Attention to C-Spine in Craniofacial Trauma-An Update
Deepak Bhimana*
Consultant Oral and Maxillofacial Surgeon, India
Submission: September 01, 2017; Published: September 18, 2017
*Corresponding author: Deepak Bhimana, Consultant Oral and Maxillofacial Surgeon, India, Email: deepak.bhimana@gmail.com
How to cite this article: Deepak B. Attention to C-Spine in Craniofacial Trauma-An Update. J Head Neck Spine Surg. 2017; 1(3): 555564.
Abstract
The evolution of research and techniques in management of a trauma patient has reduced the mortality rate significantly in the golden hour. Severe maxillofacial and neck trauma exposes patients to life threatening complications such as airway compromise and hemorrhagic shock. These conditions require rapid actions (diagnosis and management) and a strong interplay between first level health care providers, surgeons and anesthesiologists. The cases with pan facial trauma need at most scrutiny due to proximity to cranial and cervical structures. In this article an insight into the C-spine injuries in a pan facial trauma patient has been discussed.
Keywords: C-spine injury; Craniofacial trauma
Introduction
Maxillofacial injuries are frequent cause of presentations in an emergency department. Varying from simple, common nasal fractures to gross combination of the face, management of such injuries can be extremely challenging. Injuries of this highly vascular zone are complicated by the presence of upper airway and proximity with the cranial and cervical structures that may be concomitantly involved. The usual techniques of airway breathing and circulation (ABC) management are often modified or supplemented with other methods in case of maxillofacial injuries [1]. Polytrauma patient admitted to hospital may have injury to cervical spine which is not immediately obvious. Because patient is neurological normal, with no neck pain or patient is having distracting pain or patient is unconscious. In case where there is no clear indication of cervical spine injury, however, patients still needs to be evaluated for cervical spine injuries because an unstable cervical spine injury could to delayed & result in neurological deterioration. Cervical spine injuries have been reported to occur in up to 3% of patients with major trauma and up to 10% of patients with serious head injury [2].
Neck Anatomy
It is useful to divide the anatomical structures of the neck into five major functional groups, to facilitate and ensure a comprehensive assessment and surgical approach:
- Airway - pharynx, larynx, trachea, lung.
- Major blood vessels-carotid artery, innominate artery, aortic arch, jugular vein, subclavian vein.
- Gastrointestinal tract-pharynx, esophagus.
- Nerves - spinal cord, brachial plexus, cranial nerves, peripheral nerves.
- Bones-mandibular angles, styloid processes, cervical spine.
The platysma defines the border between the superficial and the deep structures of the neck. If a wound does not penetrate deep to the platysma, it is not classified as a significant penetrating neck wound. As transverse cervical veins running superficial to the platysma may bleed profusely when severed, they are easily controlled by direct pressure, and can be managed by a simple ligature. The sternocleidomastoid muscle divides the neck into the posterior triangle which contains the spine and muscles, and the anterior triangle which contains the vasculature, nerves, airway, esophagus and salivary glands [3].
When evaluating penetrating neck injuries, the neck is divided into three anatomic zones for purposes of initial assessment and management planning:
- Zone I: Extends between the clavicle/suprasternal notch and the cricoid cartilage (including the thoracic inlet).Surgical access to this zone may require thoracotomy or sternotomy. Major arteries and veins, trachea and nerves, esophagus, lower thyroid and parathyroid glands and thymus are in this zone.
- Zone II: Lies between horizontal lines drawn at the level of the cricoid cartilage and the angle of the mandible. It contains the internal and external carotid arteries, jugular veins, pharynx, larynx, esophagus, recurrent laryngeal nerves, spinal cord, trachea, upper thyroid and parathyroid glands.
- Zone III: Extends between the angle of the mandible and base of skull. It contains the extracranial carotid and vertebral arteries, jugular veins, cranial nerves IX–XII and sympathetic nerve trunk [4].
Cervical Spine and Maxillofacial Trauma
In a complex maxillofacial trauma scenario, cervical spine fracture should always be considered unless proven otherwise. Because of the proximity of cervical spine any force of such magnitude that causes facial fractures can potentially traumatize the c-spine and its ligamentous attachments [5].
