Unsuccessful Treatment of Post Laryngoplasty Cough and Dysphagia with Initially Arthramid, then Subsequently Bone Cement, Injections of the Left Aryepiglottic Fold and Vocal Fold
Shaw D1*, Lexmond NS2 and Rosanowski SM3
1Singapore Turf Club, 1 Turf Club Avenue, Singapore
2Royal (Dick) School of Veterinary Studies, Easter Bush Campus, Midlothian, Scotland
3Digital agriculture, Grasslands Research Center, Agresearch ltd., Palmerston North, New Zealand
Submission: February 27, 2024; Published: March 19, 2024
*Corresponding author: Daniel Shaw, Singapore Turf Club, Turf Club Avenue, Singapore. Email: danshaw@turfclub.com.sg
How to cite this article: Shaw D*, Lexmond NS and Rosanowski SM. Unsuccessful Treatment of Post Laryngoplasty Cough and Dysphagia with Initially Arthramid, then Subsequently Bone Cement, Injections of the Left Aryepiglottic Fold and Vocal Fold. Dairy and Vet Sci J. 2024; 16(3): 555939. DOI: 10.19080/JDVS.2024.16.555939
Simple Summary
Prosthetic laryngoplasty is a commonly performed surgical treatment of laryngeal hemiplegia, which can cause exercise intolerance in horses. Well-documented complications of prosthetic laryngoplasty (or “tieback” surgery) include coughing, nasal discharge, and dysphagia. Treatment options of cough and dysphagia complications traditionally comprised of loosening or removing the prostheses, with resulting compromise of athletic performance. A newly described treatment showing encouraging results for the resolution of cough and dysphagia complications was the augmentation of either the aryepiglottic fold and/or the vocal fold with a bulking agent injected into the ventral aspects of these folds to thicken them and help block the passage of food material into the trachea during swallowing. This paper describes a case of augmentation (injection of both aryepiglottic and vocal folds) with initially Arthramid® and then subsequently bone cement in a thoroughbred racehorse with coughing and nasal discharge after undergoing prosthetic laryngoplasty surgery. While initially successful in the resolution of clinical signs, the augmentation was only of a relatively short duration (Arthramid® 4 weeks, bone cement 3 months) until swelling resolved and signs of dysphagia returned. Also, the levels of complications in other cases using bone cement (7/7 augmentation only temporary, 3/7 necrosis and sloughing, 2/7 initial excess swelling) have led this clinic to determine that the technique may not be as promising as initial reports suggest. Prevention of dysphagia or cough in the first instance with careful attention to degree of abduction and placement position of prosthesis particularly in the muscular process may be a more rewarding long-term strategy. In cases where dysphagia or cough does occur, we would now recommend either conservative management while waiting for some loss of abduction and symptoms to resolve, or removal of the prosthesis.
Abstract
Coughing, dysphagia, and nasal discharge are common complications of prosthetic laryngoplasty. Treatment options for these complications were limited to conservative management or removal of the prosthesis. In the last few years, a new minimally invasive procedure has been described. Filling the aryepiglottic or vocal folds with a bulking agent appears to improve the laryngeal seal and help prevent feed entering the trachea during swallowing. In this case, a 4-year-old thoroughbred racehorse underwent a double augmentation procedure. It was presented with nasal discharge and coughing 12 weeks after a successful prosthetic laryngoplasty surgery to treat its left-sided laryngeal hemiplegia, and 6 weeks after left aryepiglottic fold augmentation with Arthramid®. After initial resolution of symptoms with Arthramid® treatment, the augmentation of the aryepiglottic fold had rapidly resolved, and the symptoms had returned. Differing from previous augmentation procedures, this horse had both its aryepiglottic and vocal folds bulked up with bone cement. The surgery was initially successful, and the horse was noted to have greatly reduced coughing in as little as 24 hours following surgery. However, after three months, the swelling had subsided back to normal, and the cough and discharge had returned. This, and other complications in other cases at this clinic using bone cement augmentation, i.e., per acute inflammatory response (2/7 horses), necrosis and sloughing of either the aryepiglottic fold or the vocal fold (3/7 cases) and loss of augmentation swelling within months (7/7), has led the authors to reconsider the use of this technique.
