Rehabilitation of Maxillary Defect for Adolescent Acute Lymphoblastic Leukemia (ALL) Patient with Acrylic Obturator
Jamal Saker 1* and Simindokht Zarrati2
1Fellowship student, Department of Prosthodontics, School of Dentistry, Tehran University of Medical Science, Iran
2Assistant Professor, Department of Prosthodontics, School of Dentistry, Tehran University of Medical Science, Iran
Submission: May 15, 2019; Published July 15, 2019
*Corresponding author: Jamal Saker, Department of Prosthodontics, School of Dentistry, Tehran University of Medical Science, Iran
How to cite this article: Jamal Saker, Simindokht Zarrati. Rehabilitation of Maxillary Defect for Adolescent Acute Lymphoblastic Leukemia (ALL) Patient 007 with Acrylic Obturator. J Child Adolesc Dent. 2019; 1(1): 555552.
Abstract
Acute lymphoblastic leukemia (ALL) is one of the most cancers that occur in adolescence and young adult. Despite the recovery of a large number of patients with this type of cancer, there are many complications and oral demonstration remain after healing, which related to leukemia itself or the treatment procedure including chemotherapy and radiotherapy. In general, most of acute lymphoblastic leukemia infected children have poor oral health and may encounter serious oral complication. In this clinical report we present a case of a child that had acute lymphoblastic leukemia and suffering from mucor mycosis in oral cavity, which lead to maxillary necrosis and oronasal connection. The defect in the maxilla, which was very debilitating, was treated by using acrylic obturator, to enhance patient self-confidence and quality of life
Keywords: Leukemia Maxillofacial Prosthesis Mucormycosis Palatal Obturator
Introduction
Acute lymphoblastic leukemia (ALL) is type of leukemia, or malfunction of the white blood cells, characterized by an increasing production and accumulation of immature white blood cells, known as lymphoblast. The term “acute” means that the leukemia can develop rapidly, and if not treated, would probably be fatal in a short period. Lymphocytic means it develops from immature lymphocytes. There is no specific age for onset of ALL but is more common in children (14 years and less) who represent close to 60% all cases [1].
Leukemia is generally classified as (1) acute lymphocytic, (2) acute myeloid, (3) chronic lymphocytic, and (4) chronic myeloid. Leukemia classification criteria depend on.
i. The similarity between the leukemic cells and normal cells (myeloid versus lymphoid).
ii. The clinical pathway of the disease (acute versus chronic) [2].
In a child with ALL, too many stem cells become lymphoblasts, B-lymphocytes, or T-lymphocytes. The cells do not work like normal lymphocytes and cannot fight infection very well [3]. The symptoms of ALL include fever, increased risk of infection (especially bacterial infections such as pneumonia.), increased tendency to bleed (due to thrombocytopenia), and expressive signs of anemia, including pallor, tachycardia (highheart rate), fatigue, and headache [4]. The oral manifestations that may be present are oral infections, ulceration, bleeding, and temporomandibular joint dysfunction mucositis, dysgeusia, xerostomia [5]. Acute leukemia Treatment may include chemotherapy, steroids, radiotherapy, intensive combined treatments (including bone marrow or stem cell transplants), and growth factors [6]. Generally, blood counts fall within a week of treatment and may take some time to recover, depending on the type and doses of drugs used. During this time, there is likely to be a need for antibiotics and other drugs to treat, or prevent infection. There is also likely to be a need for blood transfusions to treat severe anemia, and platelet transfusions to reduce the risk of bleeding [7]. Intensive chemoradiotherapy destroys the mucosal membrane of the mouth and throat and it is often associated with severe oral inflammation and infection, including herpes simplex, candidiasis, mucositis, and gingivitis [8-13]. In addition, these oral complications interfere with patients’ comfort, nutrition and may lead to a systemic infection that arises in the mouth [6,14].
Case Report
A 13-year-old adolescent suffered from high fever, and after being introduced to a local doctor who described antibiotic and analgesic the temperature got down, but a day later the temperature rose again. This situation has repeated severaltimes. No noticeable improvement was seen, and deterioration of the general situation of the child to the inability to breathe and turned the color of the body to yellow, and the appearance of red spots on the skin. He was transferred to Ali Asghar hospital where they diagnosed him with leukemia. However, two months after the first chemotherapy protocol, the patient felt pain in his teeth. So, he was sent to Alrasool Alkram hospital. Where they found that he had mucormycosis, he underwent a surgical operation to debride the infected bone, which was repeated several times in the following days. This child introduced to Tehran University of Medical Science (TUMS), school of Dentistry, Department of prosthodontics, with the chief complaint of oral nasal connection developed after surgical removal of the defected part of the maxilla and antibiotic therapy. Clinical examination of a patient showed loss of the central and lateral incisors canine and first premolar in the left side, severe bone resorption in the medial portion of second premolar with mobility class II.
