A Rare Case of Traumatic Leptomeningeal Cyst in Adult: Case Report
Aneesh KM1* and Shahana N2
1Specialist Radiologist, NMC Medical Center, UAE
2 Specialist Radiologist, Amina Hospital, UAE
Submission: November 28, 2019; Published: December 06, 2019
*Corresponding author: Zheng-ming Zhu, The Second Affiliated Hospital, Nanchang University, Nanchang City, Jiangxi province, China
How to cite this article: Wen-jun Zhang, Zheng-ming Zhu. A Rare Case of Small Mesenteric Hiatus Not Closed After Ten Years of Roux-en-Y Choledochojejunostomy: Case Report. J Head Neck Spine Surg. 2019; 4(1): 555628. DOI: 10.19080/JHNSS.2019.04.555628
Abstract
Roux-en-Y choledochojejunostomy is a common bile duct reconstruction operation, which has a good surgical effect, and has a low chance of bile leakage and bile duct stenosis. The main complications are bleeding, infection, anastomotic leakage and stress ulcer, but unclosed mesenteric foramen of small intestine after Roux-en-Y choledochojejunostomy is rare. Therefore, in this report, we reviewed a case of the clinical data, imaging findings, and surgical status of a patient with unclosed mesenteric foramen of small intestine of ten years after Roux-en-Y choledochojejunostomy and hope to provide a case reference for clinicians.
Keywords: Roux-en-Y choledochojejunostomy Unclosed mesenteric foramen Surgery suture
Introduction
Roux-en-Y choledochojejunostomy has different complications in clinical [1,2], and it is rare to have a proximal unclosed mesenteric hiatus. In this case, the patient had an intermittent colic episode, which was considered as the possibility of intestinal volvulus by CT examination. The small intestinal volvulus was diagnosed by postoperative exploration, and the unclosed mesenteric hiatus of the small intestine was also found. Therefore, through this case report, it is hope that can help clinical diagnosis and treatment in this area.
General clinical data and CT findings of this patient
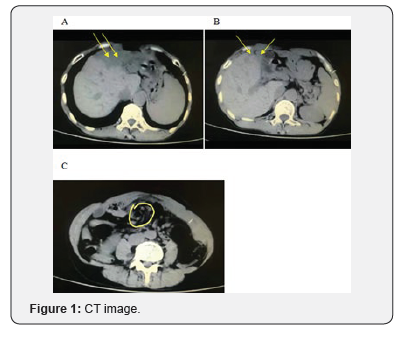
A 51-year-old female patient, recently the lower abdomen is painful for 2 days, and was admitted to the hospital for half a day with increased pain. This patient had a history of open choledochectomy, and Roux-en-Y choledochojejunostomy for more than 10 years. Examination revealed that the patient’s abdomen was soft, tenderness in the lower abdomen, no obvious rebound pain, and active bowel sounds. T: 36. 8℃, R: 19 /min, P: 78 /min, BP: 130 /80 mmHg. Abdominal CT examination showed that multiple dilatation of the intrahepatic bile duct, a large low-density shadow and a lower-density shadow could be seen in the left lobe of the liver, the position of the gallbladder fossa not shown the gallbladder, the density of the surrounding tissue was vague, and a small amount of free gas could be seen, the proximal small intestine stenosis and the thickened peritoneal adhesions could be seen (Figure 1). The image of intestinalvolvulus and mesenteric hiatus not closed.after Roux-en-Y choledochojejunostomy. A and B: Lamellar low-density shadows and the lower liquid density shadows can be seen in the left lobe of the liver, surrounding tissues are blurred, gas density shadows can also be seen, and dilatation of the intrahepatic and external bile ducts can be seen. C: Circular stenosis can be seen in the upper segment of the small intestine the density of intestinal wall is uniform. These images suggest that it may be intestinal volvulus, but the mesenteric hiatus cannot be found.
