Review on Epizootic Lymphangitis: Epidemiology and its Diagnosis
Ahmed Seid*, Mohammed Fedlu and Amana Mama
School of Veterinary Medicine, Wolaita Sodo University, Ethiopia
Submission: May 11, 2019; Published: May 29, 2019
*Corresponding author: Ahmed Seid, School of Veterinary Medicine, Wolaita Sodo University, Wolaita Sodo, Ethiopia
How to cite this article: Ahmed Seid, Mohammed Fedlu and Amana Mama. Review on Epizootic Lymphangitis: Epidemiology and its Diagnosis. Dairy and Vet Sci J. 2019; 12(1): 555830. DOI: 10.19080/JDVS.2019.12.555830
Abstract
Epizootic lymphangitis is a contagious fungal disease principally of equines that results from infection by a dimorphic fungus, Histoplasma capsulatum var. farciminosum. The disease commonly develops into a chronic debilitating condition that can manifest itself in one of three clinical forms: cutaneous, ocular and respiratory forms. The disease is primarily an ulcerating, suppurative, pyogranulomatous dermatitis and in most cases lymphangitis. Epizootic lymphangitis is a relatively common infectious disease of horses and other equids in certain parts of the world. The infection rate of EPL varies with the geographic area and the age of the animal. The disease has the potential to significantly impact the health and welfare of equids in countries in which it is endemic. EPL is second only to African Horse Sickness as a most important disease of horses in Ethiopia. The wounds caused by harness are reported as major predisposing factors of EPL in carthorses in Ethiopia. Currently, due to limited available diagnostic technologies, veterinarians in Ethiopia diagnose the disease based on clinical appearance and microscopic examination for yeast cells within pus. This has the potential for misdiagnosis, as the clinical appearance can mimic that of other diseases. Diagnosis is possible by direct visualization of the yeast form of the fungus in pus from infected lymphatic nodules and by culture or histopathologic examination of tissues from clinically affected cases. It is also possible to visualize the organism in stained histological sections of matured or developing lesions. EPL is an economically important disease in some areas of the world, particularly where large numbers of horses, donkeys, or mules are assembled. Different treatment modalities are available some of which are successful in treating early cases of the disease. Effective prevention and control of epizootic lymphangitis is based on euthanizing infected equids and the application of strict biosecurity measures.
Keywords: Epizootic lymphangitis; H. capsulatum var. farsiminosum; Equines; Epidemiology; Diagnosis
Abbrevations: CDC: Center for Disease Control; CFSPH: Center for Food Security and Public Health; CO2: Carbon Dioxide; DACA: Drug Administration and Control Agency; EPL: Epizootic Lymphangitis; H&E: Haematoxylin and Eosin; HCD: Histoplasma Capsulatum Variety Duboisii; HCF: Histoplasma Capsulatum Variety Farciminosum; OIE: Office International Des Epizootics; SDA: Sabouraud‟s Dextrose Agar; SPANA: Society for the Protection of Animals Abroad
Introduction
Equines have a prominent position in the countries agricultural and transport systems since the transportation activities are performed by equids [1]. They are mainly used as draught and pack animals and they are also used for ploughing in some parts of the country. However, despite all these uses, equids have several diseases. One of such rampant diseases is epizootic lymphangitis [2]. Epizootic lymphangitis is a debilitating fungal disease seen mainly in equids. The disease results from infection by a dimorphic fungus, Histoplasma capsulatum var. farciminosum. This organism has also been known as Histoplasma farciminosum, Cryptococcus farciminosum, Zymonema farciminosum and Saccharomyces farciminosum [3]. HCF was formerly described as an independent species, but this assessment has been changed and it is now considered a variety of H. capsulatum due to the close morphological similarities of both the mycelial and yeast forms [4].The organism exists as yeast in animal tissues and a saprophytic mycelium in the environment [5].
