Assessment and Diagnosis of Poisoning with Characteristics Features in Living or Dead
Lalit P Chandravanshi* and Mamta Pal
Division of Forensic Science, Galgotias University, India
Submission: August 20, 2018; Published: September 10, 2018
*Corresponding author: Lalit P Chandravanshi, Assistant Professor, Division of Forensic Science, School of Basic & Applied Sciences, Galgotias University, Greater Noida-201307, India.
How to cite this article: Lalit P C, Mamta P. Assessment and Diagnosis of Poisoning with Characteristics Features in Living or Dead. J Forensic Sci & Criminal Inves 2018; 10(4): 555796. DOI: 10.19080/JFSCI.2018.10.555796.
Abstract
The systematic examination of the poisoning case whether it’s in live case or deceased case is one of the most challenging tasks in forensic toxicology. In the suspected case of poisoning, both external and internal examination of the body is carried out to determine the cause of death. Forensic toxicologist generates the hypothesis based on the associated postmortem appearances and performs the related analytical tests. This review attempts to highlight the points for diagnosis of poisoning on the basis of external and internal clinical signs along with non-clinical findings. In case of lack of data associated with characteristic autopsy appearances is often very frustrating to a forensic toxicologist, therefore case history and autopsy findings are very helpful to screen which test has to perform exclusively first. Interpretation of postmortem toxicological findings is always based on the skills and experiences as well as requires literature for comparison. Case history, circumstantial evidences and autopsy findings become important part of the interpretation too. Moreover, it is advised that differentiate the clinical sign whether caused by either poison or any natural disease. Complete diagnosis of poisoning of is a collaborative investigation between forensic pathologist and toxicologist, however, in this review; information has been assembled on the basis of external and internal finding in live and dead case as well.
Keywords: Autopsy; Toxicology; Toxic syndrome; Perforation Etc
Introduction
Poisoning refers to exposure to any agent which is capable of producing an adverse response in a biological system. It may results into slight irritation, serious deleterious effects and even may cause death. Poisoning is common in the world including India but modes of poisoning varies i.e. it may results from the attempt of suicide, homicide and accidents [1]. High rate of accidental poisonings have been reported in children due to their inquisitiveness, inability to read warning labels, and inadequate supervision. At home, drugs or household chemicals are most likely the main cause of accidental exposure to children and adults [2,3]. Accidently ingestion of contaminated food, poisonous plants or animals and stinging and biting are the other causes of accidental poisoning in adult [4]. While, criminal poisoning occurs when individual or group of individuals intentionally attempts to cause destruction of life on others by using poison [5]. To harm a person criminal prefers to use poison as it provides him ample time to escape from the scene / spot. Homicidal poisoning is the killing of a human being by the administration of poison. Selected poisons are used for homicidal purposes because of their small fatal doses, tasteless and odorless properties, miscibility with drinks and availability, which are considered as ideal homicidal poisons. Financial (inheritance, insurance), personal (revenge) and psychological (a desire for power and control) factors may motivate the homicidal poisoning.
On the other hand’ suicidal poisoning defines as the self-infliction by poison with the intention of committing suicide. Availability of poisons in house or the working place is one of the factor which promote suicidal poisoning like, cyanide in electroplating units, pesticides are mostly available with farming communities, thiopental sodium nitrite in dyeing industries etc. [6]. Suicidal cases are being frequently reported in young people. Besides, barbiturates and benzodiazepines are usually used by the educated people. Anaesthetic agents like thiopental have also been reported in the suicide cases in few doctors [7,8]. On the basis of duration of exposure, sign and symptoms, medical practitioner can categorize the poisoning in fulminate, acute, sub-acute, chronic and sub chronic. Owing to the massive dose, death precedes very rapidly without any onset of symptoms is called a fulminant poisoning. In such poisoning the patient is appeared to collapse suddenly. Acute poisoning is produced either by a single high dose or several small doses taken over a short interval of time i.e. it may be seconds, minutes or hours, or repeated exposures over about a day when less. In acute are , the onset of sign and symptoms are relatively instantaneous and depends upon the dosages [9]. Delayed health effects of acute poisoning also should not be forgotten because sometime toxicity appears late even when people are no longer to the exposure of poison substance for many days, months or years. Therefore, sign and symptoms of chronic exposure varies due to different duration of exposures and how much poison enters in the body and partly on how much poison eliminates from the body during that time. Chronic poisoning is mainly seen in occupationally engaged people at their work places and is caused due to exposure of small doses over a long period of time, resulting in gradual deterioration eg: mercury, arsenic, lead, cadmium, antimony and opium [10-13]. Sub-acute poisoning occurs slowly than acute poisoning but exposure than chronic poisoning.
Methods
A literature search was conducted May to June 2018 in Pub - Med (www.ncbi.nlm.nih.gov/pubmed/), SciFinder (products/ scifnder) and Scopus (www.scopus.com/) databases filtered for poisoning studies. Total of 373 studies with poisoning outcomes was identified, of which seventy six studies were eligible and included in this review.
Diagnosis of Poisoning
Initially, prompt treatment is necessary to prevent complications due to poisoning, but the diagnosis of poisoning may be difficult because of the victim may either be unconscious or poisoned by other persons [14]. The doctors acquire information like history of poisoning and extent of poisoning to generate the hypothesis and likewise perform the laboratory test to detect the presence of particular poison and its level in blood, urine or other visceral tissues depending upon the class of poison. In case of an unconscious victim, tablets, empty containers, and vomited material are useful evidence to determine which substance was accounted for poisoning [15,16]. In order to diagnose the poisoning, physical examination of the patient is necessary; some toxic substances may cause rawness or burning of the skin. In some cases the diagnosis of poisoning is uncomplicated because of their characteristic odor and specific sign of injuries and symptoms caused; like petroleum products leave a lighter fluid or kerosene like distinctive odor and some acids and alkalis leave burns on the mouth [17,18]. Unfortunately, diagnosis in the many poisoning cases remains indecisive.
In the Living
Diagnosis of poisoning in living person is examined based on the clinical or non clinical history with circumstantial evidences and specific or nonspecific signs of poisoned patients.
History and Circumstantial Evidences
Diagnosis of self-poisoning can usually be made from the history. The doctor gathers toxicological, medical, psychiatric and social history for the diagnosis of poisoning. This history can be acquired from friends and relatives also. Suicide note, presence of any suspicious article like; tablets, bottles, vials, ampoule etc. are helpful for the assessment of poisoning in the unconscious poisoned patients or dead persons [19,20]. If the poisoning occurs in the children, poisoned material may be present at around their mouth or on their clothing. The history should consist of the patient’s age, weight, nature or amount of substance taken, time of onset of symptoms of poisoning and typical or atypical route of poisoning [21,22]. Besides, the doctor should obtain the other information like; geographic location where the poisoning occurred and the whether the patient emotionally or psychiatrically distressed. In addition, a detailed of addiction history and past medical history should be obtained, including concurrent medications and previous side effects if any. Specific attention should be required to the collect the essential information and the poisoning associated details to know whether the poisoning is intentional or unintentional.
