- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Treatment of Postmenopausal Osteoporosis
Rashmi Singla*
Department of pharmacology, Govt Doon medical college, India
Submission:November 19, 2018 ; Published: November 29, 2018 ;
*Corresponding author: Rashmi Singla, Department of pharmacology, Govt Doon medical college, India.
How to cite this article: Rashmi Singla. Treatment of Postmenopausal Osteoporosis. J Gynecol Women’s Health. 2018: 13(2): 555859. DOI: 10.19080/JGWH.2018.13.555859
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Abstract
Osteoporosis occurs when bones loose their strength and density. Bones become fragile, weak and brittle and can cause fracture easily. Osteoporosis affects women after menopause and in their later years. The drop in estrogen after menopause is associated with increased loss of bone density for few years. Osteoporosis prevalent among older postmenopausal women increases the risk of fractures. Hip and spine fractures are associated with high morbidity and mortality among this population. Bone loss can be detected by measuring bone mineral density by densitometry. The primary goal of treatment of osteoporosis is to prevent a fracture which is accomplished by slowing /stopping bone loss, maintaining bone strength and minimizing that may contribute to fractures. This is done by change in lifestyle and diet and by giving pharmacological therapy.
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Introduction
According to WHO, Osteoporosis is now widely recognized as a progressive systemic disease characterized by low bone mineral density and micro architectural deterioration in the brain that predisposes the patients to increased bone fragility.
Osteoporosis is most common in women after menopause [1]. Postmenopausal osteoporosis occurs when the rate of bone loss exceeds the rate of bone formation. Menopause typically occurs in women in the midlife during their 40s and 50sand signals the end of fertile phase of a woman’s life cycle. The transition from reproductive to non-reproductive phase is the result of a minor reduction in female hormone production by the ovaries. This transition occurs over a period of years and is a natural consequence of aging. The changes occurring during the transition can disrupt their daily activities. There are 1.5 million osteoporotic fractures every year, with an annual direct cost of treatment of $18 billion. Fractures occur because of qualitative and quantitative deterioration in the vascular and cortical skeleton. In other words, the body is breaking down bone as it normally does but it is not producing new bone. As a result, bones become fragile and weak. It is harder to heal after a fracture when one has osteoporosis, presenting a double threat for people with this condition [2-4]. The menopausal transition is associated with bone loss that exceeds 4% year and extends for 10 years or more .There is individual variation to the rate and extent of bone loss.
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Etiology
Women develop postmenopausal osteoporosis because estrogen rates declines after menopause. A lack of estrogen in postmenopausal women prevents the absorption and utilization of calcium and is the single most important factor in the development of osteoporosis in older women. As women grow older, they can lose significantly, their bone mass which results in osteoporosis. It may be identified during routine medical check up or in the wake of fractures which do not heal properly. Osteoporosis can affect almost the entire skeleton. The disease often does not become clinically apparent until a fracture occurs [5].
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
The Risk Factors
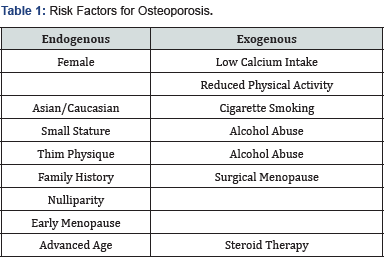
The risk factors for osteoporosis are advancing age, low body weight, maternal history of osteoporosis, the direction of a fall and the most important, the presence of risk fractures- fracture wrist, spine, proximal femur or humerus after mild/moderate trauma and those with osteopenia or spinal deformities [6] (Table 1).
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Physiology of Estrogen
Estrogens are naturally occuring steroidal hormones produced by the ovary, adrenal gland and during pregnancy by the placenta. The major estrogen produced by these organs is estradiol which they synthesise from cholesterol. Estradiol is metabolized in the liver and form estriol and estrone, both of which are mildly estrogenic and are excreted in the urine. Estrogens are most implicated in the reproductive organs but also act upon other organ systems such as CVS, Skeletal, Immune, GIT, neural sites. Their major actions are genomic, mediated by nuclear organ receptors but they may also have non- genomic actions [7].
Two estrogen receptor molecules have been identified. The original estrogen receptor & the estrogen receptor beta. Their structures are similar to those of other members of this family of receptors. The key components are the C or DNA binding domain, which binds with ligand binding affinity & sequence to DNA sequences in the promoter region of target organ, which binds estrogens & estrogen analogues.