The incidence of the disease increases with assembling of equids [2]. The disease is primarily an ulcerating, suppurative, pyogranulomatous dermatitis and in most cases lymphangitis [6]. It was seen commonly in the extremities along front and hind legs, chest wall, belly and the neck. Moreover, it can also be detected as an ulcerating conjunctivitis of the palpebral conjunctiva with excessive ocular serious discharge, or rarely as a multifocal pneumonia [5]. The organism might also invade open fresh or non-fresh lesions including ruptured strangle‟s abscesses and male castrated wounds [7]. The disease is more common in the tropical and subtropical regions, than in temperate areas [5]. It is mostly diffused in areas characterized by humid and hot climates [8]. Biting flies and ticks can also transmit the disease [9]. The incubation period of epizootic lymphangitis is variable and it has three forms: the cutaneous, the ocular and the pulmonary depending on the route of entry [6]. In a recent study, the incubation period was much longer in a horse inoculated with mycelial organisms than in a horse inoculated with the yeast form [3]. Diagnosis of EPL is based on clinical signs, laboratory tests and isolation of the causative agent.
Many treatments have been tried largely without success. The disease is rarely responding to treatment [1]. Parenteral Amphotericin B and iodides have been reported as effective [10]. Successful treatment with intravenous administration of sodium iodide, oral administration of potassium iodide and surgical excision of lesions are limited, since recurrences of clinical signs months later is possible, Furthermore, in vitro sensitivity of the organism to amphotericin B, nystatin and clotrimazole has been reported However, in most areas, Epizootic Lymphangitis is a notifiable disease, and treatment is not allowed thereby, diseased animals must be forsaking [11]. Epizootic lymphangitis can be controlled or eradicated by quarantines and the euthanasia of infected animals [3]. Formularized aluminum hydroxide adsorbed, and heat attenuated vaccines have been widely used apparently with success [12]. The importance of epizootic lymphangitis is very considerable in countries in which it is prevalent not only with respect to the chronic debilitating effects of the disease on the health and welfare of affected animals but also on its socioeconomic impact on their owners who are entirely dependent on these animals for their livelihood and the support of their families [13]. Epizootic lymphangitis is reported to have a significant impact upon livelihoods within resource poor settings [14].
Therefore, the objective of this seminar paper is:
a. To review epizootic lymphangitis: epidemiology and its diagnosis
b. To highlight on the economic impacts of epizootic lymphangitis
Overview on Epizootic Lymphangitis
Epizootic Lymphangitis
Epizootic lymphangitis is a contagious fungal disease principally of horses and other equids, which is responsible for significant morbidity and debilitating illness in affected populations of horses, mules and to a lesser extent, donkeys [10]. The disease was also being called pseudofarcy or pseudoglanders. Moreover, another synonym is Equine histoplasmosis, Histoplasmosis, Farciminosis, African farcy, Equine Blastomycosis and Equine Cryptococcosis. It is clinically characterized by a spreading suppurative inflammation of cutaneous lymphatic vessels, lymph nodes and adjacent skin [15]. This disease is a chronic infectious granulomatous disease of the skin, lymph vessels and lymph nodes of the neck and legs of horses and other equines [16]. Epizootic lymphangitis is among the top diseases of equids that have severe economic and veterinary consequences in Ethiopia [2].
Etiology
Epizootic lymphangitis results from infection by a dimorphic fungus, Histoplasma capsulatum var. farciminosum [3]. The organism exists as yeast in animal tissues and saprophytic mycelium in the environment [5]. Not surprisingly, it can survive in the environment for extended periods of time, for about a month in dust or dirt and up to 10 weeks in non-sterile water. Warm, moist conditions are believed to favor its survival [13]. Identification of the agent is made by its appearance in smears of exudates or in histological sections of lesion material [6]. The most likely source of environmental contamination is pus discharging from cutaneous lesions primarily on the limbs of affected animals [16]. It is also believed that ticks may play a good role in the transmission of this agent [5].
Epidemiology
Epizootic lymphangitis is endemic in some countries of west, north and northeast Africa and Asia including India, Pakistan and Japan, where it is mostly diffused in areas characterized by humid and hot climates [7]. It is most commonly reported from North Africa and has been well documented in India [6]. In the endemic areas in certain regions of the world, the occurrence of seasonal dusty winds exposes horses to the inhalation of dust and spores, leading to pneumonia [17]. The infection rate of EPL varies with the geographic area and the age of the animal [18]. Historically, the disease was far more widely distributed than it is today, having been introduced into many European countries in which it was subsequently eradicated through implementation of a compulsory slaughter policy [10].