Keywords: Thoroughbred; Complications; Post-laryngoplasty; Augmentation; Aryepiglottic fold
Introduction
Prosthetic laryngoplasty is a commonly performed surgical treatment of laryngeal hemiplegia, which can cause exercise in tolerance in horses [1-10]. However, complications are not uncommon following surgery, which has led to a moderate prognosis at best, and a wide variety in surgical techniques [11]. The most reported complication was loss of abduction [2]. This has led to several strategies such as using alternative suture materials, using two sutures, various reinforcements, alterations of placement positions of the sutures in the cartilage, and debridement of the cricoarytenoid joint [11,13]. The other well-documented set of complications of prosthetic laryngoplasty (or “tieback” surgery) include dysphagia, coughing and nasal discharge, relating to the presence of food, water, and saliva in the trachea during the swallowing process [11-13]. While this was a relatively rare complication in early studies [2], there has been more emphasis on this complication in more recent studies [1,11,14,15]. There is often a differentiation between “early onset” dysphagia and cough, and “late onset” or “chronic” [11].
The causes or contributing factors are thought to be over-abduction, too lateral an abduction or too caudal an abduction of the arytenoid cartilage. Other causes were penetration of the esophagus, adhesions, ventriculocordectomy procedures, the cricoarytenoid joint ablation, and unspecified neurological damage in the surgical procedure. Treatment options of cough and dysphagia complications post-laryngoplasty comprise conservative treatment in the first instance, i.e., feeding from the ground, treatment of tracheobronchitis, and hoping that the “normal” small degree of loss of abduction would lead to a resolution of the symptoms over a few months [11,13]. If the condition became chronic, or was acute and severe, then the treatment options were loosening or removing the prostheses, which may continue to affect athletic performance [16]. Options were to not replace the prosthesis, and hope that some fibrosis led to sufficient abduction to alleviate the laryngeal hemiplegia, or consider replacing the prosthesis slightly looser, or with more accurate placement, either at the same time as the removal or later [11,13].
A newly described treatment for cough and dysphagia post-laryngoplasty is the augmentation of either the aryepiglottic fold [15] or the vocal fold [14]. In this procedure, a bulking agent is injected into the ventral aspect of these folds to thicken them and help block the passage of food material into the trachea during swallowing [15]. This paper describes a case of double augmentation (injection of both aryepiglottic and vocal folds) in a thoroughbred racehorse with coughing and nasal discharge 12 weeks after undergoing prosthetic laryngoplasty surgery.
Materials and Methods
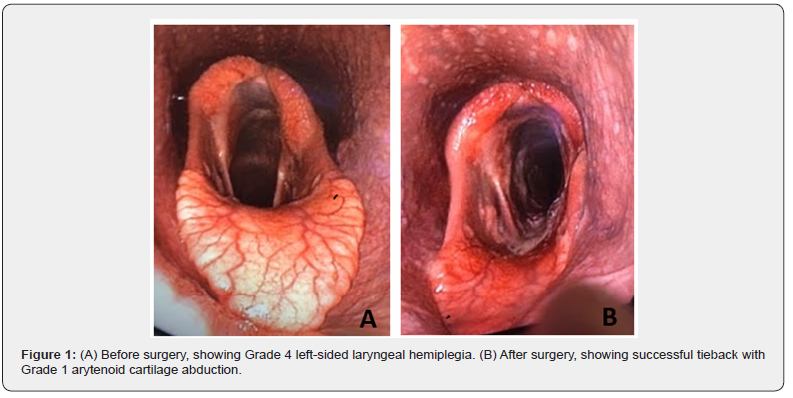
A 4-year-old racing thoroughbred was initially presented with loud respiratory noises during exercise. An endoscope performed at rest revealed Grade 4 left-sided laryngeal hemiplegia. The horse then underwent prosthetic laryngoplasty surgery, achieving Grade 1 left arytenoid cartilage abduction (Figure 1). Six weeks after the laryngoplasty, the horse was re-presented with nasal discharge and coughing. Endoscopy showed that the Grade 1 arytenoid abduction had been maintained. As the left arytenoid cartilage was unable to adduct fully during swallowing, small amounts of food material were able to enter the trachea, causing irritation, coughing and subsequent nasal discharge. The decision was made to augment the aryepiglottic fold such that it could fill the gap left open by the abducted arytenoid cartilage and improve the respiratory tract protection during swallowing. Under general anaesthesia, the left aryepiglottic fold of the horse was injected with Arthramid® Vet, a polyacrylamide hydrogel [15]. Following the procedure, the left aryepiglottic fold was seen to be swollen on endoscopic examination (Figure 2A) and provided a good laryngeal seal during swallowing. The coughing and nasal discharge was resolved at that time.
