Epidemiological and Therapeutic Aspects of Obstetric Fistula in The Peri Urban Area of Butembo in the Democratic Republic of Congo
Ndungo KE1*., Matumo P1, Mulisya O2 and Juakali Skv3
Submission: December 06, 2019;Published: December 17, 2019
*Corresponding author: Ndungo KE, Departement of Obstetrics and Gynecology, Université Catholique du Graben/Butembo, Congo
How to cite this article: Ndungo KE, Matumo P, Mulisya O, Juakali Skv.Epidemiological and Therapeutic Aspects of Obstetric Fistula in The Peri Urban 002 Area of Butembo in the Democratic Republic of Congo. J Gynecol Women’s Health. 2019: 17(4): 555968. DOI: 10.19080/JGWH.2019.17.555968
Abstract
Introduction: Obstetric fistula is an abnormal communication, acquired and direct between the genital and urinary tracts and rectal. It usually occurs after an obstruction and laborious delivery. The aim of this presentation is to determine the rate of obstetric fistula, the factors associated with these fistulas in Butembo, to describe the most frequent anatomical lesion, to establish the responsibilities and to assess the cure rate.
Material and methods: A cross-sectional and descriptive study with retrospective data from January 2014 to August 2017. Patients included in this study were admitted and managed in Gynecological ward at the teaching hospital UCG in Butembo. Of the 49 patients with different types of genital fistulas, 37 had obstetric fistula with vesico-vaginal and recto vaginal types and they were all managed.
Results: The cesarean section is the mode of delivery much concerned and accounts for 70.27%, the grand multiparous are 70.27%, the more common anatomical lesion is the vesico-vaginal fistula with 54.05%, The responsibility accounted for midwives is in 51.35% of cases, the type of health facility is the referral health center with 64.86%, the age group concerned is that of 25 to 39 years in 67.59%, the patients who came from rural area in 97.29% and the cure rate after surgery was 83.78%.
Conclusion: Obstetric fistula is frequent in Butembo, occurring in most cases after cesarean section associated with the health workers inexperience. The common anatomical lesion is vesico-vaginal fistula and the cure rate after surgery is encouraging. It is important to consider a proper training of the health workers to improve on the management during labour and delivery in order to prevent these complications
Keywords: Epidemiology Therapeutical aspects Obstetric fistula Peri urban area Butembo
Introduction
Fistulas are abnormal communication acquired between the bladder and the vagina or between the rectum and the vagina and/or between the bladder, the rectum and the vagina. The Obstetric fistula is one of the frightening after-effects of the childbirth dystocia. It is an invalidating disease, humiliating and the despair is there and permanant [1]. The physiopathology of the obstetric fistula concerns difficult delivery which is the result of ischemic necrosis part of the pelvic walls secondary to their prolonged compression by the cephalic presentation of the foetus. The risk of fistula is very high if the pelvic bodies (bladder and rectum) compressed by the presentation are in repletion.
The iatrogenic obstetric fistula, secondary to a Caesarean or ahysterectomy, result from a technical error or insufficiency of competence [1]. The on sequences are the permanent leakage of the urine and/or stool by the vagina. The main causes are however avoidable: the prolonged labour, the insufficient technical support center and unqualified staff. This study aimed to determine the frequency of obstetric fistula and to identify the associated factors in order to contribute to the reduction of the cases of Obstetric fistula in the health centers in peri urban area of Butembo.
Methods
This study was carried out at the Teaching Hospital of the Catholic University of Graben (UCG) at Butembo, in province of North-Kivu, Democratic Republic of Congo (DRC). It is a descriptive cross-sectional study and with retrospective data during the period from January 2014 to August 2017, meaning over 3 yearsand 8 months, period which had 2 outreaches of repair of the fistulas. Our study population was all women who presented leakage of urines and/or faeces from the vagina. Coming from differents villages, 49 cases were admitted including 37 cases of genital leaking which have occurred after the childbirth. Had been included in this study, the patients admitted and operated in the department of gynaecology and obstetrics at the teaching hospital of Graben University in Butembo. Were excluded, all the patients presenting with the similar leakage due to cervical cancer, in posthysterectomy not secondary to the childbirth or simple urinary incontinence due to another problems.
A particular aspect was related on the qualification of medical staff and also to the type of health unit, because the technical support center differs according to whether one is in a referral health center or in a referral hospital. The analysis of our data was done by simple arythmetic average
Results
Frequency of the obstetric fistula
In this study the frequency of obstetric fistula was 37 out of 49 admitted patients (75.51%) compared to other fistula of a gynaecological cause.
Age of the patients
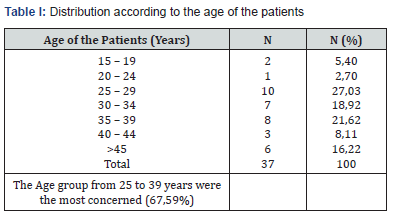
The age group of 45 years and above is about women who were living with fistula for more than 20 years from obstetric cause.