Transmission: The mode of transmission of EPL includes transmission by direct or indirect contact with traumatized skin, by biting flies, by ticks or by inhalation of HCF [19]. HCF is introduced via open wounds [13]. Spread of infection can also occur by indirect contact through contaminated objects such as grooming tools, feeding and watering utensils, and harnesses and through wound dressings [17]. Little evidence is available to describe risk factors for EPL, such as factors favoring persistence of the organism within the environment, the routes of transmission and potential vectors [9].
The wounds caused by harness are reported as major predisposing factors of EPL in carthorses in Ethiopia [20]. Experimentally, the disease can be transmitted by biting flies, e.g. Musca and Stomoxys spp that feed on open, discharging lesions. Flies may also transmit the skin form mechanically when they feed on lesions and exudates [9].Fungal spores can be trans-mitted to healthy animals by direct contact with infected animals or with inanimate objects or fomites, such as grooming equipment, bedding, saddler, etc., and enter the skin through cutaneous abrasions [7].
Both the yeast form found in animals and the mycelial form in the environment can produce epizootic lymphangitis after experimental inoculation. The source of the organisms can be the skin lesions and nasal and ocular exudates of infected animals, or the soil [3]. Ticks (Amblyoma and Boophilus) may also be involved in transmission. In a recent study, tick bites appeared to be a predisposing factor for epizootic lymphangitis in mules [7].
Species Affected: Epizootic lymphangitis mainly affects horses, donkeys and mules. H. capsulatum var. farsiminosum has also been reported in camels, cattle and dogs, and experimental infections have been established in mice, guinea pigs and rabbits [3]. Horses under six years of age are most susceptible [18]. In Africa, a third variety, which is known as Histoplasma capsulatum var. Duboisii (HCD), is the cause of human Histoplasmosis [21].
Morbidity and Mortality: The incidence of this disease is much higher when large numbers of animals are gathered together than when populations are less dense [3]. It causes considerable debility but low mortality that doesn’t usually exceeds 10% to 15% [17]. The main loss results from the inability of animals to work for several weeks because of extremely painful lesions [16]. Death is uncommon if an animal is in good condition and receives good care, but animals with extensive lesions may die [22].

Clinical Signs
Clinical signs of Epizootic lymphangitis are described based on the pathological lesions; otherwise the body temperature and general character of the animals are not changed. On the other hand, most of the animals will lose their body condition [18]. There are three forms of the disease. The three forms are cutaneous (skin), ocular and respiratory forms. The form that the disease takes seems to depend primarily on the route of entry [2]. The most common form of epizootic lymphangitis affects the Skin and lymphatic. It often occurs on the extremities, chest wall, face and neck, but can be seen wherever the organism is inoculated into a wound [3]. The cutaneous form of the disease, after which the disease was named, is the most common. The initial lesion is an open granulomatous wound along the course of a lymphatic vessel, which tends to ulcerate, or to undergo alternating periods of discharge and closure for some weeks before healing with residual scar formation [23]. The disease is insidious in onset, with a variable incubation lasting week to months. Clinically, the disease is characterized by a chronic suppurative, ulcerating pyogranulomatous dermatitis and lymphangitis. Severely affected animals become anorexic, deteriorate in condition and where there is joint involvement and lame [10] (Figure 1).

The ocular form of the disease results from inoculation of the organism into the eye, likely by biting flies [18]. It is less frequently observed and very rarely becomes generalized [10]. Initially, infection is characterized by a watery ocular discharge that may be unilateral or bilateral and variable swelling of the eyelids. This leads to the appearance of papules and button-like growths on the conjunctivae and nictitating membranes. The infection may extend to the periorbital tissues with formation of a granulomatous reaction. The secondary complications of the ocular form of the disease include corneal ulceration, panopthalmitis and myiasis [13] (Figure 2). Respiratory cases are thought to occur through inhalation of the organism either as spores from the environment or through extension of infection from the external mucous membranes of the nares or from the naso-lachrymal duct. Nodules can be present around the mucocutaneous junction of the nose and at postmortem are commonly seen to extend from the nasal passages, through the trachea and into the lung parenchyma [10]. At the hematological findings, leukocytosis, neutrophilia and an increase in the erythrocyte sedimentation rates can be observed [7]. The lesions are usually found near the external nares. These lesions may also occur in the lung. Affected animals develop a viscous mucopurulent nasal discharge and may exhibit dyspnea. Advanced cases exhibit progressive weakness, coughing and loss of bodily condition [13] (Figure 3).