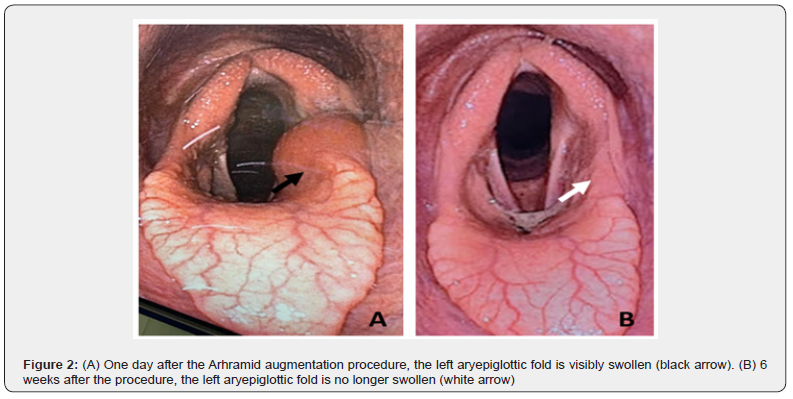
A further 6 weeks after the aryepiglottic fold augmentation (12 weeks after the initial laryngoplasty), the horse was once again presented to the hospital with a recurrence of coughing and nasal discharge. Endoscopic examination showed the left aryepiglottic fold was no longer swollen (Figure 2B). Arthramid® Vet was concluded to have only been of short-term benefit in bulking up the aryepiglottic fold.
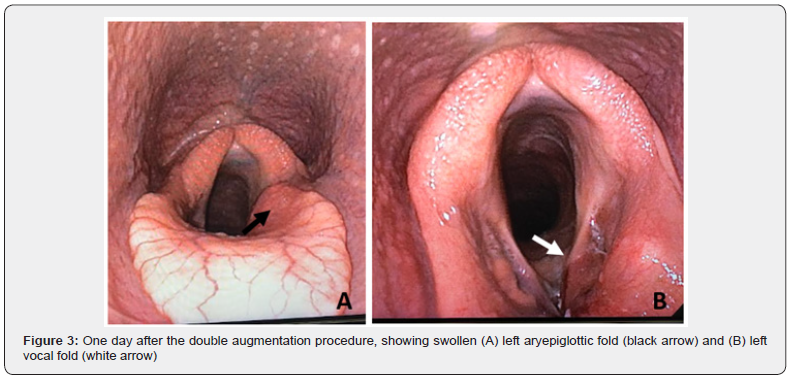
With the idea of using a more permanent substance, Stryker® Surgical Simplex P radiopaque bone cement (PMMA) was used as the bulking agent for a second augmentation procedure [14,15]. The PMMA was diluted, and an antibiotic was added in the ratio of 10.0g of the PMMA powder, 6.6ml of the PMMA liquid monomer and 0.5ml of amikacin sulfate. This ratio was tested prior to surgery and found to be fluid enough to pass through a 14-gauge needle while still retaining its hardening ability. The three components were measured out and set aside separately prior to the procedure.