Clinical Sign
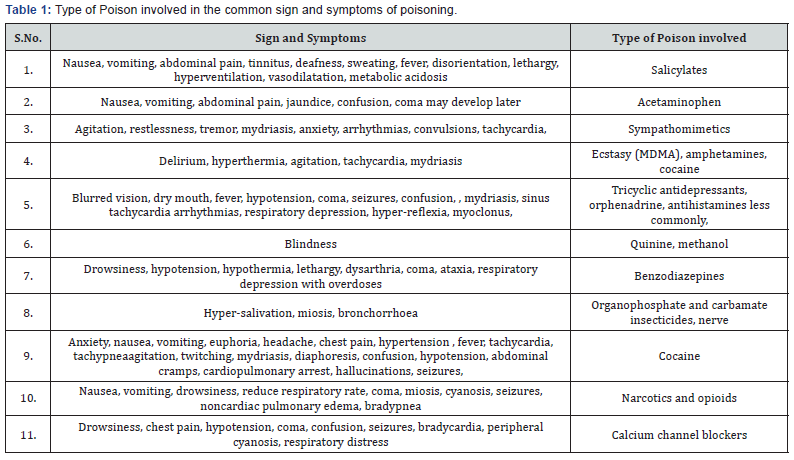
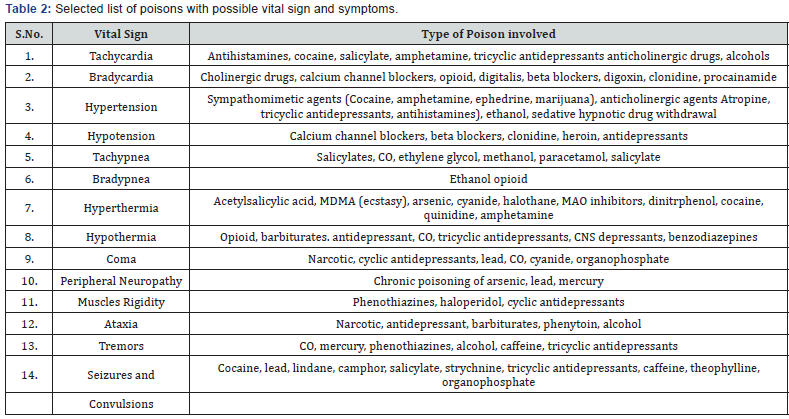
Physical examination of the poisoned person may indicate the poison or category of poison involved in poisoning. However, there is an extensive range of poisons which can cause some common effects on the person that make the diagnosis more difficult in such cases. Constellations of clinical signs of poisoning associated with some common poisons have been described as toxic syndromes and help the clinician for the preliminary identification the cause of poisoning [23,24].The doctor should note abnormalities of each system of the body of the patient including any vital sign in eyes, skin, reflexes, breath sounds, and dehydration due to vomiting/diarrhea and should also observe urine color and any kind of physical material linked with the poisoning. General observations of the poisoned person may also divulge valuable information. Diagnosis of poisoning cannot be possible on the basis of a single sign as there are various signs and symptoms come together that make diagnosis of poisoning possible with specific poisons. However, there are some important valuable specific clues which pertain for specific poison or drug only. -Such specific patterns of toxicity related to the specific poisons have been enlisted in the Table 1.
Vital Sign
Vital signs in the case of poisoning are mostly associated with the overdosed cases, cardiac arrhythmias, respiratory/ cardiovascular depression, and impairment of consciousness, convulsions agitation, and muscular weakness. The rate of respiration may be increased due to direct stimulation of the respiratory center in brain by common stimulant drugs such as caffeine, amphetamines, cocaine [25-27]. Cellular hypoxia may occur due to increase cellular oxygen consumption that associates carbon monoxide poisoning or cyanide poisoning [28,29]. Respiratory arrest may also occur due to the failure of ventilator and depression of the respiratory drive centre with the botulism or organophosphate poisoning [30,31]. Common drugs such as cocaine, phencyclidine and amphetamines may stimulate the central sympathetic nervous system and cause tachycardia and hypertension. Hypotension with bradycardia may develop due to the central depression of sympathetic output, peripheral blockage of calcium channel and J-receptors, by the overdose of tricyclic antidepressants (TCAs), calcium-channel blockers, beta blockers, reported in cyanide or carbon monoxide poisoning. In such cases tachycardia may be caused by hypovolaemia (fluid loss from vomiting and diarrhea) and vasodilatation. Unconsciousness is mostly linked with drug overdose. A variety of drugs such as narcotics, sedatives hypnotics, anticholinergics, or other sympatholytic agents may develop various neurological conditions with the other vital signs (respiratory depression, hyperension and hypotension). Drugs and chemicals can cause coma by various mechanism, including oxygen deprivation, depression of the central nervous system and the cerebral hemorrhage. Like coma, agitation, delirium, psychosis and seizure are common features of poisoning – related to drugs and chemicals. Seizures are associated with the overdose poisoning of tricyclic antidepressants, isoniazid, theophylline and stimulants such as phencyclidine, amphetamine and cocaine [32,33]. Delirium with confusion and disorientation may also occur in anticholinergic poisoning. While, paranoid psychosis associated with the amphetamine or cocaine intoxication [34,35]. Common vital signs of toxicity associated with poisons have been described in the Table 2.
Toxic Syndrome
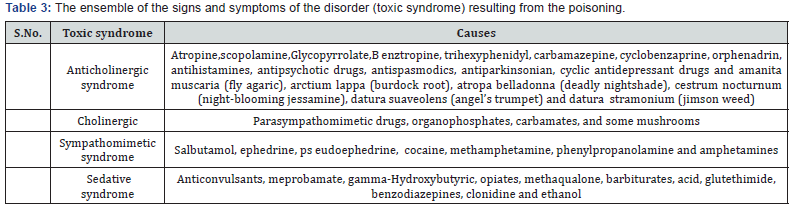
There are few poisoned conditions in which specific signs and symptoms for a particular class of poisons resemble with other clinical conditions arising due to natural disease. Toxic syndrome is described as the constellation of sign and symptoms comprising a set of clinical fingerprints consistently result from the poisons. Toxic syndrome provides a conventional clue for quick detection of suspected causes of poisoning and such toxic syndromes have been summarized in the Table 3.
Cholinergic Syndrome
Cholinergic syndrome is a condition which builds up either from acteylcholinestrase enzyme inhibition or due to direct agonist at muscranic or cholinergic receptors and simultaneously increases the levels of acetylcholine which are potentially lethal for central, peripheral muscranic and cholinergic receptors. Cholinergic syndrome has been noted mostly in organophosphate and carbamates poisoning [36,37]. Sign and symptoms of cholinergic syndrome are erratic but fasciculation and muscles weakness may be more prominent symptoms of cholinergic crisis condition of patient. Further salivation, lacrimation, urinary and faecal incontinence, pinpoint pupils, seizures and respiratory depression have also been observed in organophosphates poisoning. List of causative agents for cholinergic syndrome is shown in Table 3.
