Diagnosis and Treatment of an Unusual Atypical Acute Periodontal Abscess
Rocío Valenzuela-Narváez 1, 2* and Luis M Veliz D1
1University of Barcelone, Spain
2Medical Surgical Department, National University of San Marcos, Peru
Submission: December 12, 2019; Published: January 08, 2020
*Corresponding author: Rocío Valenzuela-Narváez, DDS National Council Science Technology and Technological Innovation, University of Barcelone, Spain
How to cite this article: Rocío Valenzuela-Narváez, Luis M Veliz D. Diagnosis and Treatment of an Unusual Atypical Acute Periodontal Abscess. J 0014 Child Adolesc Dent. 2020; 1(1): 555554.
Abstract
The correct diagnosis of pulpal and/or periodontal lesions will allow an adequate and successful treatment. The objective is to report a clinical case of diagnosis and treatment of an atypical acute periodontal abscess to demonstrate that the physiology and pathology of the periodontal and pulpal processes must be better identified, which will allow us to establish a successful treatment. This case report described an atypical acute periodontal abscess located in the region of the upper central incisors pieces 11 and 21, in a 25-year-old male patient, in whom the differential diagnosis and adequate periodontal surgical exploration is reported. The diagnostic procedures for periodontal and pulpal diseases are essential for a correct diagnosis. The physiology and pathology of periodontal and pulpal processes should be better investigated
Keywords: Diagnosis Periodontal disease Acute periodontal abscess Pathogenesis Etiopathology Fistulography Catheterization Temporomandibular Vestibular Subgingival Periapical abscesses
Introduction
The pulpal and periodontal lesions are the most prevalent in the oral cavity. These pathologies are of bacterial etiology, but of a different microbiological type. Currently there are great advances in the knowledge of bacteria but many of them are still not identified. The anatomical and histological structures of the periodontal and pulpal tissues present interrelations in the etiopathology of these processes. The diagnosis of periodontal and pulpal lesions is not always clearly defined. Therefore, it is necessary to perform the differential diagnosis of these two lesions to facilitate the efficient treatment of patients. In this article a case report is presented in which it was complicated to arrive at the correct diagnosis and later treatment. In cases where both periodontal and pulpal lesions are present, the diagnostic process sometimes becomes almost inscrutable and constituting a true test of perception and tenacity to reach the correct diagnosis. The pulp and the periodontium are closely related. It is considered that the signs and symptoms are very useful to establish a definitive differential diagnosis of each of them [1-3], in cases where both periodontal and pulpal lesions are present the diagnostic process sometimes becomes very intricate and almost inscrutable [4].In this regard, Al-Fouzan K, refers in the new classification of endodontic-periodontal lesions that an endoperiodontal lesion may have a varied pathogenesis, considering important the correct diagnosis through a clinical classification to be considered to diagnose and treat with accuracy of endo-periodontal lesion [5].
Case History
A 25-year-old male patient visited a professional due to the presence of pain lasting two weeks. In the region of the upper central incisors, pieces 11 and 21, he stated that the pain was more intense at night. The radiographic examination performed by a specialist is not observed alterations, associating the pain to an old blow, so it is prescribed analgesics. After 2 to 3 days of this episode, the pain is more intense and has a greater swelling that lasts about 4 days. The professional again indicates analgesics and oral antibiotics and mentions as an alternative the endodontic treatment. The pain continues and does not go away, the swelling is much greater and megacillin injectable is prescribed every 12 hours for 5 days. The swelling decreases considerably but a ball persists in the upper incisal region. The patient does not present any alteration of systemic character. At the stomatologic clinical examination it is observed that in the extra oral area there is no alteration or regional pathology.

