Incidence and Prognostic Factors in Distant Metastasis from Primary Head and Neck Cancer-An Institutional Experience
Raj V Nagarkar1, Ashvin P Wagh2 , Gauri S Kokane2*, Mayank Patil2 and Aditya M Markanday2
1Department of Surgical Oncologist, Curie Manavata Cancer Centre, India
2Department of Head and Neck Surgical Oncology, Curie Manavata Cancer Centre, India
Submission: November 15, 2017; Published: December 04, 2017
*Corresponding author: Gauri Kokane, Department of Head and Neck Surgical Oncology, Curie Manavata Cancer Centre, opposite Mahamarg Bus Stand, Mumbai Naka, Nashik, Maharashtra, India, Tel: +91 08424064382; Email: gaurikkn@gmail.com
How to cite this article: Raj V N, Ashvin P W, Gauri S K, Mayank P, Aditya M M. Incidence and Prognostic Factors in Distant Metastasis from Primary Head and Neck Cancer-An Institutional Experience. J Head Neck Spine Surg. 2017; 1(5): 555571.
Abstract
Introduction: Distant metastases adversely affect treatment planning as well as the overall prognosis of patient. The incidence of distant metastases is less in primary head and neck malignancy than other malignancies. objective of to calculate the median interval and to identify the frequency of occurrence as well as various risk factors for distant metastases in patients with head and neck squamous cell carcinomas.
Materials and Methods: Retrospective data of 500 patients operated at HCG Manavata cancer centre, Nashik for head and neck cancer was obtained from hospital management software system from year 2010 to 2014 with follow up of at least 2.5 year. The following variables were evaluated in relation to distant metastases: age, gender, TNM stage (I-IV), histological grade, and the site of origin of the tumor.
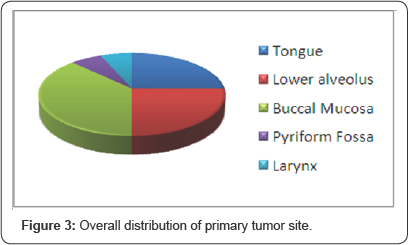
Results: Male to female ratio was 4.2:1, Distribution of primary site constituted buccal mucosa (25%), tongue (50%), lower alveolus (25%). Overall incidence of distant metastases in head and neck cancer was 3.2%.
Conclusion: Patients with advanced stage disease, higher histological grade as well as with extracapsular extension should be kept under close observation with periodic screening.
Keywords: Distant; Metastasis; Prognosis; Advanced stage
Introduction
In spite of tremendous progress in radiotherapy and chemotherapy in the past 3 decades, overall survival of head and neck cancer patient has not been significantly improved [1,2]. Distant metastases adversely affect treatment planning as well as the overall prognosis of patient. The incidence of distant metastases is less in primary head and neck malignancy than other malignancies. Location of primary tumor and clinical TNM staging significantly affects the incidence of distant metastasis and it is also influenced by the presence or absence of regional control above the clavicle. Primary tumors of advanced T stages in the hypopharynx, oropharynx and oral cavity are associated with the highest incidence of distant metastases. Distant metastasis is commonly seen in lung region accounting for 66%. It may be difficult to distinguish pulmonary metastasis from a new primary tumor, particularly if solitary. Other metastatic regions include bone (22%), liver (10%), skin, mediastinum and bone marrow. This retrospective study was conducted at HCG Manavata Cancer Centre, Nashik with the objective to calculate the median interval and to identify the frequency of occurrence as well as various risk factors for distant metastases in patients with head and neck squamous cell carcinomas.
Materials and Methods
Retrospective data of 500 patients operated at HCG Manavata cancer centre, Nashik for head and neck cancer was obtained from hospital management software system from year 2010 to 2014 with follow up of at least 2.5 year.
Inclusion criteria
a) Age 20 to 80 years of patient.
b) Patient with primary head and neck malignancy.
c) Patient with stage I, II, III, IV disease.
d) Both male and female sexes.