Anticholinergic Syndrome
Anticholinergic syndrome arises due to the competitive inhibition of muscranic cholinergic neurotransmission both in the central and peripheral nervous system. Diagnosis of anticholinergic syndrome is clinically based on the symptoms of delirium with signs of peripheral muscranic blockade. Delirium condition appears within few hour of poisoning. It is difficult to evaluate the duration of delirium, but it may persist for up to 5 days in some cases such as poisoning with the benztropine. Anticholinergic toxicity is commonly developed due to the anticholinergic class of drug and other drugs that have anticholinergic properties like antihistamines, antipsychotics, antispasmodics, cyclic antidepressants, and mydriatics [38,39]. In addition to these drugs, several anticholinergic substances are also present in different varieties of plants. Agitated delirium, tremor, myoclonus, delirium (CNS) and hyperthermia with dryness mouth and skin, mydriasis, flushing, urinary retention (PNS) are the clinical features of anticholinergic syndrome [40,41].
Sympathomimetic Syndrome
Drugs of this group include, caffeine, methamphetamines, ritalin, LSD, theophylline, MDMA, cocaine and amphetamines which produce physiologic and toxic effects by Alpha/beta adrenergic stimulation and mimicking the action of sympathetic system [42-44]. Typical adrenergic signs and symptoms are occurred in the sympathomimetic toxic syndrome, some of which can be fatal. However, intracerebral bleeding, seizures, strokes, hyperthermia, hypertension and cardiac arrhythmias are welldocumented complications of sympathomimetic toxicity [45-47] Sometimes this syndrome resembles with the anticholinergic syndrome, but the later is coupled with dry skin and diminished bowel sounds. Sympathomimetic toxic syndrome may also characterize with the some nonlethal signs and symptoms such as mydriasis, acute psychosis, paranoia, bruxism, tachycardia, diaphoresis, and delirium.
Sedative/Hypnotic Syndrome
Sedative-hypnotics are a group of xenobiotics that overcome the excitability and induce drowsiness and results in central nervous system depression. Anticonvulsants benzodiazepines, barbiturates, methaqualone, and ethanol are the most commonly used drugs that may cause such toxic syndrome. Most of the sedative/hypnotic drugs stimulate the activity of the γ-aminobutyric acid (GABA) receptors via the benzodiazepinebinding site or modifications of nerve membranes [48,49]. Deep narcosis may be occurred more likely in this syndrome. Other symptoms of sedative/hypnotic syndrome include blurred vision, slurred speech, ataxia, diplopia, hallucinations, dysesthesias, paresthesias, nystagmus, sedation, respiratory depression especially in barbiturates combination with alcohol and coma.
Ocular Clues
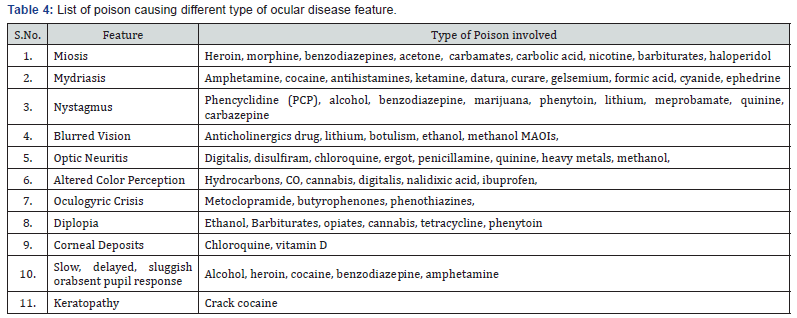
In many cases of poisoning, visual acuity has also found to be affected, even with blindness. Chloroquine, quinine and methanol poisoning is associated with the visual impairment [50-52]. Several drugs/poisons affect the pupils of the eyes and result in miosis, mydriasis and nystagmus. Both mydriasis and miosis can be physiological but may also link with non-physiological causes such as in disease condition, trauma, or intoxication of drugs/poison. Mydriasis is defined as the dilation of the pupil that results in hypersensitity of pupil to light. Mydiasis is caused by the anticholinergic (e.g. tricyclic antidepressants, atropine, cocaine, phenothiazines, benzodiazepines, barbiturates and ethanol) and sympathomimetic (e.g. amfetamines) poison. Some poison (e.g. quinine and methanol) may also cause the blindness mydriasis due to the retinal, optic nerve or ocular dysfunctions. In miosis, there is constriction of pupil that may be caused by opioids, cholinergic or anticholinesterase (e.g. organophosphates, insecticides, phencyclidine, phenothiazines and carbamate pesticides,) poisoning. Nystagmus is another – similar condition which is manifested by uncontrolled, rapid and repetitive eye movements. Nystagmus has also been reported in tobacco, barbiturate, and organophosphate poisoning (Jaanus. 1992). Ocular clues of poisoning and their cause are shown in the Table 4.
Olfactory Clues
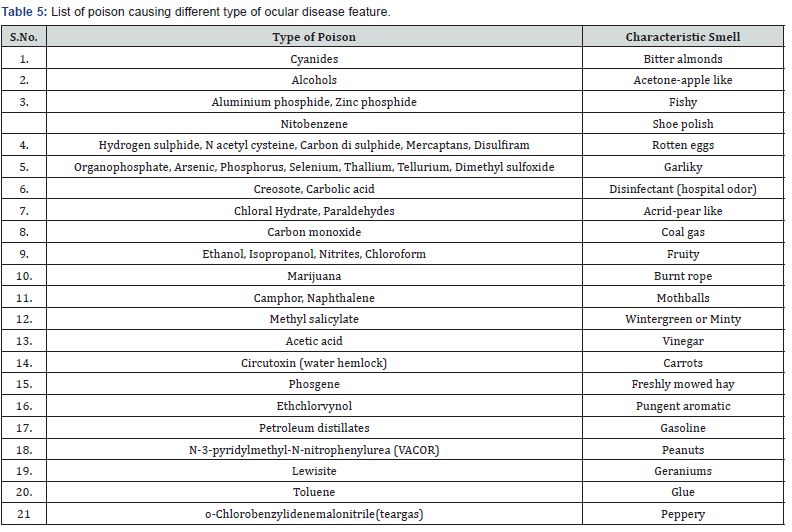
Since, several poisons give off a distinctive odor on the breath which may be perceived in the vicinity of a poisoned patient, therefore, vomit material and smell emanating from the mouth should be inspected for specific poisons. For exsulfur compounds and aluminum phosphide give off mild odor resemble the smell of a lighting match and mild garlic respectively. Owing to poisoning from these poisons, they will give off a powerful odor like rotten eggs and potent garlic odor correspondingly [53]. Petroleum products, such as kerosene, leave a characteristic odor on the breath. One or more types of smell may perceive in certain conditions like organophosphates poisoning. In this, the affected person may smell of garlic due to organophosphates poisoning and of petrol due to the other solvents [54] (Table 5).