Operation situation
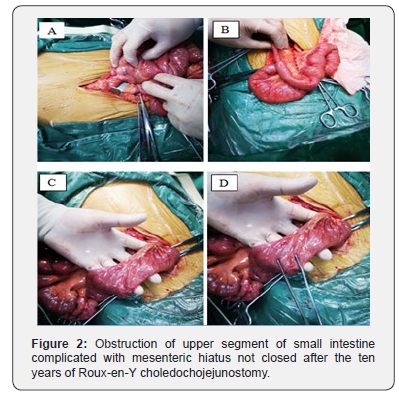
The patient was anesthetized and placed on the operating table, and then routinely the abdomen was disinfected, and the sterile sheet was paved. An incision was made in the midline of the abdomen, and then the abdominal wall, rectus abdominis, and rectus sheath was opened in order, and entered the abdominal cavity. The bowel was detected, it was found that the bowel at the proximal anastomosis of the upper segment of jejunum was twisted, resulted in intestinal stenosis and intestinal wall edema, and further exploration revealed that the unclosed mesenteric hiatus near the site of intestinal stenosis (Figure 2). After the reduction of intestinal volvulus, the mesenteric hiatus was sutured and closed, and then further detected whether there are any abnormalities in other intestines. Subsequently, the abdominal incision was sutured, and the wound was covered with sterile gauze. The bleeding and anastomotic leakage were not found during the operation. The map of obstruction of upper segment of small intestine complicated with mesenteric hiatus not closed. A: The site of volvulus of the small intestine, located the below anastomosis and the upper segment of the jejunum. B: The site of intestinal volvulus has been restored and shows the site of choledochojejunostomy. C and D: The site of the proximal mesenteric hiatus of the small intestine has shown and the mesenteric foramen is closed by stitching.
Discussion
Roux-en-Y choledochojejunostomy is to cut off and close the distal end of the jejunum about 15 cm from the duodenum jejunum, retain the broken suture for traction, and jejunumjejunostomy is performed at a distance of 55 cm from the jejunum [3]. It is one of the commonly used surgical methods in general surgery []. The main indications are as follows [4-6]:
a) Benign stricture of bile duct.
b) Some diseases requiring extrahepatic bile duct reconstruction (such as, choledochal cyst, choledochal malignant tumor or pancreatectomy, etc).
c) Liver transplantation is not suitable for end-to-end biliary anastomosis.
d) Common bile duct stricture caused by trauma, surgery or malignancy.
e) Distal common bile duct obstruction caused by malignant tumors of pancreas, duodenum and bile duct, and incarcerated stones. Roux-en-Y choledochojejunostomy has become an important surgical method for the treatment of biliary diseases, which can significantly improve biliary obstruction and relieve symptoms [7].
However, there are certain contraindications, mainly those with intrahepatic stenosis or stones above the common bile duct that have not been treated [8]. The long-term complications of the Roux-en-Y choledochojejunostomy are mainly bleeding, infection, anastomosis and leakage, and stress ulcers [9,10]. The main cause of postoperative bleeding is the peeling surface bleeding and the instability of vascular ligation during operation, while the coagulation factor or fibrinogen deficiency is also part of the cause of bleeding [11]. The principle for the treatment of postoperative bleeding is through blood transfusion, transfusion and correction of blood coagulation. If the vital signs can remain stable, the patients can continue to be treated conservatively, however, if the vital signs are unstable, it is necessary to reexplore in time to stop bleeding [12]. Patients can be cured by suing antibiotics after simple infection however, retrograde biliary infections are often secondary to anastomotic stenosis and stone formation [13]. The main causes of anastomotic stenosis and biliary fistula are the high position of the resected bile duct and small anastomosis diameter. Poor technique during operation, ischemia of the bile duct wall and scar contraction can also lead to anastomotic stenosis, which can further lead to poor bile drainage and intestinal reflux, cause reflux cholangitis and aggravate symptoms. Large caliber choledochojejunostomy or the use of a silicone tube to support the drainage tube can effectively prevent the development of the postoperative anastomosis stenosis and biliary fistula [14,15]. In this report, we reviewed a patient with Roux-en-Y choledochojejunostomy, due to this patient has a long postoperative time, we only considered the possibility of small bowel torsion before surgery. Fortunately, the location of the unclosed mesenteric hiatus in the small intestine was close to the intestinal torsion, so it was found during surgery. If neglected, serious consequences were brought to the patient after surgery. Therefore, we reported the clinical symptoms, CT imaging manifestations and surgical conditions of the patients accordingly, and as a reference for clinicians.
