Platysmal Myocutaneous Flap for Reconstruction of T1,T2 Tongue Cancer: Functional Assessment
Anshuman Kumar1*, Srikanth Bitra2 and Sowdepalli Avinash3
1Director Surgical Oncology, Dharamshila Narayana Superspeciality Hospital, New Delhi
2Fellows Head & Neck Oncology, Dharamshila Narayana Superspeciality Hospital, New Delhi
2DNB Fellow Surgical Oncology, Dharamshila Narayana Superspeciality Hospital, New Delhi
Submission: September 11, 2017; Published: October 17, 2017
*Corresponding author: Anshuman Kumar, Director Surgical Oncology, Dharamshila Narayana Superspeciality Hospital, C3 healthcare, 115, Vardhman Sunrise Plaza, vasundhara Enclave, Delhi- 110096, India, Email: dranshumankumar@gmail.com
How to cite this article: Anshuman K, Srikanth B, Sowdepalli A. Platysmal Myocutaneous Flap for Reconstruction of T1,T2 Tongue Cancer: Functional Assessment. J Head Neck Spine Surg. 2017; 1(4): 555566.
Keywords: Platysma myocutaneous flap (PMF); Tongue reconstruction; Speech evaluation; Swallowing evaluation; Wound complications
Introduction
The platysma myocutaneous flap (PMF) was first used for intraoral reconstruction in 1978 by Futrell (Futrell et al., 1978) [1]. A platysma myocutaneous flap is a versatile, easy-to-perform, one-stage procedure, and the outcome is best in adequately selected patients, with minimum donor site morbidity. It is large enough to close most head and neck ablative skin or mucosal defects up to 70cm2 and no special equipment is required (Koch, 2002) [2]. The PMF is also an excellent alternative choice to microvascular flaps, especially in patients who are medically unfit for prolonged surgery [3]. But PMF is not as popular as other options of head and neck reconstructive, because of different reasons. The main limitations are lack of bulk, problematic blood supply and unreliability. Also the rates of complications between 10% and 40% have been reported, which includes partial or complete necrosis, fistula, dehiscence, hematoma and infection [4]. The rates of complications have been linked to surgeon’s experience, technique followed and other preoperative factors. In this study we describe our experience with the use of PMF in reconstruction of T1, T2 malignant lesions of tongue. The main objective of our study is to evaluate the feasibility of PMF in tongue reconstruction. And also to evaluate the functional outcome in terms of speech and swallowing, after tongue reconstruction with PMF.
Materials and Methods
In this descriptive study, a total of 75 non-consecutive patients of T1 and T2 tongue cancer, undergoing treatment at Dharamshila Narayana superspeciality Hospital, New Delhi were retrospectively evaluated by collecting data from the period from 2013 to 2016. In our series, newly diagnosed squamous cell carcinoma cases of tongue malignancy of only T1 and T2 lesions with no previous surgery and radiotherapy were included. All patients underwent adequate glossectomy and modified radical neck dissection. Histologically, we confirmed tumor free margin of resection by using a frozen section technique. The size of the flap was designed according to the anticipated defect resulting from the excision of the primary tumor.
Operative procedure
In this descriptive study, a total of 75 non-consecutive patients of T1 and T2 tongue cancer, undergoing treatment at Dharamshila Narayana superspeciality Hospital, New Delhi were retrospectively evaluated by collecting data from the period from 2013 to 2016. In our series, newly diagnosed squamous cell carcinoma cases of tongue malignancy of only T1 and T2 lesions with no previous surgery and radiotherapy were included. All patients underwent adequate glossectomy and modified radical neck dissection. Histologically, we confirmed tumor free margin of resection by using a frozen section technique. The size of the flap was designed according to the anticipated defect resulting from the excision of the primary tumor.

The anticipated skin paddle was outlined in the lower anterio-lateral neck making it an island. The parallel vertical incision was outlined, starting at the chin medially and the tip of the mastoid process laterally with extension of 2 to 2.5cm above the clavicle bone inferiorly. Depend the skin incision of designed skin paddle up to platysma muscle. Complete the neck incision from chin to mastoid tip and up to platysma muscle.Separate the myocutaneous paddle in supra platysmal plane by sharp dissection up to angle of mandible. External jugular vein is isolated for purpose to take it along the flap in subplatysmal plane for adequate venous drainage. Then elevate the paddle of flap in subplatysmal plane in an inferior to superior direction taking care to avoid underlying fat and lymphatic tissue with flap. Meticulous and sharp dissection preferably with bipolar cautery is done while removing submandibular gland and preserve facial vein and facial artery intact with its submental branch which serve as main arterial supply to flap [5] (Figure 1).
Post operatively, patients are evaluated for a period of six months to one year and assessment of tongue mobility, speech, swallowing, and surgical complications of flap as well as neck wound were done.
Speech was evaluated by AYJNIHH 7- point speech intelligibility rating scale [6].
This 7- point rating scale is as follows:
- No noticeable differences from normal.
- Intelligible though some differences occasionally noticeable.