Dermal Clues
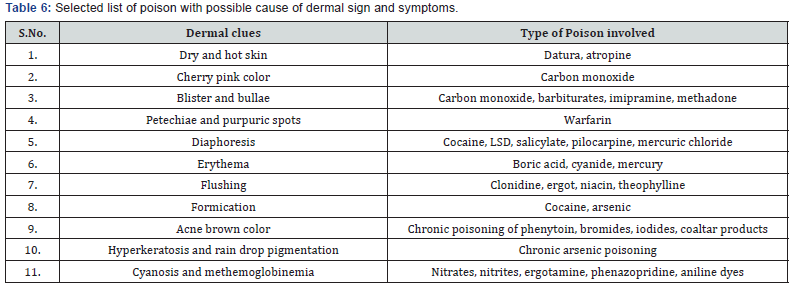
In most of the poisoning cases, dermal clues are appeared either due to direct exposure to skin or due to the systematic effects of poison. Before examining the skin; the patient’s clothing should removed to assess the skin color, temperature, formication, dryness, erytherma, sweating and presence of injection marks. Dermatitis condition may develop due to the chronic exposure of heavy metals. Hyperkeratosis and melanosis are the basic features of chronic poisoning of arsenic [55]. The presence of injection marks on the body may suggest the route of poisoning. In such cases, sample should be collected from the site of injection in order to diagnose the poisoning. Red color appearance of the skin may be due to the carbon monoxide, niacin, cyanide, boric acid and scromboid poisoning. Blue discoloration of the skin (cyanosis or methemoglobinemia) indicates the poisoning caused by the nitrates, nitrites, phenazopridine and ergotamine. The presence of a rashes or blisters may also provide clues for diagnosis. Although rashes or blisters are typically located on different part of the body like between fingers, knee and back as a result of prolonged immobility. These are classically associated with the barbiturate poisoning [56]. Patches may also be seen in vagina and scrotum in case of drug abuse of opioids and fentanyl. The dryness and moisture of skin are also important factor to differentiate an anticholinergicmediated poisoning from a sympathomimetic poisoning as dry and hot skin is associated with the anticholinergic drugs. Dry and hot skin may also be seen in food poisoning. Hyperthermia may also results in drug overdose cases and is an immediate threat to life which must be quickly recognized and treated. Hyperthermia may also be caused by impaired thermoregulatory mechanisms with inadequate heat dissipation, muscular hyperactivity or hyperrigidity and increased metabolic rate [57]. Hyperthermia in case of tricyclic antidepressant overdose results from seizures and myoclonic jerking and is an immediate danger to life. Presence of cool, clammy and sweaty skin is an indicator of hypothermia, suggesting sympathomimetic overdose. A number of drugs produce irritation, dermatitis even in therapeutic nontoxic doses, which include most of the phenothiazines, antibiotics, thiazides, sulfonamides and NSAIDs etc. Hence, dermal signs are very crucial findings that can make the diagnosis of poisoning possible with specific poison or drugs.
Inspection of Blood and Urine
Variations in the color of blood and urine from the normal are found in many intoxication conditions. Some chemical or drugs such as isobutyl nitrite or dapsone may also turn the normal color of blood into chocolate-colored blood due to the development of methaemoglobinaemia condition. Pink plasma indicates the poisoning from the haemolytic poisons (e.g. sodium chlorate). Colored urine may also be seen in various poisoning cases. Yellow or brown discoloration of urine may be caused by the chloroquinine, quinine and cresol poisoning. While, presence of green fluorescence in urine indicates acriflavine poisoning. Besides, blue or green color of the urine is caused by phenol poisoning. Crystals may also be found in urine after ingestion of ethylene glycol or due to an overdose of primidone.
Diagnosis in Dead
Investigation of poisoning in deceased person is based on the different conditions which cover case history, condition under which death caused and postmortem examination of body. Postmortem is carried out to establish the cause of death by analyzing postmortem remains. Sometime clinical diagnosis of poisoning are very complicated because presence of no specific sign and symptoms may indicate the natural death. Unavailability of case history also makes difficult to investigate the case of poisoning.
External
External postmortem finding are also very useful to explore the poisoning case and great attention should be required for external post-mortem examination. Complete external and internal examination of body indicates that which tissues are much required for chemical examination to confirm the suspected cause of death.
Clothes
Clothes should be examined carefully for the presence of any stain of poison, content of vomit and feces.
Facial Features and Natural Orifices (Lips, Mouth, Nose, Ear and Vagina)
If poisoning is suspected; photograph should be taken for analysis of facial features. Color of the face is noted with sign of poisoning. Ulceration and dark brown stains may be seen on lips and near the angle of mouth which is suggestive of corrosive’s poisoning. Careful examination of both upper and lower lids of eyes is carried out and also looks for petechial hemorrhages of conjunctiva. Vitreous fluid under ophthalmoscope should be examined and degree of turbidity of vitreous fluid is noted. The level of turbidity of the vitreous fluid is evident of postmortem gap and drug-induced deaths. The natural orifices such as the mouth, nostril, ear, rectum, and vagina may give an idea about the presence of poisonous material or the signs of it having been used. Hydrocyanic acid or opium gives off a peculiar smell near the mouth and nose. Ulceration may be found in the nasal mucosa of septum in case of cocaine sniffers. Some poisons which may be recognized by their odor are phenol, ether, opium, alcohol, organophosphorus compounds, cyanides, endrin, chloroform, paraldehyde, camphor etc. Furthermore, froth may be present at the mouth and nose in case of opium poisoning. Some organophosphorus compounds produce blood tinged froth from mouth and nose. Staining, erosion and ulceration may be present at near female external genitalia and it should also be examined for evidence of abortifacient agents or torturing agents used.
Dermal Clues
Skin should be examined for the color of postmortem staining, alopecia, hyper-pigmentation, hyperkeratosis and injection marks. Furthermore, great attention should be paid to find any blister and hemorrhagic spots under the skin. Carefully inspect fingernails, antecubital fossae, ankles, dorsum of the hands for syringe marks. Apart from these, tattoos should also be examined for syringe marks. Sometimes injection marks are deliberately defaced by cigarette burns. Jaundiced skin may be seen in phosphorus poisoning or yellow in case of acute copper poisoning. Cherry red appearance of skin suggests carbon monoxide poisoning. Deep cyanosis and bright red skin may indicate the poisoning due to the opium and hydro cyanic acid respectively. Nitrates, potassium chlorate and aniline poisoning cause brown or deep blue postmortem staining. There is early onset of rigor mortis and decomposition in cases of strychnine and hydrogen sulphide poisoning (Table 6).
Internal Findings
Autopsy is mandatory in all the cases where, there is a doubt that a drug or poison is concerned as a probable cause of death except of two conditions. The first condition is when, the patient has died due to overdose of drug in a hospital and hospital’s toxicology laboratory confirmed the lethal level of drug. In the second case, when the patient has been died due to overdose and leaves circumstantial evidences like suicide note, history of suicidal tendencies or missing medication, etc and the absence of any other possible clue of cause of death. Various poisons or drugs cause death without leaving specific, readily identifiable external or internal manifestation. In such cases, the autopsy fails to reveal the actual cause of death. In such instances, it is very complicated for an analyst to carry out the toxicological studies with the existing situations and facilities available.
Odor
The odor should be noted while opening the body. The distinctive odor may emanating in some poisons such as garlic like odor (organophosphate insecticides, arsenic), smell of oil of wintergreen (methylsalicylates), noxious rotten-egg smell (sulfur dioxide and hydrogen sulfide), mowed hay (phosgene) and bitter-almond scent is associated with cyanide as discussed earlier sections.
