpoint that has been identified in some, but not all studies, to occur more frequently in the hybrid and robotic-only revascularization groups [6-9]. Although our data do not specifically evaluate outcomes of HCR in high risk patients, individuals in this group are seemingly good candidates for HCR as the LIMA bypass is utilized, but the stress of sternotomy, aortic cross-clamping and bypass pump administration is avoided.
The HCR strategy provides mortality benefits from both a LIMA to LAD bypass as well as achieving complete revascularization of non-LAD arteries with drug-eluting stents. The survival benefit associated with a LIMA to LAD bypass in comparison to vein grafts and stenting has been demonstrated [17-20]. Complete revascularization has also been shown to have a mortality benefit compared to incomplete revascularization over a period of monitoring up to 10 years [21- 25]. Under reasonable circumstances of anatomy and viability, complete revascularization provides benefits over incomplete revascularization and should be the goal when applicable.
Maintenance of revascularization patency has been an issue with both vein graft and stent therapies. Vein graft failure (>70% of grafts occluded) occurs in about 10-45% of conventional CABG patients at one year and around 50% of vein grafts are occluded at 10 years [26-28]. In contrast, in-stent restenosis requiring revascularization occurs in approximately 25% of bare-metal and 5-10% of drug-eluting stents at 5 years [29- 31]. The combined benefits of mortality reduction with LIMA to LAD bypass grafting and non-LAD revascularization patency of stenting make a HCR a favorable approach.
Conventional CABG procedures are traditionally performed on an arrested heart with use of a temporary bypass pump for circulatory support (on-pump). Minimally invasive CABG procedures, including robotic-assisted CABG, are often performed on a beating heart without need for additional circulatory support (off-pump). The LIMA graft patency at one year was found to be significantly less in the off-pump group with patency rates of 88.7% in off-pump and 93.4% in on-pump groups [32]. Although the LIMA patency rate was found to be decreased with off-pump procedures, a separate meta-analysis found lower rates of post-operative stroke and no change in mortality or myocardial infarction at 30 days [33].
Lastly, minimally invasive procedures utilized for harvesting the LIMA and for anastomosis of the LIMA to the LAD are not universally practiced and their success, like all procedures, depends on the proficiency of the operator. Rates of conversion from a robotically-assisted procedure to an open-chest procedure were studied and found to substantially decrease as robotic experience increased from a conversion rate of 28% in the first 25 patients to 4% after completion of 75 patients [34]. Significant decreases in operative time and hospital length of stay durations also correlated with increasing experience [34]. Although successful completion of the intended robotic procedure and overall efficiency improved with experience, patient safety was not compromised during the learning period as mortality remained unchanged. Limitations of the study included the small number of hybrid patients and the lack of detailed follow up beyond the initial hospitalization. This was a retrospective cohort analysis that lacks the obvious benefits of prospective randomized trial. Patients were selected to undergo HCR based on comorbidities, prior surgical complications; projected poor wound healing and patient preference so a selection bias is possible.
Conclusion
Hybrid coronary revascularization procedures provide complete revascularization with utilization of optimal LIMA to LAD bypass grafting with percutaneous intervention of the LCx and RCA vessels. Robotic bypass grafting allows for minimal invasion and requires shorter durations of ventilation management, ICU stay and length of hospitalization as well as fewer peri-operative blood transfusion requirements. Emergent robotic bypass grafting is possible, but more commonly completed by conventional bypass grafting. The finding that operating room time and surgery time (i.e., skin incision time) were both shorter in the hybrid/robotic group is notable as these data are for a single skilled surgeon. Increased successful extubation within the operating room and decreased blood product requirements in the hybrid/robotic group are also important findings. Although the numbers of stroke and death events were too small for statistical analyses, there were no stroke or death events in the hybrid and robotic bypass groups. Patients with multi vessel CAD should be considered for revascularization with a HCR procedure. We suggest that patients with non-emergent coronary heart disease who have less than severe lung disease and pulmonary hypertension with LIMA anatomy that is favorable for harvest by a lateral incision are ideal candidates for HCR and will benefit from this revascularization method.
Author Contributions
Dr. Drexel wrote the manuscript with help from Drs. Das and Liao and Samit Roy and all were involved with some aspect of procedural completion, data collection and analysis. All authors have reviewed and approved of this paper.
Conflict of Interest
Dr. Drexel: none. Samit Roy: none. Dr. Das: none. Dr. Liao: none.
References
- Hannan EL, Wu C, Smith CR, Higgins RS, Carlson RE, et al. (2007) Off-Pump Versus On-Pump Coronary Artery Bypass Graft Surgery Differences in Short-Term Outcomes and in Long-Term Mortality and Need for Subsequent Revascularization. Circulation 116(10): 1145- 1152.
- Kevin Phan, Sophia Wong, Nelson Wang, Steven Phan, Tristan D Yan (2015) Hybrid coronary revascularization versus coronary artery bypass surgery: systematic review and meta-analysis. International Journal of Cardiology 179: 484-488.