The horse was sedated with a standard routine of 5ml of Xylazine and induced with 15ml of Ketamine and 5ml of Diazepam. It was then moved into dorsal recumbency to allow ventral access to the larynx, which was surgically prepped. A video endoscope was introduced through the horse’s mouth to allow visualization of the procedure. A 14-gauge 2½” catheter needle was placed in the cricothyroid space and advanced submucosally into the left aryepiglottic fold’s ventral aspect. Once the catheter needle was in place, the bulking agent components were mixed up and drawn up into a 5ml luer-lock syringe. The bulking agent was injected into the aryepiglottic fold submucosa (a few millimeters deep to the mucosa) until it was visibly swollen, about 1-3 ml was used. The mixture began to harden within two minutes. The same procedure was repeated with about 1-2 ml of bulking agent injected into the ventral submucosa of the left vocal fold, until it was visibly swollen. This completed the procedure, and the horse was then moved to the recovery room where it recovered without incident.
Results
An endoscopic examination performed the day after the surgery showed good thickening of both the left aryepiglottic and vocal folds. The horse was back in work within 24 hours of the procedure and was noted by both rider and trainer to have largely reduced its coughing, indicating imminent resolution of clinical signs. As bone cement is a more permanent substance, it was expected to offer lasting resolution. Over the next few months, the cough and discharge gradually returned, and a follow up endoscopic examination showed no obvious swelling in either the aryepiglottic fold or the vocal fold at three months post procedure.
Discussion
Laryngoplasty is a procedure with a well-documented complication rate. Traditionally the loss of abduction has been the major issue with surgeons and owners, leading to a range of variations in techniques to overcome this issue [17]. At this clinic, for example, over the years we have seen a change from 1 to 2 prosthesis [18], a change in suture choice from 5 metric ethibond to the 9 metric nylon (Securos system) [19], attention paid to “good bites” of the dorsal cricoid and the muscular process for less chance of “pull out” [11,13], and the opening up of the cricoarytenoid joint during surgery [20].
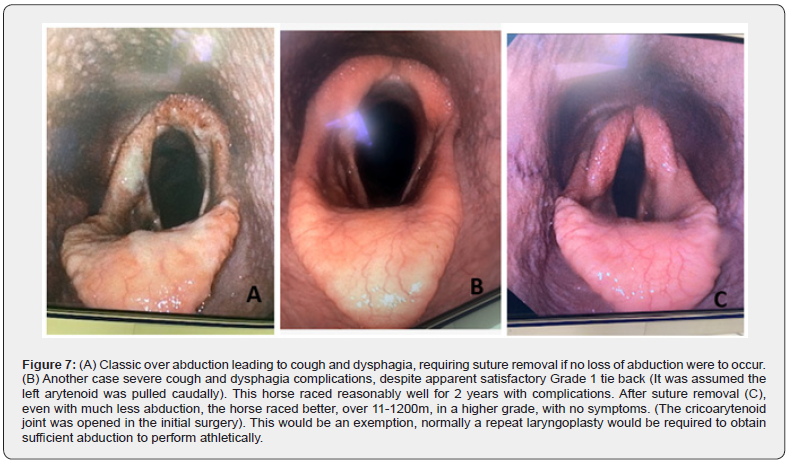
While dysphagia or cough complications were common in the early post-operative stages (up to 40%); in the long term, these were reported in only 6 to 10% of cases in a 2003 paper [2]. Another description of chronic or long-term cough or dysphagia is “late onset” [15]. The interesting concept is that having alterations in the technique to overcome the loss of abduction leads to an increase in long-term dysphagia or cough complication [11]. We can also reasonably expect surgeons being tempted to compensate for an expected loss of abduction post-surgery with a slight over abduction during surgery, which may be a contributing factor if the “normal” 1 to 2 grade loss of abduction were not to occur (Figure 7A).