Mouth and Throat
Mouth and throat are also examined for any evidence of inflammation, erosion and staining. These are also examined for the signs of corrosives or irritant poisons. Corrosive chemicals are responsible for corrosion, ulceration and desquamation of inner aspects of lips, mucus membrane of mouth and tongue [58]. Swollen, sodden, translucent, bleached tongue and mucus membrane of mouth may result due to corrosive alkali. Swollen gums, with foetid smell are the signs of acute mercuric chloride poisoning and chronic phosphorus poisoning [59,60]. Blue lining in the gum is found in the case of chronic lead poisoning. Chalky white discoloration of the teeth indicates sulphuric acid poisoning. Necrosis may be seen in pharynx manifested with agranulocytosis causes by dinitophenol suphonamides, amidopyrine, thiouracil and birbiturates. Nitric acid poisoning is characterized by pharynx lined with the softened and hyperemic mucous membrane and edema may be extensive at the opening of the larynx. Superficial opaque brownish stains may be seen in pharynx.
Esophagus
In the nitric acid poisoning, the esophagus is corroded in its upper part and hydrochloric acid produces dilated esophagus with the reddened and inflamed mucous membrane [61]. Desquamation and softening mucous membrane of the esophagus are evident in most of the corrosive alkalis poisoning. Swollen engorged mucous membrane of esophagus with patches of ulceration may be seen in iodine, mercuric chloride and acute poisoning of cantharidine. Perforation may be found in paraquat and fluoride poisoning. Contracted and the tough esophagus with whitened mucous membrane thrown up into folds and longitudinal red fissures in the mucosa may be produced by phenol poisoning. In case of antimony poisoning, esophagus is lined with yellowish-white pseudo-membranous deposit. Moreover, strong solution of potassium cyanide can cause wrinkle in mucous membrane of the esophagus with peculiar reddish-brown color.
Upper Respiratory Tract
Larynx, trachea and bronchi should be examined for any evidence of volatile irritant and inhaled poisonous material. Alcohol and barbiturates are mainly cause laryngeal edema. If the corrosive poison has been entered into respiratory tract, edema of glottis, congestion and desquamation of mucous membrane of trachea and bronchi may be seen. Congested larynx, trachea and inflamed bronchi have been reported in hydrochloride poisoning with whitish-grey opaque layer mucous membrane which can be rubbed off also. Swollen laryngeal and tracheal mucosa, edema at layer of vocal cords may be seen in ammonia poisoning [62]. Inflamed larynx and trachea with the reddened bronchi are the features of caustic alkalis poisoning. They also contain viscid and purulent mucus. Frothy bloodstained mucus is found in larynx and trachea due to potassium cyanide poisoning. Congested larynx, trachea and bronchi are the characteristics findings of veronal poisoning.
Lungs
Lungs are congested and edematous in most of the cases. If ammonia and phenol poisoning patient have survived for few days, broncho-pneumonia would be present in those cases. Severe effusions of blood into the pleural cavity, congested lungs, especially in the lower lobes have been observed in the antimony poisoning. Bloodstained effusions in the pleural cavity, subpleural hemorrhages and congested lungs may be associated with the phosphorus poisoning. Potassium cyanide poisoning may be linked with the congested or edematous lungs and petechial hremorrhages under the pleura. Hyperremia of the lungs has been described in cocaine poisoning. Eedematous, hypostatic congested lungs and patches of early broncho-pneumonia may be found in morphine or veronal toxicity. Engorgement of the lungs is the characteristic feature of strychnine poisoning.
Stomach
Discoloration and other remarkable appearances of the stomach during autopsy give rise to the question of cause of death. Unusual discolorations of the mucous membranes are mostly described in context of poisoning. When dealing with the examination of stomach and its contents, any unusual appearance, such as the hyperemia, softening, ulceration, perforation and presence of any foreign material should be noted. These signs are usually seen in corrosive and irritant chemical poisoning. In many drug poisoning cases, color and appearance may also be found normal in the stomach.
Hyperemia
It is the redness caused by an excess of blood in the mucous membrane of cardiac end of stomach. It is a deep crimson coloration, sometimes may be patchy or diffused and color of mucus membrane of stomach is velvety in arsenic poisoning. Patchy and diffused hyperemia is usually most marked with cardiac end and rarely with pyloric end of stomach. Various substances like fruit juice may also cause discoloration. Hyperemia is spreaded over whole surface of stomach and not in patches due to some disease condition but ridges of the mucus membrane is more affected in poisoning. The feature of hyperemia that differentiates it from asphyxial death is characterized by venous congestion. Hyperemia is also found on the mucus membrane of stomach in natural death, but it is only extended to the posterior wall of stomach without thickening of the wall. Generally irritant poison causes hyperemia in the mucous membrane of stomach. Sometime phenol transudes through the stomach wall and mucus membrane turns into whitish cooked appearance. Phenol may cause small hemorrhagic spots, consistency, corrugated and redbrown mucous membrane. If the solution of the corrosive mercurial salts has been swallowed, mucous membrane is converted into an opaque grayish-white color. Some effusion of blood may take place in sub mucous coat due to antimony poisoning. In this case peritoneal of stomach is also inflamed and white aphthous patches may be present. The mucous membrane of stomach is swollen, grayish-white in coloration and small ecchymosis is caused by phosphorus. The walls of vessels are wrinkled, become peculiar reddish-brown in color, distended and blood is found in the stomach due to potassium cyanide poisoning. Pale stomach has been found in chloroform poisoning.
Softening
Most of the corrosives and irritant poisons cause damage to epithelium and secrete excess mucus due to irritation. Generally softening is caused due to these poisons, which is mostly seen in cardiac end of stomach along with great curvature. All corrosives do not cause softening, corrugate and harden mucus membrane of stomach but may be seen in carbolic poisoning. Softening is almost caused by alkalis. The softening may affect the entire thickness of stomach wall. If softening occurs due to poisoning, then it is limited to the mucus membrane, but in some cases it extends to muscular coat and mucus membrane may be detached in patches over the softened part. Softening is also found at cardiac end of stomach in diseased conditions. Postmortem softening may occurs in most dependent part and all layers of stomach wall without any inflammation around the softened patches.
Perforation
Chemical ulceration is examined without cutting of stomach because ulceration is found along the greater curvature. Ulceration may develop in corrosive or irritant chemical poisoning within 24-72 hours of exposure. Erosion with thin friable margins may also found in ulceration. The surrounding mucosa is softened due to inflammation and there is diffuse hyperemia. Chemical induced ulceration differs than the ulcer developed in disease condition as disease ulcer develops at the lesser curvature with well defined margins and localized zone of hyperemia around it.