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Pathophysiology of Osteoporosis
The combined deficiency of calcitonin and estrogen has been accorded pathogenetic significance. The circulating levels of calcitonin tend to be lower in postmenopausal women. This hormone directly inhibits osteoclast activity &hence bone resorption. The local mediators include PGE2 formed by the osteoblasts, can either increase bone resorption or bone formation .Several osteoclast activating factors such as IL-1 & transforming growth factors produced locally by the macrophages and lymphocytes may contribute to regional bone resorption.
The resorption usually begins at the corticoendosteal surface, resulting in enlargement of the medullary cavity and thinning of cortex. Cancellous bone is also affected. The trabecular plates may be converted to slender strands, sometimes it can result in complete resorption or resection. Because the vertebrae have thin cortex normally and depend on their structural integrity on trabeculae, they are particularly often referred to as vertebral crush fracture syndrome. The increased bone resorption is reflected in an increased number of bizarre osteoclasts [8].
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Clinical Manifestations
Postmenopausal bone loss progresses until the skeletal fragility leads to pain in the back, spine such as lumbar lardosis or kyphoscoliosis related to vertebral collapse. Overt fractures most often are of distal radius, femoral neck and vertebral bodies. Fractures in these three sites have a combined prevalence of 40 % in women >65 years. These fractures result in 40, 00-50, 00 deaths annually [9].
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Diagnostic Evaluation
Bone quality can not be measured clinically, but bone mineral density can be measured quickly and accurately. Bone mineral density should be measured in women with strong risk factors for osteoporosis. It should also be measured in those with osteoporosis related fractures. Several techniques are available for the measurement of bone mineral density. Among them the most useful is dual energy X ray absorptiometry. With this technique the density of the proximal femur is the most useful for predicting fractures. The measurement of lumbar or spine density is most useful for maintenance therapy. A T score of lower than -2.5 especially in the presence of risk factors, indicates the need for treatment to prevent fractures. T score of less than -1 or a Z score of less than -1 at the lumbar spine/proximal femur within five years after menopause at any age indicates the need to prevent bone loss. A z score of less than -2 indicates accelerated bone loss and needs further studies to identify the risk factor [2,4,7].
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Management Strategies
It is important to screen the patients at risk and detect early bone loss in accordance with WHO standards. Postmenopusal women with established fractures should undergo an evaluation for osteoporosis that includes a comprehensive medical and family history and physical examination including vital signs and assessment of routine lab testing should be done. It should include C.B.C, serum calcium, phosphate, liver enzymes, total alkaline phosphates, creatinine & electrolyte levels, thyroid functioning testing and urinalysis [2,3].
Treatment focuses on non -pharmacological measures such as balanced diet, adequate calcium and vitamin D intake, adequate exercise, smoking cessation, avoidance of excess alcohol intake and fall prevention. If pharmacological therapy is indicated, govt. approved options are calcitonin, biphosphonates, glucosamine, SERMS, Reclast, Teripatratide, transdermal estrogens and hormone replacement therapy [10,11].
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Calcium
Calcium is most essential to bone health. The controlled clinical trials examining the effect of calcium on bone density and fractures in postmenopausal women, 15 trials (1806) patients were included that randomized post menopausal women to calcium supplementation and recorded bone mineral density of the total body. The results showed that calcium supplementation alone has small effect on bone density but there as reduction in vertebral fractures. Calcium supplementation mostly increases mineral density of non weight bearing, cortical bone. Calcium salts are available in form of calcium carbonate, calcium citrate, calcium maleate, calcium gluconate, calcium hydroxide, calcium lactate, calcium sulfate, calcium pyrophosphate, calcium oxalate, calcium pantothenate salts. Calcium carbonate is absorbed more efficiently when taken with meals because it needs acid produced by the body when food is in the intestine. In contrast ,calcium citrate can be taken with or without food. Vitamin D increases body’s efficiency at absorbing calcium. The best source of this vitamin is from sunlight. Many dietary modifications can help body absorb calcium more easily. A sodium and protein intake impairs calcium absorption, while added potassium helps with the absorption. Caffeine and alcohol can decrease the body’s ability to absorb calcium. The national institute of health adds that a diet high in fruit and vegetables shifts the acid base balance in the body, decreasing calcium absorption. The recommended dose of 1500mg of calcium and 400-800 IU of vitamin D daily can stop bone loss for some postmenopausal women [12].