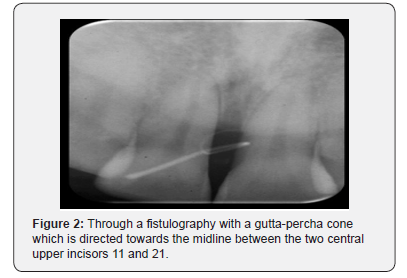
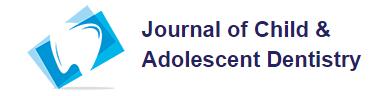
In the intraoral area, a swelling that is fluctuating and depressible is observed in the vestibular face of 11, showing slight pain on manual palpation, this abscess is located at the level of the midline (Figure 1). The pulp vitality tests were performed on the dental pieces 1.1, 12, 13, 21 and 22, so that all respond instantly to cold and heat. To the vertical percussion a normal sound is perceived and no annoyance in the pieces 11, 12, 21 and 22. Ahorizontal percussion does not refer discomfort in the mentioned dental pieces. No alterations of the periodontal tissues or areas of inflammation are observed. At periodontal probing, the clinical parameters of depth of catheterization and level of insertion are within normal ranges. Through a fistulography with a guttapercha cone, which is directed towards the midline (Figure 2) between the two central upper incisors, a slight interproximal bone reabsorption is observed between 11 and 21. Subsequently, several periodontal catheterizations were performed, finding a periodontal pocket of 4.5 mm on the palatal side towards the mesial side and subgingival tartar in the area (Figure 3). A very significant and striking detail is that of not presenting periodontal pocket on the vestibular of piece 11. At the laboratory examination, it was observed that the blood count, clotting time and bleeding time are within normal ranges. As an initial measure he was instructed to continue with the prescribed antibiotic therapy. Three days after the lesion remits and apparently disappears. From the analysis of the information obtained and the corresponding examinations, a problem of occlusion, alteration of the temporomandibular joint, maxillary tumoral pathology and systemic pathology are ruled out. Our opinion, based on the finding of the subgingival is that it is an atypical acute periodontal lesion, despite the fact that there is no deep periodontal pocket, spontaneous bleeding and purulent discharge. For all these considerations, a periodontal surgical exploration will be performed.
Surgical Technique


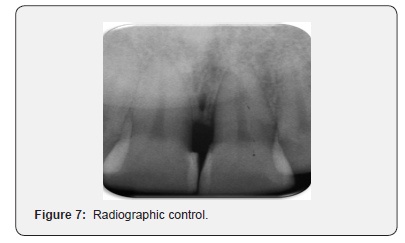
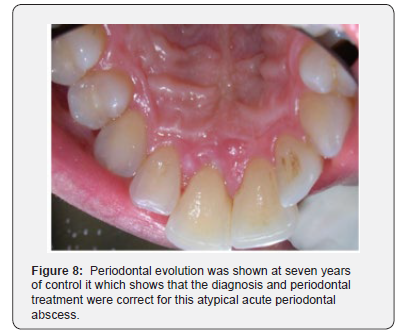
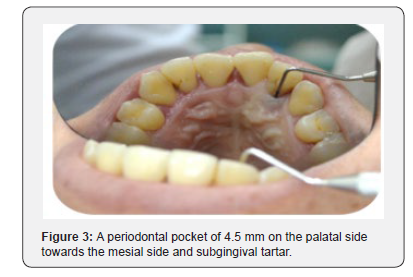
Infiltrative anesthesia was administered in the vestibular and palatal area of the anterior area near the midline. A full thickness periodontal flap was designed to cover parts12, 11, 21 and 22. The interproximal gingival papillae of the before mentioned dental pieces was decollated by the aesthetic implication of the interproximal spaces. When the flap was made on the mesial surface of piece 11, granulation tissue was observed which was removed with the earlier periodontal curettes and scrapers.After removing all the granulation tissue, the flap was carefully repositioned in its place and sutured (Figures 4,5). Adequate periodontal evolution was shown at seven months and seven years of control (Figures 6-8) which shows that the diagnosis and periodontal treatment were correct for this atypical acute periodontal abscess.