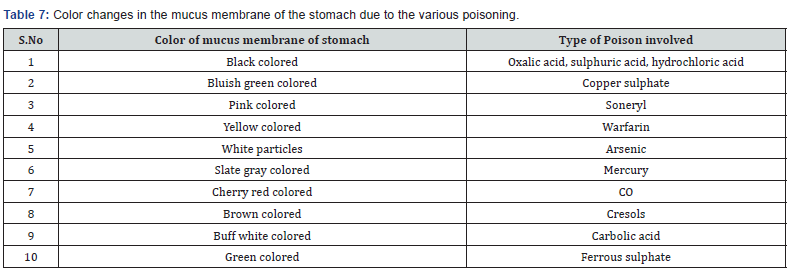
Perforation in stomach may result in two ways; by corrosion and by ulceration. Perforation occasionally takes place in stomach due to sulphuric acid or ammonia poisoning. Sulphuric acid may cause extensive destruction and blackness of stomach. There may be irregular aperture, sloughing of edges and adjacent tissues are easily torn in sulphuric acid poisoning. However, in case of irritant poisons, there is little perforation. Stomach perforation has also been reported in the piroxicam chronic poisoning [63]. Inflammation of peritoneum is referred to the perforation due to disease. The perforation associated with disease has an oval or rounded aperture at the stomach with smooth or thickened edges. The possible causes for the color of mucus membrane of stomach have been listed in Table 7.
Stomach Content
Examination of stomach contents can reveal when the victim had last meal and what meal he had. This is crucially important to determine time of death. Meals that are partially digested, completely digested or not digested at all can reveal time frame of death. The greater curvature should be opened carefully in jar for the collection of stomach content and gastric line is also examined. Further, contents are scraped out and any foreign material, such as powder, capsules, fragment of leaves or fruits, cantharides and tablets are picked off, which are either added to the main jar or collected in separate container. The contents should be carefully preserved and color of the contents should be noted. In the antimony poisoning, on opening of stomach, content is found to contain a viscus, dark, bloody, gruellike fluid while, oxalic acid usually causes a brown gelatinous stomach contents.
Intestine
Small intestine may show irruption and sometimes may also show the presence of poisonous content. Ulceration is commonly seen in large intestine and a moderate degree of congestion is seen in small intestines in case of mercurial poisoning. Dark grumous content will be found in intestine due to sulphuric acid poisoning. Acute arsenical poisoning may causes inflammation in the upper part of mucous membrane of small intestine with delayed death or the whole intestine may be inflamed. Upper part of the small intestine is deeply bile stained and whole length of small intestine may be congested with the caustic alkalis poisoning. In oxalic acid poisoning, the mucous membrane of the upper part of the small intestine becomes soft, brittle and inflamed. Enteritis is usually present in large intestine and in addition to it; patches of pigmentation may also be present in mucous membrane in chronic lead toxicity. Intestines were found to shrunken in formalin poisoning with the grayish black coloration of mucosa of large intestine or mucosal folds can also be distinctly marked [64].
Liver
Liver is the most valuable tissue specimen in most of the postmortem toxicology cases. Metabolism of drugs and chemicals is carried out in liver, it breaks them into substance that can be either lower or higher toxic. Some drugs or chemicals may cause degenerative changes in the liver and lead to malfunctioning. The color of the liver may be different from the normal in many poisoning conditions. Fatty liver may result due to some poisons and also lead to fulminant hepatic necrosis. The liver will be slightly enlarged and becomes pale in the phenol, chloral hydrate, chloroform and mercurial poisoning [65]. Sometimes liver may become fatty and friable in such cases. Fatty degeneration of parenchyma with enlargement of the liver has been observed in cocaine poisoning. The liver may be soft and doughy enlarged and may shows a soft, bright yellow or saffronic appearance from severe fatty degenerative changes in case of phosphorus poisoning.
Chronic arsenic exposure may cause enlarged liver, advanced fatty changes. However, in acute exposure of arsenic may shows cloudy swelling, paleness with characteristic of fatty changes in the liver [66].
Kidneys
Lesions on kidneys may be found due to chronic poisoning of chromium. Degenerative changes of the kidney may observe along with reddishness, swelling, softness and sometimes greasy in touch with haemorrhage in calyces in cases of poisoning with mercury, arsenic, phosphorus, cantharides, oxalic acid and viper snake venom etc. [67-69]. The internal postmortem examination shows fatty degeneration of kidneys in the chloroform poisoning. Congestion has also been observed in kidneys in some cases of cocaine, phenol and oxalic acid poisoning. Besides, in some case of oxalic acid poisoning, presence of the white powder of oxalate crystals in tubules and calyces has also been observed which give a gritty appearance on section. Owing to death from chronic poisoning of arsenic, kidneys are enlarged. In case of lead poisoning, kidneys are usually smaller than normal size and resemble the arteriosclerosis condition. The surface becomes fine, yellow granular with reddish depressions. The kidneys may show port-wine-color as in case of presence of hrematoporphyrin in sulphonal poisoning.
Heart
Presence of subendocardial haemorrhagic spots in left ventricle indicates that possible reason of death is arsenic, phosphorus and mercuric chloride poisoning etc. Ecchymoses are frequently observed in wall of left ventricle of heart with coagulated blood in acute arsenic poisoning. In chronic poisoning of arsenic, death is occurred due to heart failure and fatty diffuse degeneration of myocardium with pale flabby and friable appearances is also observed in the heart. Flabby and fatty heart with paleness muscles may also result in phosphorus poisoning. Opium poisoning may be characterized with swelling in right side of heart with dark blood. In case when death is caused due to carbon mono oxide poisoning, the right side of the heart is engorged with blood while the left side of the heart is empty [70,71]. In potassium cyanide poisoning, right side of the heart appears swollen with imperfectly clotted blood and minute hremorrhagic points in pericardium. The right heart is dilated to a great extent than the left and veins are usually full of dark blood in veronal poisoning cases. Fatty degeneration may be seen in heart during postmortem due to chloroform poisoning.
Brain and Spinal Cord
Brain and spinal cord may be congested or oedematous, particularly in case of cerebral and spinal poisons. Petechiae with edema in white matter are often seen in cases of asphyxiant poisons [72]. The brain and meninges usually show congestion with phenol poisoning. Vessels are distended with dark blood on the surface of brain with numerous small bleeding points and congestion of dura mater with the antimony poisoning. Veronal and phosphorus may cause congestion of meninges and its brains. Hyperemia of brain has been described in cocaine poisoning [73]. Morphine may also results in distention of brain vessels and meninges with blood. Sometimes edema may be present and occasionally there is little increase of fluid in ventricles. Congestion may found in the brain and in the upper part of the spinal cord due to poisoning of strychinine [74].
Spleen
Congested spleen is found with the morphine and it may be somewhat atrophied and fibrotic in lead poisoning.
Urinary Bladder
Examine mucosa of the urinary bladder for different lesions and quantity or characters of urine should be noted after opening of the bladder. For example, greenish smoky urine in bladder indicates toxicity due to phenol. Haemorthage may occur in the urinary bladder in case of abrus pecataorious, snake bite and cantharides poisoning.
Vagina and Uterus
Examination of vagina or uterus is carried out for staining, congestion, haemorthages and ulceration which are necessary in cases of attempted abortion by the use of local abortifacient agents.