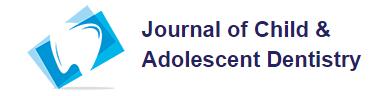
a) Wash the debris in the defect area with normal saline solution and evaluating the hard palate defect in the maxillary arch and determining if there is a need for further surgical or medical intervention the need for prosthetic intervention (Figure 1).
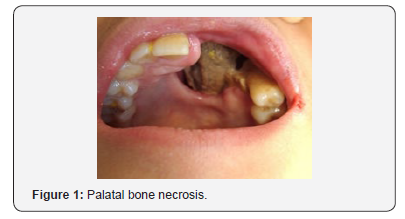
b) Preliminary impressions of upper and lower arch were recorded with irreversible hydrocolloid impression material (Jeltrate; DentsplyIntl, York, Pa) with plastic stock perforated trays. Impressions were poured with type-III dental stone and casts were obtained to fabricate the custom tray (Figure 2).
c) Border molding of the custom tray using modeling plastic impression compound (Impression CompoundType I; Kerr Corp, Orange, Calif) and make the definitive impression with (CharmFlex Polyvinyl Siloxane (PVS) Impression Material - Medium Body) (Figure 3).

d) Mounting the cast on an articulator (Hanau 96H2; Whip Mix Corp, Louisville, Ky) with a maxillomandibular relation record registered with an aid of the record base and occlusion rim.
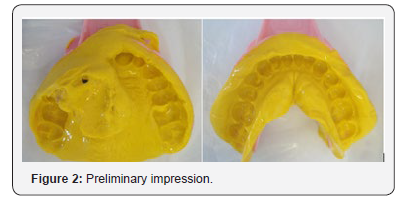
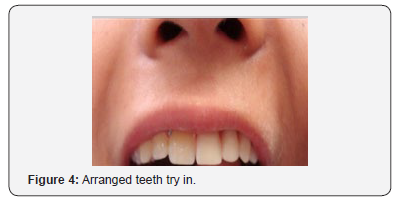
e) Evaluation the position of the artificial denture teeth arranged in the wax rim intraorally (Figure 4).
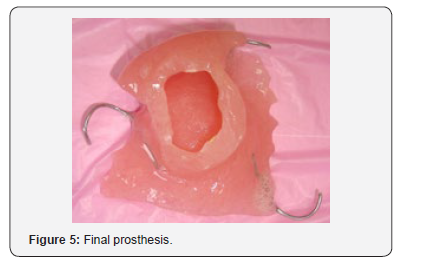
f) Processing the wax denture in heat-polymerized pink acrylic resin (Lucitone 199; Dentsply Intl) (Figure 5).
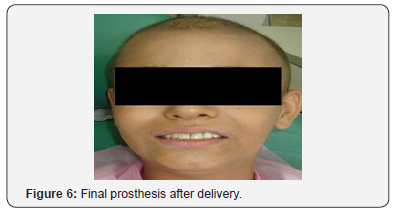
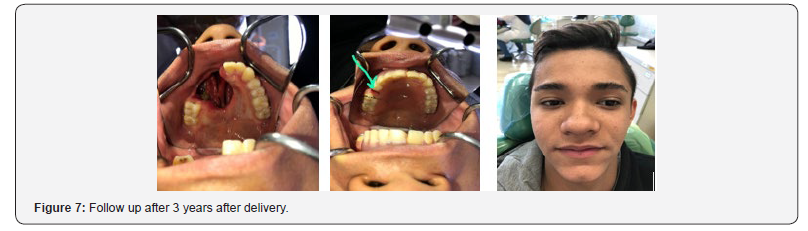
g) Inserting the completed obturator intraorally and evaluating the fitting using pressure-indicating paste (Mizzy, Inc; Cherry Hill, NJ), and equilibrate the occlusion. Evaluate the speech and swallowing functions and esthetics to ensure patient comfort (Figure 6). It was important to take into account the fact that this child was in the growthphase and constantly adjust the device to commensurate with the continued growth of the maxilla. Recall for the patient is usually done every 2 weeks due to rapid soft-tissue changes that occur within the defect during organization and healing of the wound. Follow up the patient after three years, a complete improvement in the patient’s condition was achieved and the Patient relieved completely from his illness. Our patient came to make some adjustment for his prostheses. He lost his left second premolar. We just added new tooth to his obturator and confirmed on oral hygiene care (Figure 7).