The following variables were evaluated in relation to distant metastases: age, gender, TNM stage (I-IV), histological grade, and the site of origin of the tumor. After treatment patients were followed up every month for atleast 1 year with regular screening for lung metastasis with chest x-ray and ultrasonography for any locoregional recurrence, after one year of regular follow up patient were recalled after every 3 months with routine investigation to rule out any distant metastasis. At our institute patients with advance stage disease has been put under close observation with yearly PET CT scan to rule out any occult distant metastasis.
Results

Male to female ratio in recurrent cases was 4.2:1 (Figure 1). Patients with primary tongue malignancy showed aggressive behaviour even in Stage I disease. The median interval was measured between confirmation of diagnosis to the occurrence of distant metastases. Average median interval with tongue primary and stage I disease was only 3 months. Our institutional experience of incidence of distant metastasis was accounting for 3.2% of cases.
In our study skeletal metastasis was observed in 2 5% of patients among all the distant metastasis. Patients with skeletal metastasis were mostly presented with stage III and stage IV disease while one patient was seen with stage I disease. 50% of the patients were having tongue as primary lesion while 25% of the patients were presented with buccal mucosa and lower alveolus as the primary each (Figure 2). Patients with multiple bony metastases were 25% with involvement of vertebrae, scapula, tibia and maxilla as compared to solitary metastasis which was found to be 75%. In our study extracapsular spread was observed in 75% of patients with skeletal metastasis, average median interval was observed to be 6.25 months. In this study skeletal metastasis is exclusively seen in male with 100% incidence. In our study distant failure rate was observed 3.2% out of which cutaneous metastasis was observed to be 31.25% which is quite high as compared to other study. Patients with cutaneous metastasis were presented with stage III and stage IV disease with one patient was observed to be a stage I disease and tongue primary. Average median interval for occurrence of distant metastasis was observed to be 118 months. Histological grading shows that patient with grade III diseases comprises of 40% compared to grade II which is 20% and grade I constituting 40% of cases. In our study liver metastasis was very rare and found in only one patient with rate of 6.25% of cases. In this patient median interval was 36 months which is quite good compared to other studies (Figure 3).

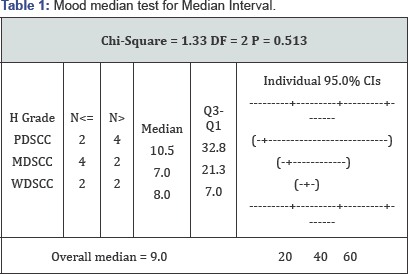
Mood's Median Test was used to derive relationship between histological grade and median interval. It showed that average median interval in PDSCC is 10.5 months; in moderately differentiated squamous cell carcinoma (MDSCC) it is 7 month whereas in well differentiated squamous cell carcinoma (WDSCC) it is 8 months. Variation of median interval in poorly differentiated squamous cell carcinoma (PDSCC) is comparatively larger as compare to the variation in other two groups. Statistically average median interval in all three category patients is nearby same (Table 1).
Table 1 show that average median interval in PDSCC is 10.5 months; in MDSCC it is 7 month whereas in WDSCC it is 8 months. Variation of median interval in PDSCC is comparatively larger as compare to the variation in other two groups. Statistically average median interval in all three category patients is nearby same.
Discussion
Squamous cell carcinoma of head and neck region commonly spread through the lymphatic spread while the non lymphatic spread accounts for approximately 10% of cases involving lungs, brain, bones and skin [3]. Risk factors for head and neck cancer metastasis have been already studied and confirmed that the increased risk of metastasis is associated with stage of disease, its histological grade, size of primary lesion and its site of occurrence with hypopharynx accounting 60%, base of tongue 53%, anterior tongue 50% [4]. Distant metastasis in head and neck cancer patient ranges from 6% to 43% in autopsy cases [2,5]. While according to Betka's review in his clinical studies it accounts for 8%-17% [6]. While in our study conducted at our institute the incidence of distant metastasis is quite low accounting for 3.2% of cases.