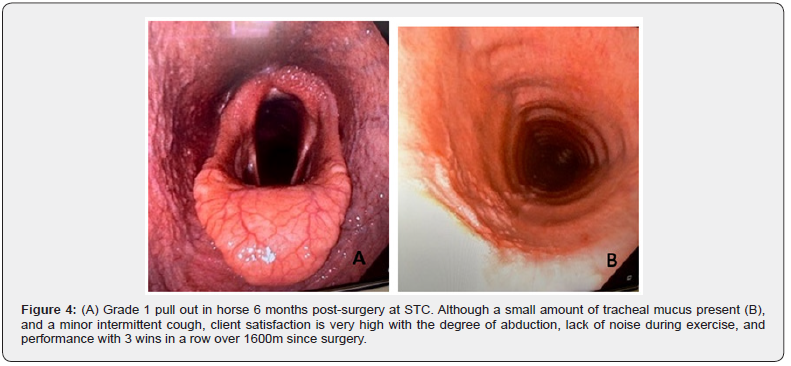
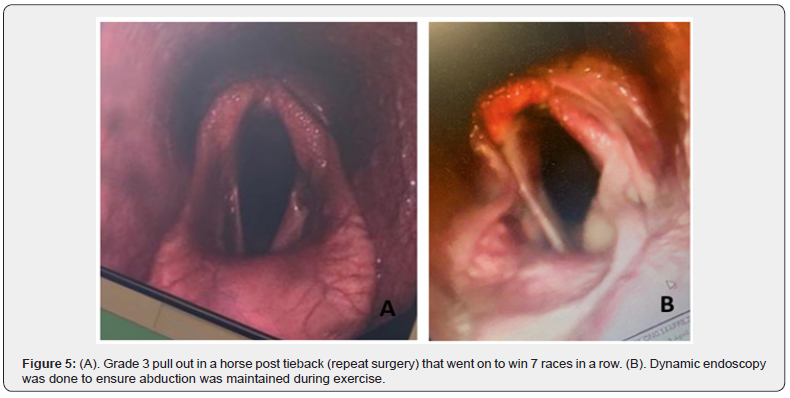
While surgeons are encouraged to aim for a Grade 2 pull out, and it was found that degree of abduction had no effect on performance [9], with modern social media and video endoscopy, there is no doubt client satisfaction is better with a Grade 1 pull out versus a Grade 3 (Figure 4), and many would aspire to this result in practice. In the authors’ experience, less abduction post-surgery is likely to lead to more respiratory noise, and the ability of the horse to perform over shorter distances only (100-1200m). However, it is accepted that individual exemptions do exist, and some individual horses can perform with very moderate abduction post-surgery (Figures 5). As clients become more aware of the effects on low grade respiratory disease on performance [21], there would be less tolerance for chronic cough and dysphagia, more routine endoscopic examination of the respiratory tract (with attention on the trachea) [22, 23] and these complications are more likely to be reported regardless of performance.
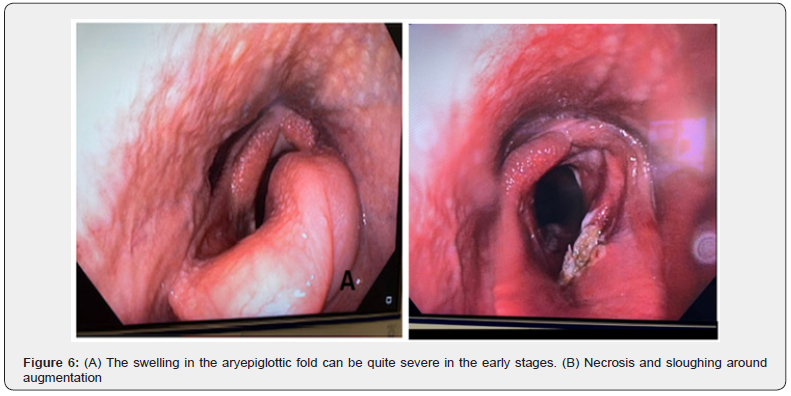
The hence increasingly common complication of cough and dysphagia has arisen requiring a remedy, the augmentation of the aryepiglottic fold and/or the vocal cord seemed an easy and highly satisfactory therapy. The rapid loss of the augmentation, with the return of the clinical signs in our hands, was a disappointing result. Added to this, other complications such as per-acute swelling in the short term (Figure 6A), and sloughing, necrosis, and fibrosis reaction (Figure 6B) has led us to abandon the technique, while waiting for further publications.