Mode of delivery
Of the 37 deliveries concerned, 26 were carried out by Caesarean section (70,27%)
Parity of the concerned deliveries
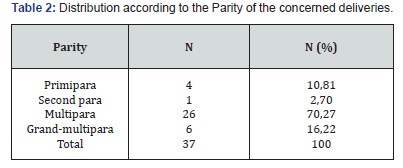
In the table 2, it is shown thats Multipara accounted for 70,27%
Type of anatomic location of the fistula
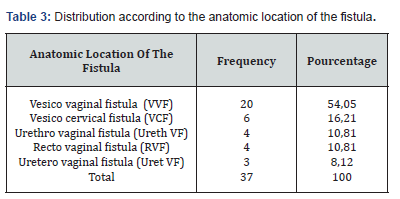
As illustrated in table 3, the VVF represented itself only 54,05% of the obstetric fistula followed by the VCF with 16,21%.
Type of health unit where the delivery was conducted
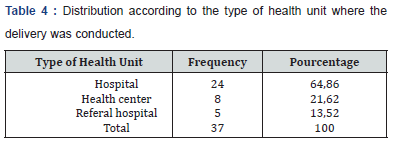
As shown in table 4 Hospitals were the most involved with 64,86 %.
Residence type
The majority of our patients came from rural area with 36 over 37 (97,29%).
Technical responsibility of health workers according to their level of education
The technical responsability of nurses was 51,35% compared with 48,65% of medical officers.
Approach for fistula repair
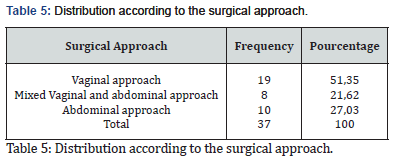
As shown in table 5, The vaginal route was the most used (51,35%)
Outcome of surgical fistula repair
The success rate was 83,78%.
Discussion
Our study shows a high frequency of obstetric fistula (75,51%) compared to other gynaecological fistula.
It is obvious that there is much more deliveries than gynaecological pathologies being able to lead to other types of fistula. Manga O, et al. [2] in Maniema, found a frequency of 66.6% the same as GARTHWAIT Mr. with HARRIS NR., in India 2010; while for Komanda et al. [9] in Kisangani had 85.91%. As shown in Table I, the age of predilection varies from 25 to 39 years is 67,59% with ranges between 19 - 67 years, while for MANGA and other authors this age is very variable with ranges between 13 - 76years [2,4-18]. Sjøveian, Solbjørg, et al. [19] found 55,1% for the age group 20-34 years.
The multiparas account for 70,27% in our study, due to an erroneous certainty to deliver vaginally or by lack of a good monitoring by the medical staff. This is similar to the results with Sjøveian, Solbjørg, et al. [19] who found 43,2% for multiparas while primiparas represented only 10,81%. NR. IDI et al. [4] in Niger, also found that the multiparas represented the 25% [4] and for GUEYE in Senegal the multiparas accounted for 53% compared with primiparas 46% [11,15]. On the other hand, J. BULAMBA N. et al in Haut Kantanga found 42.6% [16] of primiparas, for OUATTARA et al in Mali, he found that primiparous women represent 76.8 %% [5]. For JOKHIO A H et al in 2006 in Pakistan the primiparas represent 39.4%.
The anatomic classification is 48.48% for the VVF and 18.18% for the VCF. These founding are probably due to surgical technical errors among mothers probably in fully dilation with a foetal head deeply engaged and obstructed for a long time. Ofcourse the mode of delivery was by Caesarean section which is one of the big risk factors with 70,27%. In our study, it arises that the referal health centres converted nowadays into Hospitals account for 64,86% of the health facilities which employ medical officers who often do not have great experience and sometimes of insufficient number leading to authorize some nurses to practise the Caesarean section at all risk. On the other hand, OUATTARA et al. Found 6.7% of case of Caesarean section and 65.6% of case of obstetric fistula occurred in the health centres in the presence of a nursing staff only [5]. A similar situation with ours, without specifying the qualification of staff nor the kind of health facility, was already observed by most authors. Bouya Pa et al. [15] in Juba in the South Sudan, found 41% obstetric fistula following caesarean section.
Ahaduworkineh et al. [13] in Ethiopia 2016, found 24.4% following a Caesarean section and 22% following a hysterectomy done because of ruptured uterus. Other authors found that the majority of the cases of obstetric fistula is found among women having been delivered from home [3,5,6]. Onsrud M, et al. [17] found at Panzi Hospital in Bukavu DRC 40% of obstetric fistula in post caesrean section. The level of education of health workers reveals that the nurses have the technical responsibility of 51,35% and the medical officers with 48,65%, certainly with insufficienttechnical skills. The insufficient number of Doctors in remote rural area, makes that nurses replace the doctor in the event of emergency, without any confidence about their skills. The technical support should be adressed, because a referral health centre is less equipped than a referral hospital.