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Vitamin D
Calcitriol enhances absorption of calcium and phosphate from intestine. The metaanalysis of these 5 studies suggested a potentially important reduction in vertebral fractures with the intake of vitamin D. Factors that can affect vitamin D intake include decreased exposure to sunlight, decreased dietary intake and absorption problems. The body’s use of vitamin D is enhanced in the presence of Mg and boron. Alfacalcidiol is orally active used in the dose of 1-2 microgms/day. It can increase bone mineral density and reduce fracture incidence in the elderly population. Cholecalciferol (vitamin D3) is used as granules for oral ingestion and oily solution for I.M injection. Calcitriol 0.25 -1 microgms is given orally daily or on alternate days [13].
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Magnesium
The other vital nutrients synergistically promote the maintenance of healthy bone tissue. For instances mega doses of calcium in absence of other minerals such as magnesium may contribute to abnormal soft tissue calcification. Oral supplements with as much magnesium as calcium helps to prevent bone loss. Mg increases the remineralisation of weight bearing trabecular bone in post menopausal osteoporotic women. The daily dose of magnesium is 200-300mg [13].
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Zinc
This vital trace element is essential for normal bone formation. It is involved in the biochemical activities of vitamin D. The daily requirement is 2-4mg [13].
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Boron
Small amounts of this trace element can enhance absorption of calcium. The daily requirement is 2mg [13, 14].
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Manganese
This trace element is essential for the mineralization of the bone as well as the production of cartilage and connective tissues. The best source of Mn in the diet is from grains [13].
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Calcitonin
It is produced by C cells of the thyroid. It inhibits bone resorption by direct action on osteoclasts. 30 studies were done in post menopausal women on calcitonin treatment .Calcitonin is shown to reduce the risk of vertebral fractures but the effect on hip fracture appears to be less than that of biphosphonate therapy .It is used in post menopausal osteoporosis as 100Usc or IM daily along with calcium and vitamin D supplements. A nasal spray formulation delivering 200 IU per actuation has become available in some countries [15-17].
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Biphosphonates
Etridronate, Alendronate, risedronate inhibit bone resorption. Alendronate is administered empty stomach in the morning with a full glass of water and patient is instructed not to lie down or take food for at least 30min. It is available as 35 and 70mg tablets. Recent data support the use of alendronate 10mg daily in the treatment of steroid induced osteoporosis. The dose of 5mg daily has been shown to prevent accelerated bone loss in newly postmenopausal omen & may be useful for omen who are unable to take estrogen sensitive cancers or clotting disorders.
Calcium, iron, antacids, mineral water, tea, coffee, fruit juice interfere with Alendronate absorption. Side effects are git. Irritation, gastric erosion, flatulence, body ache. Etidronate is administered as orally or as intravenous. Adverse effects are gastric irritation, bone pain. The dose is 5- 7.5mg/kg /day [18].
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Reclast (Zoledronic Acid)
The randomized phase 11 trial is studying how well alendronic acid works in preventing osteoporosis in patients undergoing donor stem cell transplant. Reclast is specifically prescribed for treatment of osteoporosis in postmenopausal women. It is a bisphosphonic acid inhibitor of osteoclastic bone resorption. Once administered, it rapidly moves to bone and preferentially localizes at sites of high bone turnover. Reclast is supplied as 5mg in a 100ml ready to infuse solution for intravenous administration. The recommended initial dose of the drug is a 5mg infusion once a year given intravenously over no less than 15 minutes. Adverse effects associated with the use of Reclast may include arthralgia, pyrexia, hypertension, headache, myalgia, and pain in extremity, influenza like illness & nausea [19,20].
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Strontium Ralenate (Proteolos)
It is also used for the treatment of osteoporosis in postmenopausal women. It is usually reserved for women who cannot take biphosphonates. In the dose of 2gms, it has dual action of increasing bone formation as well as decreasing bone breakdown and it has been shown to decrease the risk of hip and spine fractures. Strontium seems to be associated with an increased risk of blood clots in the veins [21].
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Glucosamine
The most advanced dietary supplements for the management of bone and joint health include chondro- protective agents such as high quality glucosamine that may decrease the inflammation. A double blind clinical study states that glucosamine supplements may increase the cartilage and fluid that surrounds the joints or helps prevent breakdown of these substances .Glucosamine is a nutrient supplement that serves the purpose of cartilage building or lubrication of joints. Glucosamine helps the efficient working of joints and tissues. Glucosamine sulfate also plays a crucial role in the repair, maintenance and replacement of worn out or damaged tissues. It is an important constituent of body cartilage, soft tissue that protects the joint. Glucosamine sulfate greatly helps in relieving the osteoporosis pain in knee joints .It is suitable and effective treatment for mild levels of arthritis as well as osteoporosis. The recommended dose of glucosamine sulfate is 100mg in 1-2 capsules during the day at meal times with food. Side effects of glucosamine are very few [22].