Discussion
It is considered that the accessory ducts can be a direct way of communication between the pulp and the periodontium. The presence of accessory ducts varies between 23 and 76%. [2] It is estimated that 30-40% of teeth have lateral or accessory ducts and most of them are located in the apical third of the root. Wildorf found 58.2% apical deltas and 31.3% collateral canals in the lower first premolars [2]. When the pulp becomes necrotic, there is a direct inflammatory response in the periodontal ligament at the level of the apical foramen and/or the exit of accessory conduits. Inflammatory products of pulpal origin can slip through the apex, lateral channels and accessories to trigger an inflammatory vascular response in the periodontium. Among these are living pathogens, such as bacteria, fungi and viruses, many of them similar to the pathogens found in periodontal infections. The action of periodontal inflammation on the pulp it is controversial topic and studies abound with contradictory results. It has been suggested that periodontal disease has no consequence on the pulp, at least until it damages the apex. On the other hand, several studies suggest that the effect of periodontal disease on the pulp is degenerative in nature, with increased calcification, fibrosis and collagen resorption with a direct inflammatory effect. Primary periodontal disease is mainly due to periodontal pathogens in which chronic periodontitis progresses apically along the root surface. In most cases, pulp tests indicate a normal pulpal reaction usually there is plaque buildup and calculus [6]. The treatment of periodontal disease can also cause secondary pulp involvement. The lateral canals and dentinal tubules can be opened in the oral cavity by scaling and root planning or by flap surgery. It is possible for a blood vessel in a lateral conduit to break in the scraping and microorganisms to enter that area during treatment causing inflammation and necrosis of the pulp [7]. On the other hand, clinical test are imperative for the correct diagnosis and for the differentiation between pulp and periodontal disease. A single test is usually not enough to establish a conclusive diagnosis [8,9]. The scientific evidence has been reviewed and a similar case report has not been found. This lesion is atypical because the periodontal abscess of regular size is located on the vestibular of 11, very distant from its origin, which is an incipient periodontal pocket (4.5mm deep) which is located on the mesial palatal surface of the piece 11. Clinically this periodontal abscess located on the middle third of the vestibular root of the piece 11 gives the initial impression of being compatible with an abscess of pulp origin, in a tooth that does not have dental caries and in a patient with a state of health periodontal very acceptable. While the patient ismedicated with antibiotics the periodontal abscesses disappears. After the cessation of the action of antibiotics the abscess returns. The microbiology of periodontal abscesses has been studied by isolating more frequently periodontal pathogens observed in periodontal abscesses more frequently than in periapical abscesses [9]. Remember that periodontal abscess is the third most frequent dental emergency, especially in untreated patients and in periodontal treatment during the maintenance phase [10]. However, in this case the patient is not periodontal or treated or in maintenance. It can be hypothesized that there are still not described anatomical communications that may be joining or being in anastomosis in the mesial area of. The periodontal pocket of 4.5 mm to periodontal probing did not present purulent discharge. We consider that it is important to analyze all clinical aspects necessary to diagnose and adequately treat endoperiodontal lesions, as reported by Western JS & Scully et al. [7,8].
On the other hand, we agree with that reported by Jivoinovici, who recommend that in these lesions endodontic and periodontal treatment should be sequential, with treatment intervals of three months between endodontic treatment and periodontal surgery [9]. As we observed, the endo-perio lesions can be interdependent due to the vascular and anatomical connections, according to Anderson et al. [10] Therefore an accurate identification of the etiological factors of the lesions is essential. It is necessary to differentiate the origins of the periodontal-endodontic lesions, including the communication channels between the pulp and periodontium that act as possible bridges for the dissemination of microorganisms.
Conclusion
The correct diagnosis of pulpal and/or periodontal lesions is fundamental which will allow a successful treatment. Thephysiology and pathology of periodontal and pulpal processes should be better investigated including clinical characteristics. The success requires knowledge and experience for the application of intuitive thinking and the special perceptive sensitivity gives in addition to a rigorous concentration and meticulousness in the task.
References
- Herrera D, Retamal-Valdes B, Alonso B, Feres M (2018) Acute periodontal lesions (periodontal abscesses and necrotizing periodontal diseases) and endo-periodontal lesions. J Periodontol 89: 85-102.
- Wildorf F (2002) Anatomy of the roots and canals of the mandibular first premolars. J Dent Research 71: 63-66.
- Jivoinovici R, Scuciu I, Gheorghiu I, Suciu I (2017) Clinical radiological aspects of primary endodontic lesions with secondary periodontal involvement. J Med Life 10(1): 70-75.
- Kishan KV, Hedge V, Ponnappa KC, Girish TN, Ponappa MC (2014) Management of palate radicular groove in a maxillary lateral incisor. J Nat Sci Biol Med 5(1): 178-181.
- Al-Fouzan KS (2014) A new classification of endodontic-periodontal lesions. Int J Dent 919173: 1-5.
- Wadia R, Ide M (2017) Periodontal emergencies in general practice. Prim Dent J 6(2): 46-51.
- Western JS, Gupta VV, Ramachandra SS (2019) Salvaging a periodontally compromised and endodontically involved three-rooted mandibular first molar with cervical enamel projection. Compen Contin Educ Dent 40: 172-177.
- Scully C, Malamos D (2015) Swelling in the anterior gingivae. Dent Update 42: 981-982.
- Jivoinovici R, Suciu I, Dimitriu B, Perlea P, Bartok R, et al. (2014) Endo-periodontal lesión-endodontic approach. J Med Life 7: 542-544.
- Anderson WD, Treister NS, Mayeaux EJ, Nalliah RP (2015) Oral lesions you can’t afford to miss. J Farm Pract 64(7): 392-399.