Diagnosis
The diagnosis of EPL is based on the clinical examination of the lesions, microscopic examination of the yeast form of HCF in pus, serological tests and skin hypersensitivity testing [6]. Culture of the organism is necessary to confirm the presence of Histoplasma species but this is not without difficulty as the organism is slow growing and care must be taken to reduce overgrowth by contaminants. It is preferable to aspirate a sample from un-ruptured nodule after clipping and disinfecting the skin to reduce contamination. It is also possible to visualize the organism in stained histological sections of matured or developing lesions [10]. Inoculation of samples into immune suppressed mice can also be used for diagnosis [16]. Histofarcin, a skin test antigen for the diagnosis of epizootic lymphangitis is locally produced from the mycelial form of HCF in disease-endemic districts. Microscopic and mycological examinations of clinical lesions should be used as the „„gold standard‟‟ for the validation of this test [8].
Laboratory Diagnosis: Laboratory tests used in the diagnosis of epizootic lymphangitis include: identification of the yeast form of HCF in smears of exudates or in histological sections of material from lesions, serological tests (i.e., fluorescent antibody test, enzyme-linked immunosorbent assay and passive hem agglutination tests), skin hyper sensitivity test and isolation of the causative agent by culture [7]. The organism in the tissues is in its yeast form. It may be stained with Giemsa, Diff-Quick, or Gomori methenamine silver [16].
Direct Microscopic and Mycological Investigation
Pus samples collected from un-ruptured nodules were used for direct microscopic and mycological examinations. The nodules were washed with soap and water, shaved, and disinfected with alcohol. The contents of the nodules were aspirated with sterile needles and syringes and used for the preparation of smears for microscopic examination and isolation. The smears were fixed with methanol, stained with Gram‟s stain. Samples of lesions that include both viable and non-viable tissue should be collected in 10% neutral buffered formalin for histopathology. They should be kept refrigerated and sent to the laboratory on wet ice as soon as possible. Air–dried smears from exudates should be prepared on glass slides and fixed immediately for direct examination [3]. For the identification of the yeast form of HCF examination was made using oil immersion at 100 magnifications. In addition, material was inoculated aseptically onto slants of Sabouraud‟s Dextrose Agar (SDA, Oxoid) containing chloramphenicol (0.5 g/l) and enriched with 2.5% glycerol. For the isolation of the mycelial form, incubation was made at 26.8 °C and 5% CO2 and isolation of the yeast form was made at 37.8 °C and 5% CO2 [6]. The media were checked periodically and Gram-stained preparations were made from suspicious growth. Sub-culturing was made in antibiotic-free SDA slants of universal bottles.
Direct Microscopic Examination
Air–dried smears from exudates should be prepared on glass slides and fixed immediately for direct examination [3]. Before collection of samples the nodules were washed with soap and water, shaved, and disinfected with alcohol. The contents of the nodules were aspirated with sterile needles and syringes and used for the preparation of smears for microscopic examination. The smears were fixed with methanol, stained with Giemsa stain for the identification of the yeast form of HCF [20]. Microscopic examination of Giemsa or Gram-stained smears of pus/swabs aspirated from a nodule reveal Gram- positive yeast forms with a halo (unstained capsule-like) structure [23].