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Serms
Selective estrogen receptor modulators like raloxifene and tamoxifen have been marketed. Tamoxifen causes improvement in bone mass due to antiresorptive effect. Tamoxifen is effective orally. The dose is 10-20mg BD. Raloxifene is an estrogen partial agonist in bone and CVS system. Raloxifene prevents bone loss in post menopausal women. Raloxifene is absorbed orally but has low bioavailability due to extensive first pass metabolism. Its side effects are deep vein thrombosis and pulmonary embolism. The dose is 60 mg /day. It is preferably used in women who are 5 years past their menopause [23].
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Transdermal Estradiol Patches
In a clinical trial using transdermal delivery-0.1mg of 17- beta -estradiol for days 1-21 and oral dose on day 11-21 of a 28 days cycle. Transdermal estradiol treatment is effective in postmenopausal women with established osteoporosis in only who had hysterectomy as the side effects of estrogen affect the other women with uterus [24].
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Teriparatide
Teriparatide is used for the treatment of osteoporosis in post menopausal women with an increased risk of fractures. It works by decreasing the formation of bone and is given by daily injection under the skin in the abdomen or thigh. The recommended dose of teriparatide is 20mg injected OD. It is good to take teriparatide at the same time each day. It decreases incidence of spinal fractures [25].
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
HRT
Hormone replacement therapy remains a valuable option for the prevention of osteoporosis in elderly post -menopausal women. The choice of treatment depends on age, the presence/ absence of prevalent fractures, esp. at the spine and the degree of bone mass density measured at spine and hip. The study of osteoporotic fractures provided epidemiological data that bone loss continues in older women & that estrogen may decrease this loss. Hormone replacement therapy is available as conjugated equine estrogens in the dose of 0.625mg /day regularly or in cyclic fashion. plus medroxyprogesterone acetate 2.5mg/day or estrogen therapy. A 2002 study from Wake Forest University School of Medicine indicates that stopping HRT does not appear to accelerate loss of bone in post menopausal women. The study also showed that while bone mass increased substantially in the first 36 months after starting HRT. There was little gain in bone mass after that. Among women who remain on HRT for upto 5 more years, it appears that bone mass remains stable at the same level as 3 year treatment. But potential risks associated with HRT included are an increased risk of venous thrombosis, an exacerbation of preexisting liver disease for women with intact uterus taking estrogen alone and an increased risk of endometrial carcinoma. Serious side effects of hormone replacement therapy include enlarged and tender breasts, nausea, skin discolouration, water retention, weight gain, headache and digestive problems [26-28].
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Life Style Changes
Exercise greatly reduces the risk of heart disease, high B.P and diabetes. It has positive effects on mental well being also. The sort of exercise that is beneficial in preventing osteoporosis is weight bearing such as walking or aerobics. Stopping smoking should be a priority to enjoy a longer life. Alcohol consumption should also be kept in safe limits.
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
Conclusion
Osteoporosis represents an increasingly serious problem around the world. The economic burden of disease imposes is already considerable and will further grow as the population ages. It incorporates multiple modalities of therapy. In addition to early detection, patient education, exercise and nutritional supplementation, multiple therapeutic agents should be implemented early in an attempt to prevent initial and subsequent fractures.
Results of large placebo controlled trials have shown that alendronate, raloxifene, risedronate, 1-34 fragment of parathyroid hormone and nasal calcitonin greatly reduced the risk of vertebral fractures. Calcium along with vitamin D is most important for increasing bone strength and vitamin supplementation is not sufficient to treat individuals with osteoporosis but is useful sp. in elderly women in care homes. Hormone replacement therapy remains a valuable option for the prevention of osteoporosis in post menopausal women. Choice of treatment depends on age, the presence or absence of prevalent fractures, esp. at the spine and the degree of bone mineral density measured at spine and hip. Non-pharmacological intervention include adequate calcium intake and diet, selected exercise programmes, reduction of other risk factors for osteoporotic fractures. The overall benefit versus risk assessment is a central focus in each of the clinical trial outcomes.
