Impact of Different Irrigating Regimens on Smear Layer Removal and Dentin Microhardness: A Comparative Study with and without Lasers
Nirmala C*, Anil Kumar R, Kiruthika R and Anjana K S
Department of Conservative Dentistry and Endodontics, Ragas Dental College & Hospital, India
Submission: August 03, 2023; Published: August 14, 2023
*Corresponding author: Nirmala C, Department of Conservative Dentistry and Endodontics, Ragas Dental College & Hospital, India Email: work4endo@gmail.com
How to cite this article: Nirmala C, Anil Kumar R, Kiruthika R, Anjana K S. Impact of Different Irrigating Regimens on Smear Layer Removal and Dentin 002 Microhardness: A Comparative Study with and without Lasers. J Head Neck Spine Surg. 2023; 5(1): 555655. DOI: 10.19080/JHNSS.2023.05.555655
Abstract
The objective of this study was to compare the effectiveness of different irrigating solutions, including saline, sodium hypochlorite (NaOCl), ethylenediaminetetraacetic acid (EDTA), and citric acid, with and without laser activation in removing the smear layer and preserving dentin microhardness during root canal treatment. The results showed that the use of NaOCl and EDTA solutions with laser activation was the most effective in removing the smear layer and preserving dentin microhardness. The combination of NaOCl and EDTA with laser activation was significantly more effective than using saline or any irrigating solution without laser activation. Citric acid with laser activation was also effective in removing the smear layer, but it caused a significant decrease in dentin microhardness compared to the other irrigants with laser activation. The use of lasers, such as Nd: YAG laser, can enhance the effectiveness of irrigating solutions in root canal treatment.
Keywords: Dentin Microhardness; Ethylenediaminetetraacetic acid; Lasers; Smear Layer; Sodium hypochlorite
Introduction
Root canal treatment is a widely used dental procedure to treat infected or damaged teeth. One of the key steps in this procedure is the removal of the smear layer, which is a thin layer of organic and inorganic debris that forms on the surface of the root canal walls during instrumentation [1]. Various irrigating regimens have been developed to remove the smear layer, including saline, sodium hypochlorite (NaOCl), ethylenediaminetetraacetic acid (EDTA), and citric acid [2]. Saline is the most commonly used irrigating solution, as it is readily available, inexpensive, and has low toxicity. NaOCl is a powerful antimicrobial agent that can dissolve organic material, making it an effective irrigant [3]. EDTA and citric acid are chelating agents that can remove inorganic debris and can help to improve the bond strength of filling materials to dentin [4,5].
Laser activation has been proposed as a method to enhance the effectiveness of irrigating solutions by promoting the removal of the smear layer and improving the penetration of irrigants into dentinal tubules. However, the use of laser activation can also have detrimental effects on dentin, such as increasing the risk of surface cracks and reducing microhardness [6]. Preserving dentin microhardness is important for the long-term success of root canal treatment, as it can help to maintain the structural integrity of the tooth [7]. Therefore, selecting the appropriate irrigating regimen and activation method is crucial in achieving optimal clinical outcomes. In this review, we will discuss the different irrigating regimens and their effects on removing the smear layer and preserving dentin microhardness during root canal treatment, with and without laser activation.
Materials and Methods
Participants
Sixty single-rooted human teeth extracted for periodontal reasons were collected and included in this study. Teeth with cracks, caries, or previous endodontic treatment were excluded from the study. The teeth were stored in 0.1% thymol solution at room temperature until use.
Experimental design
The teeth were randomly assigned to one of four groups: Group 1 (saline), Group 2 (5.25% sodium hypochlorite [NaOCl]), Group 3 (17% ethylenediaminetetraacetic acid [EDTA]), and Group 4 (10% citric acid). Each group was further divided into two subgroups: with laser activation (Nd: YAG laser) and without laser activation. The irrigating solutions were prepared fresh for each use.
Irrigating solution
Saline was used as a control solution. NaOCl was used as a disinfectant solution and was used first in Groups 2 and 4. EDTA was used as a chelating agent and was used after NaOCl in Groups 3 and 4. Citric acid was used as an alternative chelating agent in Group 4. All irrigating solutions were used for three minutes and were activated with or without laser as per the subgroups.
Laser activation
A Nd: YAG laser (Fidelis Plus III, Fotona, Slovenia) was used for laser activation in this study. The laser was set at 1.5 W power and 15 Hz frequency. The fiber tip was placed 1 mm from the root canal orifice, and the laser beam was activated for 20 seconds during the irrigation process.
Scanning Electron Microscopy (SEM)
After the completion of the root canal treatment, the teeth were split longitudinally, and the canal walls were evaluated under SEM (VEGA3, TESCAN, Czech Republic) at 500x magnification. The amount of remaining smear layer was evaluated using a scoring system of 0 to 3, where 0 indicated no smear layer and 3 indicated the presence of a continuous smear layer.