The repair of the fistula was done mostly by vaginal route, according to the type of the lesion (51, 35%) followed by the abdominal route (27,03%). For IDI et al. [4] repair is done by vaginal route in 91.4%. Both routes are also considered according to the type of lesion [12] In this study the success rate was of 83,78% and the failures were especially related to the number of previous repairs, like with the complexity of certain lesions. For other authors the success rate range between 68.7% and 93.4% [7-11,13,14,16].
Conclusion
The obstetric fistula is frequent in the peri-urban area of Butembo and constitutes the most unpleasant morbidity of the postpartum. It still remains a serious problem of the reproduction health. However it is avoidable if the health workers in the reproductive health became aware of the principles to prevent obstetric fistula. Indeed, it is enough to detect the risk factors during the prenatal care and to take care of the partogram during labor. Lastly, the anatomy of a pregnant uterus and the knowledge of the surgical skills of the Caesarean section must constitute a prerequisite for any doctor not experienced.
Conflicts of Interest
The authors declare that they have no conflicts of interest related to this article.
Acknowledgement
I would also in a special way, like to thank the Université Catholique du Graben fundation for their financial and moral support. The data used to support the findings of this study are available from the corresponding author upon request.
References
- World healthorganization (2009) Fistule obstétricale, principes directeurs pour la prise en charge clinique et le développement de programme/ éditeurs: Gwyneth Lewis, Luc de Bernis.
- Manga O,Tshibangu X, Aimé M (2015) Ampleur de la fistule obstétricale dans la province du Maniema (mini campagne 2014). Kisangani médical 6(2).
- Komanda L, Lupay A, Maindo AMA, Okenge L (2015) Fistules urogénitales: étude épidémiologique et Clinique dans deux hopitaux généraux du district de la Tshopo, Kisangani - RDC. Kisangani médical 6(2).
- Idi N, Gabra M, Nayama M, Ganda S, AmoulKinni G, et al. (2010) Fistules vésico-vaginales d’origine obstétricale. Etude prospective à propos de 111 cas à l’hôpital national de NIAMEY. Journal de la SAGO 11(1).
- Ouattara K, Traore ML, Cissé C (1991) Quelques aspects des fistules vésico-vaginales en République du Mali, à propos de 134 cas. Médecine de l’Afrique Noire 38(12): 856-860.
- Anoukoum T, Attipou A, Akpadza K, Ayite EA, Agoda-Koussema LK, et al. (2010) Aspects épidémiologiques, étiologiques et thérapeutiques de la fistule obstétricale au Togo. Progrès en urologie 20(1): 71-76.
- Moudouni S, Nouri M, Koutani A, IbnAttya A, Hachimi M, et al. (2001) Les fistules vésico-vaginales obstétricales. A propos de 114 cas, Progrès en urologie, Maghreb 11: 103-108.
- Camey M (1998) Les fistules obstétricales, Progrès en Urologie 7, Bd, Flandrin- 75116 Paris, 4e trimestre.
- Manga O, Aime M, Tshibangu X (2015) Les statistiques des réparations des fistules dans un pays en conflits armés récurrents: cas de la province du Maniema en RDC. Kisangani médical 6(2).
- 10. Léon Mubikayi, Tozin Rahma (2015) Place de la fibrose dans la guérison de la fistule vésico-vaginale obstétricale. Kisangani médicalseptembre 6(2).
- Gueye SM, Diagne BA, Mensah A (1992) Les fistules vésico-vaginales : Aspects étiopathogéniques et thérapeutiques au Sénégal. Médecine d’Afrique Noire 39(8/9).
- Santosh K, Nitin SK, Gopalakrishnan G (2007) Vesicovaginal fistula: an update. Indian J urol 23(2): 187-191.
- Sori DA, Azale AW, Gemeda DH (2016) Characteristics repair outcome of patients with vesicovaginal fistula managed in Jimma University teaching Hospital. Ethiopia. BMC urol 16(1): 41.
- Garthwaite M, Harris N (2010) Vesicovaginal fistula: our experience of 47 cases in a tertiary care hospital of west Bengal. Indian J urol.
- Bouya PA, Nganongo WI, Lomin D, Iloki LH (2012) Retrospective study of 34 urogenital fistulas of obstetrical origin, gynecol, obstet, fertil. South Sudan.
- Bulamba JN, Mukuku O, Foma JDY, Kinenkinda X, Kakundji P, et al. (2018) Les fistules obstétricales dans la province du Haut Kantanga en Republique Démocratique du Congo, à propos de 242 cas. Pan Afr Med J 29: 34.
- Onsrud M, Sjoveian S, Mukwege D (2011) Cesarean delivery-related fistulae in the Democratic Republic of Congo. Int J Gynaecol Obstet 114(1): 10-14.
- Jokhio AH, Kelly J (2006) Obstetric fistulas in rural Pakistan. Int J Gynaecol Obstet 95(3): 288-289.
- Sjøveian S, Vangen S, Mukwege D, Onsrud M (2011) Surgical outcome of obstetric fistula: a retrospective analysis of 595 patients. Acta obstetricia et gynecologica Scandinavica 90(7): 753-760.






