References
- Yang XW, Chen JY, Yan WL, Du J, Wen ZJ, et al. (2017) Case-control study of the efficacy of retrogastric Roux-en-Y choledochojejunostomy. Oncotarget 8(46): 81226-81234.
- Shamsaeefar A, Nikeghbalian S, Kazemi K (2017) Thirteen-Year Evaluation of the Management of Biliary Tract Complication After Deceased Donor Liver Transplantation. Prog Transplant 27(2): 192-195.
- Hashimoto R, Matsuda T, Aoki H, Okuzono T, Nakahori M (2017) Double-balloon assisted trans-anal ERCP in a patient with Roux-en-Y choledochojejunostomy. Gastrointest Endosc 85(6): 1298-1299.
- Huang C, Ning Z, Zhu Z (2019) Torsional Necrosis of an Output Loop Internal Hernia After Roux-en-Y Choledochojejunostomy: A Case Report. Front Surg 6: 51.
- Han JH, Lee JH, Hwang DW, Song KB, Shin SH, et al. (2018) Robot resection of a choledochal cyst with Roux-eny hepaticojejunostomy in adults: Initial experiences with 22 cases and a comparison with laparoscopic approaches. Ann Hepatobiliary Pancreat Surg 22(4): 359-366.
- Yamamoto M, Tahara H, Hamaoka M, Seiichi S, Shintaro K, et al. (2018) Utility of hepatobiliary scintigraphy for recurrent reflux cholangitis following choledochojejunostomy: A case report. Int J Surg Case Rep 42: 104-108.
- Saito R, Tahara H, Shimizu S, Ohira M, Ide K, et al. (2017) Biliary-duodenal anastomosis using magnetic compression following massive resection of small intestine due to strangulated ileus after living donor liver transplantation: a case report. Surg Case Rep 3(1): 73.
- Watson CJ, Rasmussen A, Jamieson NV, Johnston PS, Barnes ND, et al. (1995) Liver transplantation in patients with situs inversus. Br J Surg 82(2): 242-245.
- Jia CK, Lu XF, Yang QZ, Weng J, Chen YK, et al. (2014) Pancreaticojejunostomy, hepaticojejunostomy and double Roux-en-Y digestive tract reconstruction for benign pancreatic diseases. World J Gastroenterol 20(36): 13200-13204.
- DuCoin C, Moon RC, Teixeira AF, Jawad MA (2014) Laparoscopic choledochoduodenostomy as an alternate treatment for common bile duct stones after Roux-en-Y gastric bypass. Surg Obes Relat Dis 10(4): 647-652.
- Saeki Y, Ide K, Kakizawa H, Ishikawa M, Tashiro H, et al. (2013) Controlling the bleeding of jejunal varices formed at the site of choledochojejunostomy: report of 2 cases and a review of the literature. Surg Today 43(5): 550-555.
- Rezende-Neto JB, Petroianu A, Santana SK (2008) Subtotal splenectomy and central splenorenal shunt for treatment of bleeding from Roux en Y jejunal loop varices secondary to portal hypertension. Dig Dis Sci 53(2): 539-543.
- Fan C, Yan XP, Liu SQ, Wang CB, Li JH, et al. (2012) Roux-en-Y choledochojejunostomy using novel magnetic compressive anastomats in canine model of obstructive jaundice. Hepatobiliary Pancreat Dis Int 11(1): 81-88.
- Costa-Genzini A, Takahashi W, Dos Santos RG, Gaboardi MT, Noujaim HM, et al. (2012) Single-balloon enteroscopy for treating Roux-en-Y choledochojejunostomy stenosis after liver transplantation: a case report. Transplant Proc 44(8): 2503-2504.
- Suo T, Song LJ, Tong SX (2011) Gallstone in jejunal limb with jejunocolonic fistula 10 years after Roux-en-Ycholedochojejunostomy. World J Radiol 3(1): 38-40.






