Isolation of HCF and Histopathology
The lung tissue sample was taken from a nodular lesion on the lung, it was grinded with pistol and mortar and inoculated aseptically onto slants of Sabouraud‟s Dextrose Agar (SDA, Oxoid) containing chloramphenicol (0.5g/ liter) and enriched with 2.5% glycerol. Incubation was made at 26 0C and 5% CO2 for 8 weeks. The media were checked periodically for the presence of growth of mycelial form of HCF [23]. Primary isolation of the mycelial forms was obtained within 6–8 weeks as white to grayish white, folded, raised cerebriform colonies on SDA. The colonies were adherent to the medium and became brownish on aging. In Haematoxylin and Eosin (H&E) stained histological sections, the appearance of the lesions is quite characteristic that it consists of pyogranulomatous inflammation with fibroplasia. Langerhans giant cells are common [16]. The presence of numerous HCF, some of which show budding, both intra and extracellularly in tissue sections stained with H&E stain is of diagnostic value [18].
Postmortem Lesions: At necropsy, areas of the skin and subcutaneous tissue are thickened, and the skin may be fused to the underlying tissues. The regional lymph nodes may be enlarged and inflamed. Nodules in the skin have a thick, fibrous capsule and the affected lymphatic vessels are usually thickened or distended. Both nodules and lymphatic contain purulent exudates. In some cases, the lesions may extend to the underlying joints, resulting in arthritis, Periarthritis or periostitis. Multiple, small, gray–white nodules or ulcers with raised borders and granulating bases may be apparent on the nasal mucosa, and lesions may be found on the conjunctiva and cornea. The lungs, spleen, liver, testes and other internal organs may also contain nodules and abscesses [3].
5.8.2. Differential Diagnosis: Several infectious diseases can be confused on clinical grounds with epizootic lymphangitis, the most important of which is glanders, especially “farcy” or the skin form of the disease [10]. Differential diagnoses include glanders (farcy), caused by Burkholderia mallei, ulcerative lymphangitis due to Corynebacterium pseudo tuberculosis, sporotrichosis caused by Sporothrix schenckii and the skin lesions of Histoplasmosis caused by H. capsulatum var. capsulatum [16].
Economic impact of Epizootic Lymphangitis
Epizootic lymphangitis is one of the infectious diseases causing huge economic losses and low productivity in horses [7]. It is an economically important disease in some areas of the world, particularly where large numbers of horses, donkeys, or mules are assembled. This disease was a serious concern during the early twentieth century when large numbers of horses were stabled together (www.qldhorsecouncil.com). This disease continues to be a significant concern in some countries such as Ethiopia, where the prevalence in carthorses is nearly 19%and economic losses from this disease are high [3]. The impact of EPL was multi-dimensional and encompassed effects upon the horse, the individual owner and the wider society. Working equids provide a vital utility and source of income to many people in resource-poor settings. Often, infection with EPL resulted in a reduction in working ability which had a direct impact upon the livelihoods of owners and their dependent family members. EPL also impacted upon the welfare of the horse as sick animals continued to be worked and, in advanced cases, horses were abandoned due to ineffective or unavailable treatment [9]. Treatment costs in terms of money and time lost by owners without effective treatment outcomes contribute to the suffering and death of animals. In Ethiopia equines are important animals to the resource-poor communities in rural and urban areas of Ethiopia, providing traction power and transport services at low cost. The use of equines in door-to-door transport service also provides urban dwellers with the opportunity of income generation [24]. In general, the study has shown that EPL greatly affects the economic and social wellbeing of equine owners. Direct effects include reduced income due to lower work capacity or inability to work at all, cost of treatment, loss of customers and the need to purchase new equines. In addition, the owner faces social stigma due to foul smelling [25].
Status of Epizootic Lymphangitis in Ethiopia
Although Epizootic lymphangitis has been eradicated from Europe, it is currently prevalent in Ethiopia, where between 0% and 39% of equids may be infected, with the rate being dependent upon the region [20]. In two separate participatory studies in different areas of Ethiopia, horse owners consistently volunteered EPL as a high-priority disease [9]. EPL contributes to extensive morbidity and subsequent mortality due to abandonment of chronically infected animals and can have a devastating impact on the incomes of poor families [26]. Within regions where the disease is endemic, access to treatment is a significant challenge. The Society for the Protection of Animals Abroad (SPANA) currently provides free veterinary care within its clinics; however, topical treatment with tincture of iodine and oral dosing with potassium iodides are labor intensive, expensive, and of limited efficacy in moderate to severe cases of EPL. It is imperative that animals be diagnosed early during the disease to improve treatment outcomes, conserve resources, and reduce the burden of infection within the population. Currently, due to limited available diagnostic technologies, veterinarians in Ethiopia diagnose the disease based on clinical appearance and microscopic examination for yeast cells within pus.