- Intelligible although noticeably different.
- Intelligible with careful listening although some words unintelligible.
- Speech is difficult to understand with many words unintelligible.
- Usually is unintelligible.
- Unintelligible.
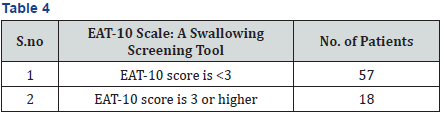
Swallowing assessment was done by EAT-10 scale [7]. This scale rates swallowing function, based on the patient’s responses to questioning, on scale maximum points of 40. If the EAT-10 score is 3 or higher, it indicates swallowing difficulties. This scale have 10 questions with a score of 0 to 4. The score 0 indicates no problem and score 4 indicates severe problem. As the score increases the severity increases.
The questionnaire is as follows:
- My swallowing problem has caused me to lose weight (0-4).
- My swallowing problem interferes with my ability to go out for meals (0-4).
- Swallowing liquids takes extra effort (0-4).
- Swallowing solids takes extra effort (0-4).
- Swallowing pills takes extra effort (0-4).
- Swallowing is painful (0-4).
- The pleasure of eating is affected by my swallowing (0-4 )
- When I swallow food sticks in my throat (0-4).
- I cough when I eat (0-4).
- Swallowing is stressful (0-4).
Tongue mobility is evaluated by asking patient to touch the upper lip, right commisure and left commisure with tip of the tongue. The surgical complications of flap that are assessed, include partial and complete loss of flap, flap detachment, marginal necrosis, fistulisation and partial epidermolysis.
The neck wound healing status is also evaluated as follow: normally healed, wound dehiscence, skin flap necrosis and wound contraction. The criterion used to differentiate between extended or regular wound dehiscence was the presence of a “dehiscent area” ≥ 2cm2. Skin flap necrosis was defined as wide when it affected an area of 2 cm2 or more [7].
Mobility of tongue (To upper lip/Right commissure/Left commissure): Tongue mobility evaluated by asking patient to touch the upper lip, right commisure and left commisure with tip of the tongue.
Results
A total of seventy five patients with T1 and T2 tongue cancer were included in the study. The histologic diagnosis was squamous cell carcinoma in all cases. All patients underwent curative Adequate glossectomy with modified radical neck dissections. Complications of the flap, Status of the neck Flap, Swallowing and speech function and tongue mobility were evaluated 6 months to 1 year postoperatively.
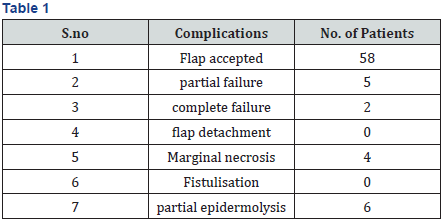
Complications of the flap
Flap complications were noted in 17 patients (22.6%) with complete failure in 2 patients (2.6%), which was managed by complete wound debridment and allowed healing with secondary intension. Partial failure in 5 patients (6.6%) was managed by local measures, such as surgical wound debridement of necrotic tissue. Marginal necrosis and partial epidermolysis is seen in 4 patients (5.3%) and 6 patients (8%) respectively. These complications need prolonged nasogastric nutrition for 15 days (Table 1).
Neck wound complications
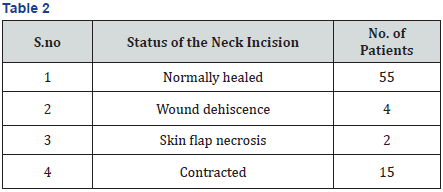
Neck wound complications were divided into four categories in which 55(73.3%) cases had normal healing of neck incision flap (Figure 2). Wound dehiscence and skin necrosis reported in 4(5.3%) and 2(2.6%) respectively, required surgical revision. Most of the patients 15(20%) reported with contraction and neck stiffness which was treated by neck physiotherapy (Table 2).

Speech
After excision of primary lesion and platysma flap reconstruction, intelligibility fell to grade 6 in two (2.6%) patient, Grade 5 in three (4%) patient, and grade 4 in five (6.6) patients. More patients showed intelligible although noticeably different in 27(36%) patients and intelligible though some differences occasionally noticeable in 38(50.6%) patients (Table 3).
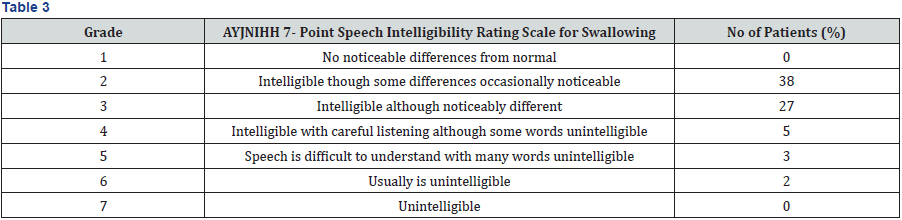
(“1” = no noticeable differences from normal, “7” = unintelligible).