Clinical awareness about the status of cervical spine is achieved using the most commonly used three evidence-based decision protocols, Nexus criteria [6], Canadian spine rule [7], Harbor view criteria [8]. In patients who are awake, clearance protocol can be effectively implemented by a detailed clinical examination; however, in an unconscious patient, it is not possible. The clearance of such patients hinges on clinical examination, risk, and radiographic examination such as noncontract computerized tomography, static flexon extension radiography, magnetic resonance imaging, and dynamic fluoroscopy [1,9].
Anderson et al. [10] reviewed cervical spine clearance in blunt trauma patients and classified patients based on their symptoms and ability to provide a reliable evaluation. Patients are acutely categorized into one of four groups
a) Asymptomatic: There are two main protocols for cervical clearance in the asymptomatic patient that have been and continue to be widely utilized:
i. National Emergency X-Radiography Utilization Study (NEXUS) Low-Risk Criteria (NLC) [6] and
ii. Canadian Cervical-Spine Rule (CCR) [7,11].
b) Temporarily non-assessable: Temporarily non assessable patients have a transient inability to provide a reliable examination. These patients are expected to resume their baseline cognitive function and be evaluable within 24-48 hours. Harris et al. [11] reported on this group of patients and found that most common factors in the category of temporarily non assessable are drug/alcohol intoxication, concussion, or pain from distracting injuries. Once the patient has regained adequate cognitive function and is deemed clinically asymptomatic after a comprehensive examination, he or she can be treated as such and cleared clinically without imaging. If a patient is presumed to regain his or her normal baseline cognitive function within the 24-48 hours time but cervical clearance becomes more urgent, such as when surgical intervention is required for other injuries, the individual can be evaluated as an obtunded patient with advanced imaging. The most common guideline for this patient population is to have them undergo a multi-detector CT scan and/or maintain their cervical collar [11].
c) Symptomatic: Symptomatic patients are those with neck pain, tenderness, or neurologic symptoms. This subgroup requires spinal imaging. The various imaging options include static and dynamic plain radiographs, CT, and MRI. Each of these various imaging methodologies has specific advantages and disadvantages, not only regarding sensitivity and specificity but also in terms of timing and cost. Plain radiography is one of the earliest imaging modalities and is currently readily available, fast, and low cost in comparison to other types of studies. In patients with suspected spine trauma, plain radiographic evaluation has been shown to have a wide range of reported sensitivity for cervical spine injuries ranging from 31.6 to 52% depending on the study [11,12].
d) Obtunded: Cervical spine clearance in the obtunded patient is the most controversial aspect and focuses mainly on whether an MRI is necessary in addition to a negative MDCT. Though an exceedingly rare incident, isolated neurologic injury does occur and can lead to significant morbidity. The percentage of acute trauma patients who are obtunded at the time of evaluation ranges from about 20 to 30% [3,11,13].
Diagnostic Imaging
Plain radiography
The lateral view is 83% sensitive and 97% specific for detecting cervical spine fracture. Adding an open mouth view and AP view increases sensitivity to nearly 100%. The open mouth view is essential for excluding C1 arch or C2 odontoid process fractures. The AP view assesses alignment of uncovertebral joints and spinous processes. Oblique views can be used to assess facet joints, pedicles, and lateral mass, especially at the cervicothoracic junction. If the cervico-thoracic junction cannot be visualized on the lateral view, obtain a swimmer’s lateral view or a CT scan.
Obtain a CT scan if the patient has normal x-rays but persistent cervical tenderness and pain. Flexion extension views are not useful in the acute setting. Pain and discomfort preclude adequate motion to assess for ligamentous injuries. Only perform a flexion-extension view on an alert patient under supervision. Flexion with an occult ligamentous injury may precipitate neurologic injury [2,14,15].