Skeletal metastasis
Squamous cell carcinoma of head and neck region predominantly metastasizes to lung which constitutes about 66% of distant metastases. Solitary pulmonary metastasis is difficult to distinguish from a new primary tumor SCC of head and neck region also metastasizes to bone (22%), liver (10%), skin, mediastinum and bone marrow [7]. In our study skeletal metastasis was observed in 25% of patients among all the distant metastasis. Patients with skeletal metastasis were mostly presented with stage III and stage IV disease while one patient was seen with stage I disease. In this study 50% of the patients were having tongue as primary lesion while 25% of the patients were presented with buccal mucosa and lower alveolus as the primary lesion each. Patient with multiple bony metastasis were 25% with involvement of vertebrae, scapula, tibia and maxilla as compared to solitary metastasis which was found to be 75%. In our study extracapsular spread was observed in 75% of patients with skeletal metastasis, which denotes extracapsular spread is a crucial factor in bone metastasis. Histological grade shows that patient with moderately differentiated squamous cell carcinoma (MDSCC) accounts for 75% of bone metastasis compared to well differentiated squamous cell carcinoma (WDSCC) with 25% of cases. Patients with skeletal metastasis has poor prognosis with disease free survival of only few months [8]. In our study average median interval was observed to be 6.25 months. Patients with multiple bone metastasis was having less median interval as compared to solitary metastasis. In this study skeletal metastasis is predominantly seen in male with 100% incidence in male patients.
Skin metastasis
Squamous cell carcinoma of head and neck region rarely metastasise to skin and associated with poor prognosis and progressive disease [9]. Incidence of distant cutaneous metastasis is in the range of 0.7% to 10% and is seen in breast and lung as primary tumor [10]. Incidence of cutaneous metastasis from squamous cell carcinoma of head and neck region is lower as compared to other primary malignancy and accounts for 0.8-1.3% [11]. In our study distant failure rate was observed 3.2% out of which cutaneous metastasis was observed to be 31.25% which is quite high as compared to other study. Patients with cutaneous metastasis were presented with stage III and stage IV disease with one patient was observed to be a stage I disease. Average median interval for occurance of distant metastasis was observed to be 118 months. Erythematous nodule which is commonly seen in cutaneous metastasis can be considered as infective foci several times [11]. Occurence of these skin nodule is represented as either solitary or multiple lesion [9]. According to Yoskovitch et al. [11] majority of skin nodule occurs above the diaphragm [11]. When the Cutaneous metastases appeared distally it is thought to be because of hematogenous route and when it is seen in close relation to primary tumor, spread is through dermal lymphatics [12]. In our study cutaneous metastasis was observed as multiple lesion which mimics the infection foci for which the necessary antibiotics were prescribed, and is seen close to incision line as well as close to primary tumor similar to other studies. Histological grading shows that patient with grade III diseases comprises of 40% compared to grade II 20% and grade I 40% of cases. In this study cutaneous involvement is seen in other sexes with equal predilection. According to cologlu et al. [12] cutaneous metastasis occurred when pulmonary circulation be bypassed via the azygous and vertebral venous systems and Batson's plexus [13].
Liver Metastasis
Head and neck squamous cell carcinoma rarely metastasises to liver, approximately seen in 4.4% of cases with poor prognosis and median survival of 4 months. In our study liver metastasis was very rare and found in only one patient with rate of 6.25% of cases. In this patient median interval was 36 months which is quite good compared to other studies. Ultrasound is considered to be a cheap and convenient method with fewer side effects for the diagnosis of liver metastasis while in our cancer centre PET CT scan is choice of treatment to rule out any distant metastasis. Patients with single hepatic nodule in head and neck cancer can be screened with ultrasound associated a normal liver function if LDH elevation should be the only biological sign of alert [14].