Discussion
Leukemia is a malignancy affecting the white blood cells of the bone marrow [5]. Palate perforation can occur due to trauma, bacterial infection such as osteomyelitis, Wegener’s granulomatosis, viral infection such as herpes zoster, fungal infection such as mucormycosis, aspergillosis, prolonged cocaine abuse, and malignancies [14]. Prosthetic rehabilitation of the palatal perforation with obturator by a maxillofacial prosthodontist has two primary objectives [15]:
i. To optimally restore the functions of mastication, deglutition, and speech thereby improving and enhancing the quality of life of these patients.
ii. To achieve normal oro-facial appearance
Conclusion
The increased risk for systemic fungal infection and the potential fatal consequences spread in patients receiving bone marrow transplants or antineoplastic therapy. And this have indicated the importance of prevention of, mucositis, ulceration, hemorrhage or infection because the condition can be exacerbated and lead to changes Irreversible bone necrosis that progressed in our patient and led to contact between the oral and nasal cavities. The oral health status of hospitalized children suffering from leukemia or other cancers is generally poor. They should be considered, as high-risk patients for oral complications and this situation require a special care and recurrent follow up session under supervision of well-trained dentists and medical teams.
References
- Seiter K, Sarkodee Adoo C, Talavera F, Sacher R A and Besa E C (2019) ed Acute Lymphoblastic Leukemia. Medscape Reference.
- MR Howard, PJ Hamilton (2008) Leukemia in Hematology, (3rd edn), Elsevier, Philadelphia, Pa, USA p: 33-66.
- Greenberg MS, Glick M. Ship, JA Burket's (2008) Oral Medicine 11th Hamilton, Ontario, BC Decker Inc p: 153-187.
- Beumer J, Marunick MT, Esposite SJ (2011) Maxillofacial Rehabilitation: Prosthodontic and Surgical Management of Cancer Related Acquired and Congenital Defects of the Head and Neck.3rd Quintessence Publishing Co Inc. USA, pp. 468.
- Jabbour E, Thomas D, Cortes J, Kantarjian HM, O Brien S (2010) Central nervous system prophylaxis in adults with acute lymphoblastic leukemia. Cancer 116(10): 2290-2300.
- (2014) Evolution of cancer treatments: Chemotherapy (PDF). Cancer.org American Cancer Society.
- Mukherjee S (2010) The emperor of all maladies: a biography of cancer. Simon and Schuster.
- Baliga AM, Brave VR, Vyas HA (1995) Oral mucosal lesions in patients with acute leukemias and related disorders due to cytotoxic therapy. J Indian Soc Pedod Prev Dent 13(1): 25-29.
- Carrega G, Castagnola E, Canessa A, Argenta P, Haupt R, et al. (1994) Herpes simplex virus and oral mucositis in children with cancer. Support Care Cancer 2(4): 266-269.
- Epstein JB, Vickars L, Spinelli J, Reece D (1992) Efficacy of chlorhexidine and nystatin rinses in prevention of oral complications in leukemia and bone marrow transplantation. Oral Surg Oral Med Oral Pathol 73(6): 682-689.
- Ferretti GA, Ash RC, Brown AT, Largent BM, Kaplan A, et al. (1987) Chlorhexidine for prophylaxis against oral infections and associated complications in patients receiving bone marrow transplants. J Am Dent Assoc 114(4): 461-467.
- McGaw WT, Belch A (1985) Oral complications of acute leukemia: prophylactic impact of a chlorhexidine mouth rinse regime. Oral Surg Oral Med Oral Pathol 60(3): 275-280.
- Weisdorf DJ, Bostrom B, Raether D, Mattingly M, Walker P, Pihlstrom B, et al. (1989) Oropharyngeal mucositis complicating bone marrow transplantation: prognostic factors and the effect of chlorhexidine mouth rinse. Bone Marrow Transplant 4(1): 89-95.
- Samanta DR, Senapati SN, Sharma PK, Shruthi BS, Paty PB, et al. (2009) Hard palate perforation in acute lymphoblastic leukemia due to mucormycosis – A case report. Indian J Hematol Blood Transfus 25(1): 36-39.
- Keyf F (2001) Obturator prostheses for hemimaxillectomy patients. J Oral Rehabil 28(9): 821-829.