The strategy of this clinic in the meantime will be,
• Prevention, paying attention to recent advice and developments to placement position of the suture in the muscular process, which, if it is too advanced along the spine, will cause the arytenoid cartilage to be pulled caudally as well as abducted, leading to epiglottic failure dorsally on the left during the swallowing process.
• Other considerations, such as doing the procedure standing or under general anaesthesia, whether to open the cricoarytenoid joint or not, and whether to include ventricular cordectomy or not, the authors believe at this stage the evidence is still conflicting on whether to make a firm recommendation.
• If despite our best efforts we have cough or dysphagia post-surgery, our advice will be to wait 6 to 8 weeks and see if the condition spontaneously resolves.
• If the condition is chronic, (or “late onset”), and of a severity of client non-acceptance, or causing poor performance, then removal of the sutures would be in our experience the only option. Following this procedure, and especially if a long period of time has elapsed, or the cricoarytenoid joint was included in the initial surgery, we may have sufficient fibrosis that holds the arytenoid cartilage abducted enough to be able to perform (Figure 7C). However, in most cases, we must be prepared that athletic ability will be compromised, and to put in another laryngoplasty, either at the time of suture removal, or (in our preference) 3 to 6 months later.
Conclusion
Double augmentation of both the aryepiglottic and vocal folds seemed to be a viable procedure to correct cough and dysphagia following prosthetic laryngoplasty. It was minimally invasive and should not have interfered with athletic improvement following the initial prosthetic laryngoplasty procedure or required time out of work to recover and promised immediate resolution of clinical signs. However, the augmentation was relatively short lived, a few weeks only with the Arthramid® and a few months only with the bone cement. In addition, some other side effects were noted in a series of cases in this clinic , being loss of swelling after a relatively short period (7/7 cases over 3-6 months), per acute swelling in the days following the procedure (2/7 cases), and necrosis and sloughing of either the vocal fold or the aryepiglottic fold (3/7 cases), leading the authors to conclude this technique may not be as promising as initially thought.
References
- De Clercq E, Rossignol F, Martens A (2018) Laryngeal hemiplegia in the horse: an update. Vlaams Diergeneeskd Tijdschr 87: 283-294.
- Dixon RM, McGorum BC, Railton DI, Hawe C, Tremaine WH, et al. (2003) Long term survey of laryngoplasty and ventriculocordectomy in older, mixed breed population of 200 horses, Part 1, Maintenance of surgical abduction and complications of surgery. Equine Vet J 35: 389-396.
- Goulden BE, Anderson LJ (1982) Equine laryngeal hemiplegia, Part III, Treatment by laryngoplasty. NZ Vet J 30: 1-5.
- Russel AP, Sloane DE (1994) Performance analysis after prosthetic laryngoplasty and bilateral ventriculectomy for laryngeal hemiplegia in horses :70 cases (1986-1991). J Am Vet Med Assoc 204: 1235-1241.
- Ducharme NG, Hackett RP (1995) Surgical alternative in the treatment of laryngeal hemiplegia in the horse. Swiss Vet 11: 59-61.