Lung metastasis
Lung is the most common distant site of metastasis from squamous cell carcinoma of head and neck region which accounts for 66% [4]. Pulmonary metastasis is difficult to distinguish from new primary tumors of lung. In our study lung metastasis was found to be 37.5% suggesting most common site of distant metastasis compared to other sites and almost equal to other studies. Patients with lung metastasis were presented with stage II and stage III disease, most common site of primary tumor were buccal mucosa followed by tongue and larynx. Histological grade shows that patient with grade III disease accounts for 80% of the cases with lung as distant metastasis site. In this study lung involvement is purely seen in male patients. Patient's primary tumor and lymph node status is the risk factor for lung metastasis. In such scenario preoperative radiographic imaging such as CT thorax should be done to rule out distant pulmonary metastasis. In post op status annual chest x-ray is sufficient to check for lung metastasis but at the same time patient's with high risk factor requires chest x-ray after every 3-6 months. Patient's with locoregionally controlled disease but because of the aggressive nature of primary tumor such as adenoid cystic carcinoma as well as basaloid cell carcinoma requires extensive evaluation.
Conclusion
Extracapsular spread was associated with increased chance of skeletal metastasis. Patients with multiple skeletal metastases indicated poor prognosis compared to solitary bone metastasis. Tongue primary shows aggressive behaviour as compared to others. Patients with poorly differentiated SCC also expressed poor prognostic curve. Patients with advanced stage disease, higher histological grade as well as with extracapsular extension should be kept under close observation with periodic screening.
References
- Buckley JG, Ferlito A, Shaha AR, Rinaldo A (2001) The treatment of distant metastases in head and neck cancer present and future. ORL 63: 259-264.
- Taneja C, Allen H, Koness RJ, Radie-Keane K, Wanebo HJ (2002) Changing patterns of failure of head and neck cancer. Arch Otolaryngol Head Neck Surg 128(3): 324-327.
- Marioni G, Blandamura S, Calgaro N, Ferraro SM, Stramare R, et al. (2005) Distant muscular (gluteus maximus muscle) metastasis from laryngeal squamous cell carcinoma. Acta Otolaryngol 125(6): 678-682.
- Kotwall C, Sako K, Razack MS, Rao U, Bakamjian V, et al. (1987) Metastatic patterns in squamous cell cancer of the head and neck. Am J Surg 154: 439-442.
- Al-Othman MO, Morris CG, Hinerman RW, Amdur RJ, Mendenhall WM (2003) Distant metastases after definitive radiotherapy for squamous cell carcinoma of the head and neck. Head Neck 25(8): 629-633.
- Betka J (2001) Distant metastases from lip and oral cavity cancer. ORL J Otorhinolaryngol Relat Spec 63(4): 217-221.
- Ferlito A, Shaha AR, Silver CE, Rinaldo A, Mondin V (2001) Incidence and sites of distant metastases from head and neck cancer. ORL J Otorhinolaryngol Relat Spec 63(4): 202-207.
- Bhandari V, Jain RK (2013) A retrospective study of incidence of bone metastasis in head and neck cancer. J Cancer Res Ther 9(1): 90-93.
- Pitman KT, Johnson JT (1999) Skin metastases from head and neck squamous cell carcinoma: incidence and impact. Head Neck 21(6): 560-565.
- Wollina U, Graaefe T, Konrad H, Schonlebe J, Koch A, et al. (2004) Cutaneous metastases of internal cancer. Acta Dermatoven APA 13(3): 79-84.
- Yoskovitch A, Hier MP, Okrainec A, Black MJ, Rochon L (2001) Skin metastases in squamous cell carcinoma of the head and neck . Otolaryngol Head Neck Surg 124(3): 248-252.
- Caloglu M, Uygun K, Altaner S, Uzal C, Kocak Z, et al. (2006) Nasopharyngeal carcinoma with extensive nodular skin metastases: A case report. Tumori 92(2): 181-184.
- Marcy PY, Magné N, Bailet C, Pivot X, Dassonville O, et al. Liver metastases from head and neck squamous cell carcinomas: radiological






