- Mini Review
- Abstract
- Introduction
- Etiology
- The Risk Factors
- Physiology of Estrogen
- Pathophysiology of Osteoporosis
- Clinical Manifestations
- Diagnostic Evaluation
- Management Strategies
- Calcium
- Vitamin D
- Magnesium
- Zinc
- Boron
- Manganese
- Calcitonin
- Biphosphonates
- Reclast (Zoledronic Acid)
- Strontium Ralenate (Proteolos)
- Glucosamine
- Serms
- Transdermal Estradiol Patches
- Teriparatide
- HRT
- Life Style Changes
- Conclusion
- References
References
- Kamis JA, Melton LJ, Christian C, Johnston CC, Khaltaev N, eat al. (1994) The diagnosis of osteoporosis. J Bone Miner Res 9(8): 1137-1141.
- Rosen CJ (2005) Post menopausal osteoporosis. N Eng J Med 353: 595- 603.
- Kamal HK (2006) Postmenopausal osteoporosis; etiology, current diagnostic strategies, and nonprescription interventions. J Manang Care Pharm 12(6SupplA): 34-39.
- Aloia JF, Cohn SH, Vaswani A, Yeh JK, Yuen K, et al. (1985) The Risk factors in postmenopausal osteoporosis. Am J Med 78(1): 95-100.
- Richard Eastell (1998) Treatment of postmenopausal osteoporosis. N Eng J Med 338: 735-746.
- Jeni Warden (2010) Management of osteoporosis in postmenopausal women: 2010 position statement of The North American Menopause Society. Menopause 17(1): 25-54.
- Shaw gynecology
- Robbins pathology
- Davidson
- Cranny A (2003) Treatment of postmenopausal osteoporosis. BMJ, p. 327.
- (1994) Postmenopsal osteoporosis prevention. British Medical J, pp. 1268-1269.
- Tilyard BW, George FS, J Thomson (1992) Treatment of post menopausal osteoporosis with calcitriol or calcium. N Eng J Med 326: 357-362.
- Stristsbogtrykkeri (1984) Proceedings of the Copenhagen International Symposium on osteoporosis. pp. 755-761.
- Steven Ehiting (1994) Postmenopausal osteoporosis prevention. British Medical Journal pp. 1268-1269.
- Stristsbogtrykkeri (1984) Proceedings of the Copenhagen International Symposium. pp. 755-761.
- Citrielli R, Gonnelli S, Zacchei F, Bigazzi S, Vattimo A, et al. (1988) Bone turnover in postmenopausal osteoporosis. Effect of calcitonin treatment, J Clin Invest 82(4): 1268-1274.
- Rack PJ, Sebba A (2005) Optimizing administration of bisphosphonates in women with postmenopausal osteoporosis. Treat Endocrinol 4(4): 245-251.
- Devogelaer JP, Brown JP, Burckhardt P, Meunier PJ, Goemaere S, et al. (2007) Zoledronic acid efficacy and safety over five years in postmenopausal osteoporosis. Osteoporos Int 18(9): 1211-1218
- Black DM, Delmas PD, Eastell R, Reid IR, Boonen S, et al. (2007) Pivotal Fracture Trial Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. The New England Journal of Medicine.
- Peter FU, Bologonese SMA (2010) Life style changes for preventing postmenopausal osteoporosis. Rev Endocr Metab Disord 11(4): 253- 259.
- Luficin EG, Wahner, Fallon MW, Hodgson SF, Kotowicz MA, et al. (1992) Treatment of post menopausal osteoporosis with transdermal estrogen. Ann Intern Med 117(1): 1-9.
- Belchetz PE (1994) Hormonal treatment of post menopausal women. N Engl J Med 330(15): 1062-1071.
- (2003) HRT update on the risk of breast cancer and long term safety, current problems in pharmacovigilance. Vol 29.
- Hormone TN (2003) Management of osteoporosis, Scottish intercollegiate guidelines Network. replacement therapy risks and benefits.
- Peter F Ullrch, Lifestyle changes for preventing postmenopausal osteoporosis.
- Pharmaceutical Journal (2003) Osteoporosis treatment and prevention of fragility fractures, Prodify Guidance. 271: 646-648.
- (2010) Management of osteoporosis in postmenopausal women. Menopause 17(1): 25-54.
- Delmas PD (2002) Treatment of postmenopausal osteoporosis. Lancet 359(9322): 2018-2026.






