- Strand E, Martin GS, Haynes PF, McClure JR, Vice JD (2000) Career racing performance in Thoroughbreds treated with prosthetic laryngoplasty for laryngeal neuropathy; 52 cases (1981-1989). J Am Vet Med Assoc 217: 1689-1696.
- Davenport CL, Tulleners EP, Parente EJ (2001) The effect of recurrent laryngeal neurectomy in conjunction with laryngoplasty and unilateral ventriculocordectomy in Thoroughbred racehorses. Vet Surg 30: 417-421.
- Kidd JA, Slone DE (2002) Treatment of laryngeal hemiplegia in horses by prosthetic laryngoplasty, ventriculectomy and vocal cordectomy. Vet Rec 150: 481-484.
- Barakzai SZ, Boden LA Dixon PM (2009) Postoperative race performance is not correlated with degree of surgical abduction after laryngoplasty in National Hunt Thoroughbred racehorses. Vet Surg 38: 934-940.
- Marks D, Mackay-Smith MP, Cushing LS, Leslie JA (1970) Use of a prosthetic device for surgical correction of laryngeal hemiplegia in the horse. J Am Vet Med Assoc 157: 157-163.
- Rossignol F, Duscharme NG (2021) Complications in laryngeal surgery. In Complications in Equine Surgery. Rubio-Martinez LM, Hendrickson DA (Eds) Wiley-Blackwell Pp: 438-467.
- Hawkins JF, Tulleners EP, Ross MW, Evans LH, Raker CW (1997) Laryngoplasty with or without ventriculectomy for the treatment of left laryngeal hemiplegia in 230 racehorses. Vet. Surg 26: 484-491.
- Hawkins J (2014) Evaluation and management of horses with Dysphagia Following Prosthetic Laryngoplasty. In Advances in Equine Upper Respiratory Surgery. Hawkins, J (Eds) Wiley Blackwell Pp: 57-60.
- Luedke LK, Cheetham J, Mohammed HO, Ducharme NG (2020) Management of postoperative dysphagia after prosthetic laryngoplasty or arytenoidectomy. Vet Surg 49: 529-539.
- Vidovic A, Delling U (2017) Aryepiglottic fold augmentation as treatment for late-onset dysphagia following surgical treatment of recurrent laryngeal neuropathy. Tierarztliche Praxis Ausgabe G: Grosstiere - Nutztiere 45: 219-225.
- Cramp P, Barakzai SZ (2012) Surgical management of recurrent laryngeal neuropathy. Equine Vet Educ 24: 307-321.
- Byrne CA, Hotchkiss JW, Barakzai SZ (2023) Variations in the application of equine prosthetic laryngoplasty: A survey of 128 equine surgeons. Vet Surg 52: 209-220.
- Dart A, Tee E, Brennan M, Dart C, Perkins N, et al. (2009) The effect of prosthesis number and position on rima glottidis area in equine laryngeal specimens. Vet Surg 38: 452-456.
- Scherzer S, Hainisch EK (2005) Evaluation of a canine cranial cruciate repair system for use in equine laryngoplasty. Vet Surg 34: 548-553.
- Parente EJ, Birks EK, Habecker P (2011) A modified laryngoplasty approach promoting ankylosis of the cricoarytenoid joint. Vet Surg 40: 204-210.
- Holcombe SJ, Robinson NE, Derksen FJ, Bertold B, Genovese R, et al. (2006) Effect of tracheal mucus and tracheal cytology on racing performance in Thoroughbred racehorses. Equine Vet J 38: 300-304.
- Kusano K, Hobo S, Ode H, Ishikawa Y (2008) Tracheal endoscopic and cytological findings and blood examination results in thoroughbred racehorses suspected to have lower respiratory tract disease. J Equine Sci 19: 97-102.
- Koblinger K, Nicol J, McDonald K, Wasko A, Logie N, et al. (2011) Endoscopic Assessment of Airway Inflammation in Horses. J Vet Intern Med 25: 1118-1126.






