Conclusion
Various approaches have been explored to summarize the information in context to diagnosis of poisoning in the discipline of post-mortem toxicology and thorough guidance has been provided to establish the cause of toxicity. Diagnosis of poisoning is extremely important in unconscious people for the management of poisoning. Diagnosis other than poisoning must also be considered because some clinical features may result due to diseases or by secondary effects such as anoxia. Poisoning with the various compounds may be misdiagnosed due to resemblance of clinical feature with disease conditions like high dose of paracetamol, thallium and paraquat has been associated with the hepatitis, paraesthesia and pneumonitis diseases respectively. Diagnosis of poisoning is extremely difficult in death cases, where drugs are used to cure disease, however, results in casualty due to either over dose or side effects. This review was needed to enhance the evidence based knowledge, for the diagnosis of poisoning in the discipline of forensic toxicology.
References
- Aggarwal NK, Aggarwal BBL (1998) Trends of poisoning in Delhi. J Ind Acad for Med 20: 32-6.
- Klepac T, Busljeta I, Macan J, Plavec D, Turk R (2000) Household chemicals- -common cause of unintentional poisoning. Arh Hig Rada Toksikol 51: 401-7.
- Asghar A, Anees M, Mahmood KT (2010) Accidental Poisoning in Children. J Biomed Sci and Res 2: 284-289.
- Majowicz SE, Meyer SB, Kirkpatrick SI, Graham JL, Shaikh A, et al. (2016) Food, health, and complexity: towards a conceptual understanding to guide collaborative public health action. BMC Public Health 16: 487
- Stevenson R, Tuddenham L (2014) Novel psychoactive substance intoxication resulting in attempted murder. J Forensic Leg Med 25: 60- 61.
- Flaig B, Zedler B, Ackermann H, Bratzke H, Parzeller M (2013) Anthropometrical differences between suicide and other non-natural death circumstances: an autopsy study. Int J Legal Med 127(4): 847-56.
- Gold KJ, Sen A, Schwenk TL (2013) Details on suicide among US physicians: data from the National Violent Death Reporting System. Gen Hosp Psychiatry 35(1): 45-9.
- Chavoushi SF, Mesman L, Noordzij PG, Sikma MA, van Maarseveen EM (2016) Attempted suicide with barbiturates purchased online Ned Tijdschr Geneeskd 160: D491.
- Greene SL, Dargan PI, Jones AL (2005) Acute poisoning: understanding 90% of cases in a nutshell. Postgrad Med J 81: 204-216.
- Landrigan PJ (1982) Occupational and community exposures to toxic metals: lead, cadmium, mercury and arsenic. West J Med 137: 531-9.
- Krantz A, Dorevitch S (2004) Metal exposure and common chronic diseases: a guide for the clinician. Dis Mon 50(5): 220-62.
- Dhatrak SV, Nandi SS (2009) Risk assessment of chronic poisoning among Indian metallic miners. Indian J Occup Environ Med 13(2): 60- 64.
- Najafi M, Sheikhvatan M, Montazeri A, Sheikhfathollahi M (2009) Quality of life in opium-addicted patients with coronary artery disease as measured with WHOQOL-BREF. Int J Soc Psychiatry 55(3): 247-256.
- Thompson TM, Theobald J, Lu J, Erickson TB (2014) The general approach to the poisoned patient. Dis Mon 60(11): 509-524.
- Erickson TB, Thompson TM, Lu JJ (2007) The approach to the patient with the unknown overdose Emerg Med Clin North Am 25(2): 249- 281.
- Nordt SP, Campbell C, Medak A, Tomaszweski C, Clark RF (2011) Ultrasound visualization of ingested tablets: a pilot study. Pharmacotherapy 31(3): 273-276.
- Martinez MA, Ballesteros S (2009) Toxicological findings in two planned complex suicide cases: ingestion of petroleum distillates and subsequent hanging. J Anal Toxicol 33(6): 336-42.
- Dinis Oliveira RJ, Carvalho F, Moreira R, Proença JB, Santos A, et al. (2015) Clinical and forensic signs related to chemical burns: a mechanistic approach. Burns 41(4): 658-79.
- Martens F (2001) Suspected poisoning. What kind of emergency care? MMW Fortschr Med143(49-50): 28-33.
- Martinez MA, Ballesteros S, Sanchez de la Torre C, Almarza E (2005) Investigation of a fatality due to trazodone poisoning: case report and literature review. J Anal Toxicol 29(4): 262-8.
- Ghosh S (2014) A typical manifestations of organophosphorus poisoning following subcutaneous injection of Dichlorvos with suicidal intention. Indian J Crit Care Med 18(4): 244-246.
- Behal N, Wong A, Mantara R, Cantrell FL (2016) Human Poisoning Through Atypical Routes of Exposure. J Community Health 41(1): 105- 8.
- Krenzelok EP, Leikin JB (1996) Approach to the poisoned patient. Dis Mon 42(9): 509-607.
- Bosse GM, Matyunas NJ (1999) Delayed toxidromes. J Emerg Med 17(4): 679-90.
- Nehlig A, Daval JL, Debry G (1992) Caffeine and the central nervous system: mechanisms of action, biochemical, metabolic and psychostimulant effects. Brain Res Brain Res Rev 17(2): 139-170.
- Harper SJ, Jones NS (2006) Cocaine: what role does it have in current ENT practice? A review of the current literature. The Journal of Laryngology and Otology 120(10): 808-811.
- Heal DJ, Smith SL, Gosden J, Nutt DJ (2013) Amphetamine, past and present a pharmacological and clinical perspective. Psychopharmacol 27(6): 479-496.
- Hamel JA (2011) Review of acute cyanide poisoning with a treatment update. Crit Care Nurse 31(1): 72-81.
- Reiter CE, Alayash AI (2012) Effects of carbon monoxide (CO) delivery by a CO donor or hemoglobin on vascular hypoxia inducible factor 1α and mitochondrial respiration. FEBS Open Bio 24: 113-118.
- Wongtanate M, Sucharitchan N, Tantisiriwit K, Oranrigsupak P, Chuesuwan A, et al. (2007) Signs and symptoms predictive of respiratory failure in patients with foodborne botulism in Thailand. Am J Trop Med Hyg 77(2): 386-389.
- Leibson T, Lifshitz M (2008) Organophosphate and carbamate poisoning: review of the current literature and summary of clinical and laboratory experience in southern Israel. Isr Med Assoc J 10(11): 767-70
- Amundsen EJ, Reid MJ (2014) Self-reports of consumption of amphetamines, cocaine and heroin in a survey among marginalized drug users. Sci Total Environ 487: 740-745.
- Bowyer JF, Hanig JP (2014) Amphetamine and methamphetamineinduced hyperthermia: Implications of the effects produced in brain vasculature and peripheral organs to forebrain neurotoxicity. Temperature (Austin) 1(3): 172-82.
- Zhang Y, Zhong BL, Li Y, Ma ZL, Tian Y, et al. (2012) Brain event related potentials associated with psychiatric symptoms in amphetamine-type stimulant dependent patients. Int J Psychiatry Med 43(2): 189-196.
- Şanlıdag B, Derinoz O, Yıldız N (2014) A case of pediatric age anticholinergic intoxication due to accidental Datura stramonium ingestion admitting with visual hallucination. Turk J Pediatr 56(3): 313-315.