- Kon ZN, Brown EN, Tran R, Joshi A, Reicher B, et al. (2008) Simultaneous hybrid coronary revascularization reduces postoperative morbidity compared with results from conventional off-pump coronary artery bypass. J Thorac Cardiovasc Surg 135(2): 367-375.
- Zhao DX, Leacche M, Balaguer JM, Boudoulas KD, Damp JA, et al. (2009) Routine intraoperative completion angiography after coronary artery bypass grafting and 1-stop HCR results from a fully integrated hybrid catheterization laboratory/operating room. J Am Coll Cardiol 53(3): 232-241.
- de Cannière D, Jansens JL, Goldschmidt-Clermont P, Barvais L, Decroly P, et al. (2001) Combination of minimally invasive coronary bypass and percutaneous transluminal coronary angioplasty in the treatment of double-vessel coronary disease: Two-year follow-up of a new hybrid procedure compared with ‘on-pump’ double bypass grafting. Am Heart J 142(4): 563-570.
- Reicher B, Poston RS, Mehra MR, Joshi A, Odonkor P, et al. (2008) Simultaneous ‘hybrid’ percutaneous coronary intervention and minimally invasive surgical bypass grafting: feasibility, safety, and clinical outcomes. Am Heart J 155(4): 661-667.
- Hu S, Li Q, Gao P, Xiong H, Zheng Z, et al. (2011) Simultaneous hybrid revascularization versus off-pump coronary artery bypass for multivessel coronary artery disease. Ann Thorac Surg 91(2): 432-438.
- Vassiliades TA, Kilgo PD, Douglas JS, Babaliaros VC, Block PC, et al. (2009) Clinical outcomes after hybrid coronary revascularization versus off-pump coronary artery bypass: a prospective evaluation. Innovations (Phila) 4(6): 299-306.
- Halkos ME, Vassiliades TA, Douglas JS, Morris DC, Rab ST, et al. (2011) Hybrid coronary revascularization versus off-pump coronary artery bypass grafting for the treatment of multivesselcoronary artery disease. Ann Thorac Surg 92(5): 695-1701.
- Srivastava MC, Vesely MR, Lee JD, Lehr EJ, Wehman B, et al. (2013) Robotically assisted hybrid coronary revascularization: does sequence of intervention matter? Innovations (Phila) 8(3): 177-183.
- Delhaye C, Sudre A, Lemesle G, Vanesson L, Koussa M, et al. (2010) Hybrid revascularization, comprising coronary artery bypass graft with exclusive arterial conduits followed by early drug-eluting stent implantation, in multivessel coronary artery disease. Arch Cardiovasc Dis 103(10): 502-511.
- Yau JM, Alexander JH, Hafley G, Mahaffey KW, Mack MJ, et al. (2008) Impact of perioperative myocardial infarction on angiographic and clinical outcomes following coronary artery bypass grafting (from PRoject of Ex-vivo Vein graft ENgineering via Transfection [PREVENT] IV). Am J Cardiol 102(5): 546-551.
- Mohammed AA, Agnihotri AK, van Kimmenade RR, Martinez-Rumayor A, Green SM, et al. (2009) Prospective, comprehensive assessment of cardiac troponin T testing after coronary artery bypass graft surgery. Circulation 120(10): 843-850.
- Tricoci P, Leonardi S, White J, White HD, Armstrong PW, et al. (2013) Cardiac troponin after percutaneous coronary intervention and 1-year mortality in non-ST-segment elevation acute coronary syndrome using systematic evaluation of biomarker trends. J Am Coll Cardiol 62(3): 242-251.
- M Leacche M, Byrne JG, Solenkova NS, Reagan B, Mohamed TI, et al. (2013) Comparison of 30-day outcomes of coronary artery bypass grafting surgery verus hybrid coronary revascularization stratified by SYNTAX and euroSCORE. J Thorac Cardiovasc Surg 145(4): 1004-1012.
- Shen L, Hu S, Wang H, Xiong H, Zheng Z, et al. (2013) One-stop hybrid coronary revascularization versus coronary artery bypass grafting and percutaneous coronary intervention for the treatment of multivessel coronary artery disease: 3-year follow-up results from a single institution. J Am Coll Cardiol 61(25): 2525-2533.
- Loop FD, Lytle BW, Cosgrove DM, Stewart RW, Goormastic M, et al. (1986) Influence of the internal-mammary-artery graft on 10-year survival and other cardiac events. N Engl J Med 314(1): 1-6.
- DHannan EL, Wu C, Walford G, Culliford AT, Gold JP, et al. (2008) Drugeluting stents vs. coronary-artery bypass grafting in multivessel coronary disease. N Engl J Med 358(4): 331-341.
- Wu C, Zhao S, Wechsler AS, Lahey S, Walford G, et al. (2011) Long-term mortality of coronary artery bypass grafting and bare-metal stenting. Ann Thorac Surg 92(6): 2132-2138.