Swallowing

Mobility of tongue
In these adequate glossectomy patients with platysma flap reconstruction, tongue mobility was evidently recovering, and mostly adequate for producing intelligible speech. Tongue mobility in Upper lip, Right commissure, and Left commissure seen in 47 (62.6%) patients. One side restricted movements mostly towards reconstructed site in 13(17.3%) patients. Two side restricted movements and completely restricted tongue mobility is seen in 9(12%) patients and 6(8%) patients respectively (Table 5).
Discussion
The primary blood supply to PMF derives from sub mental artery which branches from a facial artery and additional blood supply comes inferiorly from the cervical transverse vessels, medially from thyroid vessels and laterally from occipital and postauricular vessels. This is a multiaxial blood supply as it has multiple anastomoses with ipsilateral and contralateral mental, labial and sublingual arteries [8-10].
In our study of the 75 patients we preserve the facial artery and external jugular vein. External jugular vein provides retrograde valve less communication with internal jugular vein through retromandibular and facial venous system, which allows adequate venous drainage.
The experience about reliability of platysma flap is not uniform among the various authors, some author claim excellent results, while others experienced the poor results [11]. Our results showed 77.3% of complete acceptance of the flap (Figure 3-5) while remaining 2.6% shows complete failure(2cases) and 6.6% (5 cases) were partial loss of the flap. Marginal necrosis and partial epidermolysis is seen in 4 patients (5.3%) and 6 patients (8%) respectively. The rates of necrosis of platysma myocutaneous flap found in many other studies ranged from 7.1 to 29.2% [11].



In tongue reconstruction, restoration of speech is an important component. After excision of primary lesion and platysma flap reconstruction, intelligibility fell to Grade 6 in only two (2.6%) of patients, Grade 5 in three (4%) patients, and grade 4 in five (6.6) patients. Majority of patients showed Grade 3 (intelligible although noticeably different) patients and Grade 2 (Intelligible though some differences occasionally noticeable) in patients. Similar results were reported in a study where majority had speech restoration without significant deficits in a month after surgery [12].
Thin and pliability of this flap allows reconstructed tongue with good mobility. Good mobility of tongue is seen in 47(62.6%) patients and restricted tongue mobility is seen in 15(20%).
Conclusion
In conclusion, surgeons should consider the option of using a platysma myocutaneous flap when reconstructing tongue defects. The main advantages are that this flap is readily available, easy to perform, can be obtained during neck dissection and the donor site can be closed in a primary way, with minimal flap complications and good functional outcome. Results can be compared with free flap reconstruction.
References
- Futrell JW, Johns ME, Edgerton MT, Cantrell RW, Hugh GSF (1978) Platysma myocutaneous flap for intraoral reconstruction. Am J Surg 136(4): 504-507.
- Koch WM (2002) The platysma myocutaneous flap: underused alternative for head and neck reconstruction. Laryngoscope 112(7 Pt 1): 1204-1208.
- Tosco P, Demo PG, Ramieri G, Tanteria G, Pecorari G, et al. (2012) The platysma myocutaneous flap (PMF) for head and neck reconstruction: A retrospective and multicentric analysis of 91 T1-T2 patients. Journal of Cranio-Maxillo-Facial Surgery 40(8): e415-e418.
- Pagani D, Capaccio P, Fontanella W, Sambataro G, Broich G, et al. (2007) Vertical Platysma Myocutaneous Flap Reconstruction for T2-staged Oral Carcinoma. Anticancer Res 27(4C): 2961-2964.
- Verschuur HP, Dassonville O, Santini J, Vallicioni J, Poissonnet G, et al. (1998) Complications of the myocutaneous platysma flap in intraoral reconstruction. Head Neck 20(7): 623-629.
- Speech.
- Belafsky PC, Mouadeb DA, Rees CJ, Pryor JC, Postma GN, et al. (2008). Validity and reliability of the Eating Assessment Tool (EAT-10). Ann Otol Rhinol Laryngol 117(12): 919-924.
- Coleman JJ, Jurkiewicz MJ, Nahai F, Mathes SJ (1983) The platysma musculocutaneous flap: Experience with 24 cases. Plast Reconstr Surg 72(3): 315-323.
- Rabson JA, Hurwitz DJ, Futrell JW (1985) The cutaneous blood supply of the neck: Relevance to incision planning and surgical reconstruction. Br J Plast Surg. 38(2): 208-219.
- Gal TJ, Futran ND (2002) Outcomes research in head and neck reconstruction. Fac Plast Surg 18(2): 113-117.
- Peng LW, Zhang WF, Zhao JH, He SG, Zhao YF (2005) Two designs of platysmal myocutaneous flap for reconstruction of oral and facial defects following cancer surgery. Int J Oral Maxillofac surg 34(5): 507- 513.
- Rufat ML, Cristobal BN, Fillat ES, Ruiz de la Cuesta Martín D (2014) Platysma Flap: An Alternative to Free Flaps. J. Maxillofac Oral Surg 13(2): 84-86.






