CT scan
A CT scan is useful for determining the presence and extent of osseous injury. In fact, it is superior to MRI in this situation. In blunt trauma patients, CT scan detects 99.3% of cervical spine fractures. Injuries in the transverse plane may be missed on axial cuts, i.e., odontoid fractures. It is essential to obtain coronal and sagittal reconstructions [2,16].
MRI
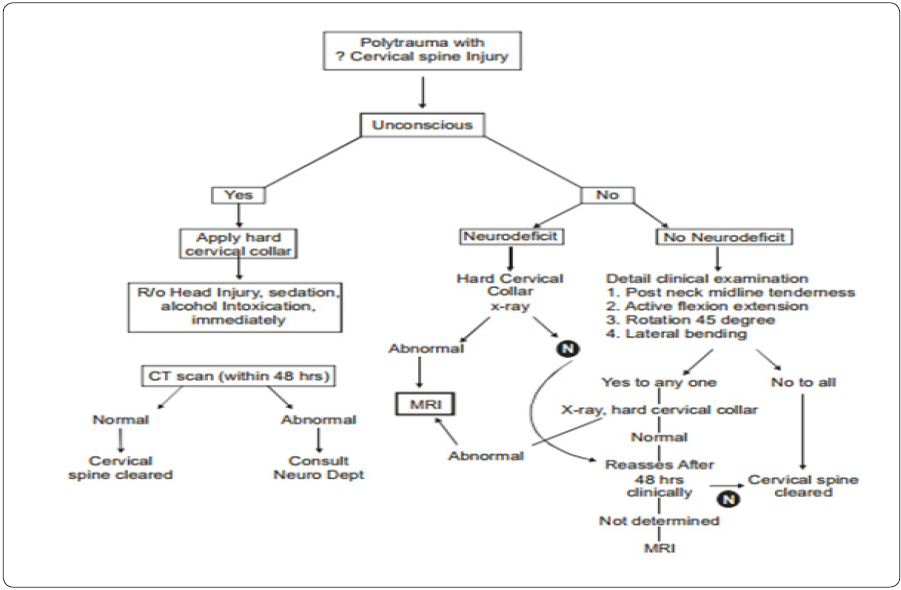
MRI is indicated for evaluating neurologic deficits and ligamentous injuries.MRI is superior to CT for demonstrating spinal cord pathology, intervertebral disc herniation, and ligamentous disruption. MRI has limited usefulness as the primary means for initial cervical clearance. The highly sensitive images of MRI show muscular and soft tissue images that do not necessarily correlate with clinical instability. MRI is not necessary if the initial screening CT is negative and the patient does not demonstrate neurologic abnormalities. CT has evolved to be first line modality in obtunded patient in a trauma setting. If the CT is negative, Anderson supports discontinuing the cervical collar. MRI may find abnormalities even if the CT is negative; however, these abnormalities are not likely to be clinically significant. The American College of Radiology advocates both CT and MRI for clearance of the obtunded patient [2,17,18] (Figure 1).
Conclusion
There is a continuing debate about the credibility of these clinical protocols in C-spine without the aid of radiographic assessment. In a neurologically unstable patient, the cervical spine must be immobilized irrespective of the injury. The universally accepted method of C-spine management includes hard collars, block and straps, and manual axial inline stabilization. These management methods are rather emotional and lack adequate scientific basis, especially in conscious patients. However, the generally accepted fact is that the application of collar protects and stabilizes the cervical spine temporarily until definitive management is done. The cervical collar should be applied by an experienced person or a person trained to do that. It should be snugly fitted to aid immobilization and while applying care should be taken not to compress the neck. Improper applications of collars are implicated in airway obstruction and perhaps rise in intracranial pressure by affecting the venous return from the brain. This complicates head injury and increases the cerebrospinal fluid leakage form skull base fractures and creates problems during operative repair of maxillofacial injuries. The gravity of all maxillofacial injuries lies in the fact that they pose an immediate threat to life because of its proximity to both the airway and brain. All the same, each case is unique; thus, the management is exacting even for the most experienced of professionals. In any given scenario, no treatment approach can be sure and flawless. The need of the hour is a multipronged approach requiring a partnership between several departments. While new technology and material developments [19] have helped ease the situation, it is the timely intervention, sheer skill, and presence of mind of emergency personnel, and surgeons that counts.