- Wu C, Camacho FT, Zhao S, Wechsler AS, Culliford AT, et al. (2013) Long-term mortality of coronary artery bypass graft surgery and stenting with drug-eluting stents. Ann Thorac Surg 95(4): 1297-1305.
- Sarno G, Garg S, Onuma Y, Gutiérrez-Chico JL, van den Brand MJ, et al. (2010) Impact of completeness of revascularization on the five-year outcome in percutaneous coronary intervention and coronary artery bypass graft patients (from the ARTS-II study). Am J Cardiol 106(10): 1369-1375.
- Aggarwal V, Rajpathak S, Singh M, Romick B, Srinivas VS (2012) Clinical outcomes based on completeness of revascularisation in patients undergoing percutaneous coronary intervention: a meta-analysis of multivessel coronary artery disease studies. EuroIntervention 7(9): 1095-1102
- Vieira RD, Hueb W, Gersh BJ, Lima EG, Pereira AC, et al. (2012) Effect of complete revascularization on 10-year survival of patients with stable multivessel coronary artery disease: MASS II trial. Circulation 126(11 Suppl 1): S158-S163.
- Garcia S, Sandoval Y, Roukoz H, Adabag S, Canoniero M, et al. (2013) Outcomes after complete versus incomplete revascularization of patients with multivessel coronary artery disease: a meta-analysis of 89,883 patients enrolled in randomized clinical trials and observational studies. J Am Coll Cardiol 62(16): 1421-1431.
- Lichtenberg A, Klima U, Paeschke H, Pichlmaier M, Ringes-Lichtenberg S, et al. (2004) Impact of multivessel coronary artery disease on outcome after isolated minimally invasive bypass grafting of the left anterior descending artery. Ann Thorac Surg 78(2): 487-491.
- Alexander JH, Hafley G, Harrington RA, Peterson ED, Ferguson TB, et al. (2005) Efficacy and safety of edifoligide, an E2F transcription factor decoy, for prevention of vein graft failure following coronary artery bypass graft surgery: PREVENT IV: a randomized controlled trial. JAMA 294(19): 2446-2454.
- Magee MJ, Alexander JH, Hafley G, Ferguson TB Jr, Gibson CM, et al. (2008) Coronary artery bypass graft failure after on-pump and offpump coronary artery bypass: findings from PREVENT IV. Ann Thorac Surg 85(2): 494-499.
- Harskamp RE, Lopes RD, Baisden CE, de Winter RJ, Alexander JH (2013) Saphenous vein graft failure after coronary artery bypass surgery: pathophysiology, management, and future directions. Ann Surg 257(5): 824-833.
- Ellis SG, Stone GW, Cox DA, Hermiller J, O’Shaughnessy C, et al. (2009) Long-term safety and efficacy with paclitaxel-eluting stents: 5-year final results of the TAXUS IV clinical trial (TAXUS IV-SR: Treatment of De Novo Coronary Disease Using a Single Paclitaxel-Eluting Stent). JACC Cardiovasc Interv 2(12): 1248-1259.
- Weisz G, Leon MB, Holmes DR Jr, Kereiakes DJ, Popma JJ, et al. (2009) Five-year follow-up after sirolimus-eluting stent implantation results of the SIRIUS (Sirolimus-Eluting Stent in De-Novo Native Coronary Lesions) Trial. J Am Coll Cardiol 53(17): 1488-1497.
- Kandzari DE, Mauri L, Popma JJ, Turco MA, Gurbel PA, et al. (2011) Lateterm clinical outcomes with zotarolimus- and sirolimus-eluting stents. 5-year follow-up of the ENDEAVOR III (A Randomized Controlled Trial of the Medtronic Endeavor Drug [ABT-578] Eluting Coronary Stent System Versus the Cypher Sirolimus-Eluting Coronary Stent System in De Novo Native Coronary Artery Lesions). JACC Cardiovasc Interv 4(5): 543-550.
- Hattler B, Messenger JC, Shroyer AL, Collins JF, Haugen SJ, et al. (2012) Off-Pump coronary artery bypass surgery is associated with worse arterial and saphenous vein graft patency and less effective revascularization: Results from the Veterans Affairs Randomized On/ Off Bypass (ROOBY) trial. Circulation 125(23): 2827-2835.
- Afilalo J, Rasti M, Ohayon SM, Shimony A, Eisenberg MJ (2012) Offpump vs. on-pump coronary artery bypass surgery: an updated metaanalysis and meta-regression of randomized trials. Eur Heart J 33(10): 1257-1267.
- Afilalo J, Rasti M, Ohayon SM, Shimony A, Eisenberg MJ, et al. (2009) Effectiveness and safety of total endoscopic left internal mammary artery bypass graft to the left anterior descending artery. Am J Cardiol 104(12): 1684-1688.






