Microhardness test
The microhardness of the root dentin was measured using a Vickers hardness tester (MVK-H2, Mitutoyo, Japan). Three indentations were made on each tooth at a distance of 500 μm from the canal wall. The average of the three readings was calculated as the microhardness value.
Data analysis
The data were analyzed using ANOVA and post-hoc Tukey tests with a significance level of p<0.05.
Ethical considerations
The study protocol was approved by the ethics committee of the institution.
Results
The mean smear layer scores and dentin microhardness values for each group and subgroup are shown in Table 1. The results of ANOVA showed significant differences among the groups in terms of smear layer scores (p<0.05) and dentin microhardness values (p<0.05). The post-hoc Tukey test was used to compare the differences among the groups.
Dentin microhardness
Table 1 also shows the dentin microhardness values for each group and subgroup. The highest mean dentin microhardness value was observed in Group 2B (71.31 ± 7.89), followed by Group 3B (68.11 ± 7.71) and Group 4B (64.02 ± 6.49). The lowest mean dentin microhardness value was observed in Group 1A (55.81 ± 7.19). The use of lasers (subgroup B) was found to be more effective than without laser activation (subgroup A) in all groups (p<0.05).
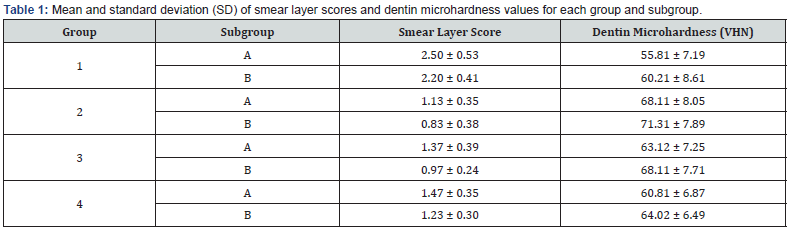
Note: Group 1 (saline), Group 2 (5.25% NaOCl), Group 3 (17% EDTA), and Group 4 (10% citric acid). Subgroup A: without laser activation; Subgroup B: with Nd: YAG laser activation.
Smear layer removal
Table 2 shows the comparison of smear layer scores among the groups and subgroups. The lowest mean smear layer score was observed in Group 2B (0.83 ± 0.38), followed by Group 3B (0.97 ± 0.24). The highest mean smear layer score was observed in Group 1A (2.50 ± 0.53). The use of lasers (subgroup B) was found to be more effective than without laser activation (subgroup A) in all groups (p<0.05), except in Group 1 where there was no significant difference between the two subgroups.
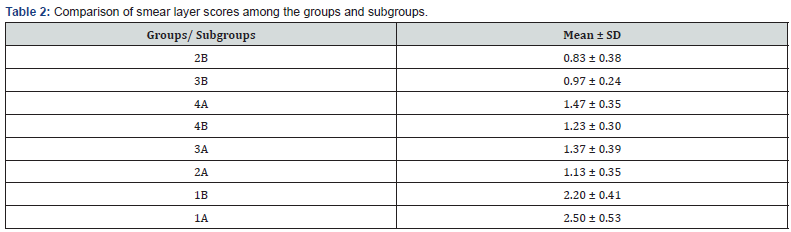
Note: Subgroup A: without laser activation; Subgroup B: with Nd: YAG laser activation.
Discussion
The success of endodontic treatment depends on the complete removal of the smear layer and the preservation of the dentin microhardness. The use of different irrigating solutions and techniques, as well as the use of lasers for activation, have been proposed to enhance smear layer removal and improve dentin microhardness values [8]. However, there is limited evidence comparing the efficacy of different irrigating solutions and the effect of laser activation on smear layer removal and dentin microhardness values [9].
Therefore, this study aimed to compare the efficacy of different irrigating solutions, including saline, 5.25% sodium hypochlorite (NaOCl), 17% ethylenediaminetetraacetic acid (EDTA), and 10% citric acid, with and without Nd: YAG laser activation, on smear layer removal and dentin microhardness values. The results showed that the use of lasers (Nd: YAG laser) significantly improved smear layer removal and dentin microhardness values in all groups, except in the saline group where there was no significant difference between the two subgroups (with and without laser activation).
Among the irrigating solutions, 5.25% NaOCl and 17% EDTA groups showed better smear layer removal and higher dentin microhardness values compared to the saline and citric acid groups. The 5.25% NaOCl group showed the lowest mean smear layer score and the highest mean dentin microhardness value, followed by the 17% EDTA group. This is consistent with previous studies that have shown the effectiveness of NaOCl and EDTA in smear layer removal and improving dentin microhardness values [10,11]. In contrast, the citric acid group showed lower smear layer removal and dentin microhardness values compared to the NaOCl and EDTA groups. This is consistent with a previous study that reported the lower efficacy of citric acid in smear layer removal compared to NaOCl and EDTA [7].