- Peduto VA, D’Uva R, Piga M (1996) Carbamate and organophosphate poisoning. Minerva Anestesiol 62(1-2): 33-54.
- Vale A, Lotti M (2015) Organophosphorus and carbamate insecticide poisoning. Handb Clin Neurol 131: 149-168.
- Jang DH, Manini AF, Trueger NS, Duque D, Nestor NB (2010) Status epilepticus and wide-complex tachycardia secondary to diphenhydramine overdose. Clin Toxicol 48(9): 945-8.
- Madhuvrata P, Singh M, Hasafa Z, Abdel Fattah M (2012) Anticholinergic Drugs for Adult Neurogenic Detrusor Overactivity: A Systematic Review and Meta-analysis. Eur Urol 62(5): 816-30.
- Matos ME, Burns MM, Shannon MW (2000) False-positive tricyclic antidepressant drug screen results leading to the diagnosis of carbamazepine intoxication. Pediatrics 105(5): E66.
- Mowry JB, Spyker DA, Brooks DE, McMillan N, Schauben JL (2015) Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 32nd Annual Report. Clin Toxicol 53(10): 962-1147.
- Lineberry TW, Bostwick JM (2006) Methamphetamine abuse: a perfect storm of complications. Mayo Clin Proc 81(1): 77-84.
- Swanson SM, Sise CB, Sise MJ, Sack DI, Holbrook TL, et al. (2007) The scourge of ethamphetamine: impact on a level I trauma center. J Trauma 63(3): 531-537.
- Bronstein AC, Spyker DA, Cantilena LR Jr, Green JL, Rumack BH, et al. (2011) Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 29th Annual Report. Clin Toxicol (Phila) 50(10): 911-1164.
- Sue YM, Lee YL, Huang JJ (2002) Acute hyponatremia, seizure, and rhabdomyolysis after ecstasy use. J Toxicol Clin Toxicol 40: 931-932.
- Budisavljevic MN, Stewart L, Sahn SA (2003) Hyponatremia associated with 3,4-methylenedioxymethylamphetamine (“Ecstasy”) abuse. Am J Med Sci 326(2): 89-93.
- Hollander JE, Henry TD (2006) Evaluation and management of the patient who has cocaine-associated chest pain. Cardiol Clin 24(1): 103-14.
- Chen HY, Albertson TE, Olson KR (2016) Treatment of drug-induced seizures. Br J Clin Pharmacol 81(3): 412-429.
- Weaver MF (2015) Prescription Sedative Misuse and Abuse. Yale J Biol Med 88(3): 247-256.
- Dyson EH, Proudfoot AT, Bateman DN (1985) Quinine amblyopia is current management appropriate? J Toxicol Clin Toxicol 23(7-8): 571- 8.
- Mackie MA, Davidson J, Clarke J (1997) Quinine - acute self-poisoning and ocular toxicity. Scott Med J 42(1): 8-9.
- Barceloux DG, Bond GR, Krenzelok EP, Cooper H, Vale JA (2002) American Academy of Clinical Toxicology practice guidelines on the treatment of methanol poisoning. J Toxicol Clin Toxicol 40(4): 415-46.
- Bogle RG, Theron P, Brooks P, Dargan P I, Redhead J (2006) Aluminium phosphide poisoning. Emerg Med J 23(1): e3.
- Rastogi SK, Tripathi S, Ravishanker D (2010) A study of neurologic symptoms on exposure to organophosphate pesticides in the Indian J Occup Environ Med 14(2): 54-57.
- Chandravanshi LP, Yadav RS, Shukla RK, Singh A, Sultana S, et al. (2014) Reversibility of changes in brain cholinergic receptors and acetylcholinesterase activity in rats following early life arsenic exposure. Int J Dev Neurosci 34: 60-75.
- Beveridge GW, Lawson AA (1965) Occurrence of bullous lesions in acute barbiturate intoxication. Br Med J 1(5438): 835-837.
- Olson KR, Benowitz NL (1984) Environmental and drug-induced hyperthermia. Pathophysiology, recognition, and management. Emerg Med Clin North Am 2(3): 459-474.
- Castano R, Thériault G, Gautrin D (2007) Categorizing nasal septal perforations of occupational origin as cases of corrosive rhinitis. Am J Ind Med 50(2): 150-153.
- Smith GE (1985) Fluoride, teeth and bone. Med J Aust 143: 283-286.
- Eide R, Schiønning JD, Ernst E, Hansen IM, Wesenberg GR (1995) Mercury content in rat teeth after administration of organic and inorganic mercury. The effects of interrupted exposure and of selenite. Acta Odontol Scand 53(1): 12-16.
- Broor SL, Kumar A, Chari ST, Singal A, Misra SP, et al. (1989) Corrosive oesophageal strictures following acid ingestion: clinical profile and results of endoscopic dilatation. J Gastroenterol Hepatol 4(1): 55-61.
- Walton M (1973) Industrial ammonia gassing. Br J Ind Med 30(1): 78- 86.
- Russell R (1999) Defining patients at risk of non-steroidal antiinflammatory drug gastropathy. Ital J Gastroenterol Hepatol 31(1): S14-S18
- Dabrowski A, Szewczyk T, Peterlejtner T (1979) Gastrojejunal burns caused by formalin Pol Przegl Chir 51: 177-179.
- VanHeijst AN, Zimmerman AN, Pikaar SA (1977) Chloralhydrate-the forgotten poison. Ned Tijdschr Geneeskd 121: 1537-1539.
- Mazumder DN (2005) Effect of chronic intake of arsenic-contaminated water on liver. Toxicol Appl Pharmacol 206(2): 169-175.
- Chang LW, Sprecher JA (1976) Degenerative changes in the neonatal kidney following in-utero exposure to methyl mercury. Environmental Research 11(3): 392-406.
- Tanimoto A, Hamada T, Kanesaki H, Matsuno K, Koide O (1990) Multiple primary cancers in a case of chronic arsenic poisoning--an autopsy report. J UOEH 12(1): 89-99.
- Tonelli M, Pannu N, Manns B (2010) Oral phosphate binders in patients with kidney failure. N Engl J Med 362(14): 1312-1324.
- Kuller LH, Radford EP, Swift D, Perper JA, Fisher R (1975) Carbon monoxide and heart attacks. Arch Environ Health 30(10): 477-82.
- Kojima T, Nishiyama Y, Yashiki M, Une I (1982) Postmortem formation of carbon monoxide. Forensic Sci Int 19(3): 243-248.
- Varnell RM, Stimac GK, Fligner CL (1987) CT diagnosis of toxic brain injury in cyanide poisoning: considerations for forensic medicine. Am J Neuroradiol 8(6): 1063-1066.
- Ryan A, Molloy FM, Farrell MA, Hutchinson M (2005) Fatal toxic leukoencephalopathy: clinical, radiological, and necropsy findings in two patients. J Neurol Neurosurg Psychiatry 76(7): 1014-1016.
- Perper JA (1985) Fatal strychnine poisoning-a case report and review of the literature. J Forensic Sci 30(4): 1248-1255