References
- Jose A, Nagori SA, Agarwal B, Bhutia O, Roychoudhury A (2016) Management of maxillofacial trauma in emergency: An update of challenges and ontroversies. J Emerg Trauma Shock 9(2): 73-80.
- Ambulgekar R, Kothari P, Kandolkar P, Takkar R (2014) Cervical spine Injury clearance protocol in polytrauma patients. IOSR Journal of Dental and Medical Sciences 13(2): 14-16.
- Krausz AA, Krausz MM, Picetti E (2015) Maxillofacial and neck trauma: a damage control approach. World J Emerg Surg 10: 31.
- Nason RW, Assuras GN, Gray PR, Lipschitz J, Burns CM (2001) Penetrating neck injuries: analysis of experience from a Canadian trauma centre. Can J Surg 44(2): 122-126.
- Davidson JS, Birdsell DC (1989) Cervical spine injury in patients with facial skeletal trauma. J Trauma 29(9): 1276-1278.
- Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI (2000) Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med 343(2): 94-99.
- Stiell IG, Wells GA, Vandemheen KL, Clement CM, Lesiuk H, et al. (2001) The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA 286(15): 1841-1848.
- Hanson JA, Blackmore CC, Mann FA, Wilson AJ (2000) Cervical spine injury: a clinical decision rule to identify high-risk patients for helical CT screening. AJR Am J Roentgenol 174(3): 713-717.
- Davis JW, Kaups KL, Cunningham MA, Parks SN, Nowak TP, et al. (2001) Routine evaluation of the cervical spine in head-injured patients with dynamic fluoroscopy: a reappraisal. J Trauma 50(6): 1044-1047.
- Anderson PA, Muchow RD, Munoz A, Tontz WL, Resnick DK (2010) Clearance of the asymptomatic cervical spine: a meta-analysis. J Orthop Trauma 24(2): 100-106.
- Simpson AK, Harris MB (2013) Cervical Spine Clearance. In: Sethi MK, Jahangir AA, Obremskey WT (eds.), Orthopedic Traumatology: An Evidence-Based Approach, Springer publishing, New York, United States, pp. 23-39.
- Holmes JF, Akkinepalli R (2005) Computed tomography versus plain radiography to screen for cervicalspine injury: a metaanalysis. J Trauma 58(5): 902-905.
- Iida H, Tachibana S, Kitahara T, Horiike S, Ohwada T, et al. (1999) Association of head trauma with cervical spine injury,spinal cord injury, or both. J Trauma 46(3): 450-452.
- MacDonald RL, Schwartz ML, Mirich D, Sharkey PW, Nelson WR (1990) Diagnosis of Cervical Soine injuries in motor vehicle crash victims: how many x-rays are enough? J Trauma 30(4): 392-397.
- Buckholtz RW, Heckman JD, Tornetto P, Brown CCM, Ricci WM, et al. (2010) Rockwood and Greens Fractures in Adults. In: Buckholtz RW, Heckman JD, Tornetto P, Brown CCM, Ricci WM, et al. (eds.), Principles of Spine Trauma Care. (7th edn), Lippincott Williams & Wilkins, Philadelphia, Pennsylvania, United States.
- Brown CV, Antevil JL, Sise MJ, Sack DI (2005) Spiral computed tomography for the diagnosis of cervical, thoracic and lumbar spine fractures: Its time has come. J Trauma 58(5): 890-895.
- Thuret S, Moon LD, Gage FH (2006) Therapeutic Interventions after spinal cord injury. Nat Rev Neurosci 7(8): 628-643.
- Hogan GJ, Mirvis SE, Shanmuganathan K, Scalea TM (2005) Exclusion of unstable cervical spine injury in obtunded patients with blunt trauma: Is MRI needed when mutli-detector row CT findings are normal? Radiology 237(1): 106-113.
- Grayzel J, Wiley JF (2017) What’s new in emergency medicine.






