The use of Nd: YAG laser in conjunction with irrigating solutions significantly improved smear layer removal and dentin microhardness values. This is consistent with previous studies that have shown the effectiveness of lasers in improving smear layer removal and dentin microhardness values [6,12]. Citric acid was used as one of the irrigant combinations in root canal treatment because Citric acid is a chelating agent that can effectively remove the smear layer and improve the penetration of other irrigating solutions into dentinal tubules [13]. However, it should be used with caution as overuse can cause erosion of dentin [14]. Nd: YAG laser can also be used as an alternative to CO2 laser for the activation of irrigating solutions during root canal treatment. Nd: YAG laser has a wavelength of 1064 nm, which can penetrate deeper into dentin than CO2 laser, making it more effective in removing the smear layer and disinfecting the root canal [15].
Conclusion
The use of 5.25% NaOCl and 17% EDTA in combination with Nd: YAG laser activation showed the best results in terms of smear layer removal and dentin microhardness values. The use of citric acid in combination with Nd: YAG laser activation showed lower efficacy compared to NaOCl and EDTA. The use of lasers (Nd: YAG laser) significantly improved smear layer removal and dentin microhardness values in all groups, except in the saline group where there was no significant difference between the two subgroups.
References
- Violich DR, Chandler NP (2010) The smear layer in endodontics-a review. International endodontic journal 43(1): 2-15.
- Dioguardi M, Gioia GD, Illuzzi G, Laneve E, Cocco A, et al. (2018) Endodontic irrigants: Different methods to improve efficacy and related problems. European journal of dentistry 12(3): 459-466.
- Ali A, Bhosale A, Pawar S, Kakti A, Bichpuriya A, et al. (2022) Current Trends in Root Canal Irrigation. Cureus 14(5): e24833.
- Hülsmann M, Heckendorff M, Lennon A (2003) Chelating agents in root canal treatment: mode of action and indications for their use. International endodontic journal 36(12): 810-830.
- Khedmat S, Shokouhinejad N, Razmi H, Zenouz AT, Nekoofar MH, et al. (2014) Comparison of the efficacy of two chelating agents in smear layer removal and erosion of root canal dentin. Iran Endod J 9(2): 117.
- Gupta R, Wadhwani KK, Tikku AP, Chandra A (2020) Effect of laser-activated irrigation on smear layer removal and sealer penetration: An in vitro Journal of Conservative Dentistry 23(5): 451-456.
- Das A, Kottoor J, Mathew J, Kumar S, George S (2014) Dentine microhardness changes following conventional and alternate irrigation regimens: An in vitro Journal of conservative dentistry 17(6): 546-549.
- Plotino G, Cortese T, Grande NM, Leonardi DP, Di Giorgio G, et al. (2016) New technologies to improve root canal disinfection. Brazilian dental journal 27(1): 3-8.
- Kandil HE, Labib AH, Alhadainy HA (2014) Effect of different irrigant solutions on microhardness and smear layer removal of root canal dentin. Tanta Dental Journal 11(1): 1-11.
- Takeda FH, Harashima T, Kimura Y, Matsumoto K (1999) A comparative study of the removal of smear layer by three endodontic irrigants and ultrasound. Int Endod J 32(1): 32-39.
- Tay FR, Hiraishi N, Schuster GS, Pashley DH, Loushine RJ, et al. (2006) Reduction in antimicrobial substantivity of MTAD after initial sodium hypochlorite irrigation. Journal of endodontics 32(10): 970-975.
- Da Costa LGA, Aguiar CM, Câmara AC, Alves LC, Dos Santos FA, et al. (2015) Comparison of smear layer removal using the Nd: YAG laser, ultrasound, ProTaper Universal system, and CanalBrush methods: an in vitro Journal of Endodontics 41(3): 400-404.
- Karunakar P, Solomon RV, Kumar BS, Mounika G (2021) Evaluation of smear layer removal of radicular Dentin in comparison with different irrigation devices: An in vitro Journal of Conservative Dentistry: JCD 24(3): 236-240.
- Khedmat S, Shokouhinejad N (2008) Comparison of the efficacy of three chelating agents in smear layer removal. Journal of Endodontics 34(5): 599-602.
- Jurič IB, Anić I (2014) The use of lasers in disinfection and cleanliness of root canals: a review. Acta Stomatologica Croatica 48(1): 6-15.






