This has the potential for misdiagnosis, as the clinical appearance can mimic that of other diseases (e.g., ulcerative lymphangitis, sporotrichosis and the cutaneous form of glanders [20]. Culture of H. capsulatum var. farciminosum from clinical lesions would be definitive but is challenging and rarely attempted. Therefore, reliable and robust approaches to diagnosis are required to support clinical decision making and enable epidemiological studies to provide the rationale for the development of disease prevention strategies. EZL has recently been highlighted to be a priority neglected disease of working equids [9]. Epizootic lymphangitis is a common infectious disease of horses in Ethiopia. It is a significant concern in the country, where the prevalence in carthorses is nearly 19%, and economic losses from this disease are high [7]. It is particularly prevalent in carthorses in most parts of Ethiopia studied. For instance, it occurs in 24.9% horses in Woliso [20]. Similarly, studies conducted in Ethiopia in horses showed that EPL is endemic to Ethiopia and its distribution covers humid and hot areas. Epizootic lymphangitis is second only to African Horse Sickness as a most important disease of horses in Ethiopia [27]. The disease primarily occurs in areas with altitudes ranging from 1600 to 2400mm above sea level, which allows the environmental form of HCF to persist for several months. It is common in Ethiopia, especially in cart horses, affecting an average of 18.8% of horses in warm and humid areas [2].
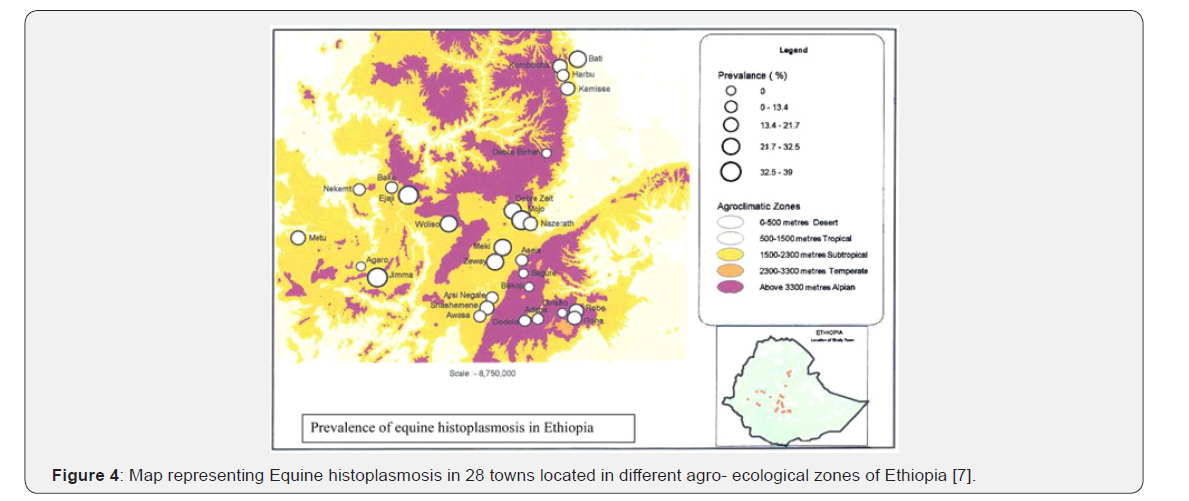
The prevalence of disease accounts for 26.2% in cart horses and 21% in cart mules. Although a few studies have been conducted in western and central Ethiopia there is a lack of information on the epidemiology of EPL in large parts of the country [28]. Recently, an overall prevalence of 18.8% was recorded for EPL in carthorses in 28 Ethiopian towns [27] (Figure 4).
Treatment
Although successful treatment with intravenous administration of sodium iodide, oral administration of potassium iodide and surgical excision of lesions has been reported, there is no completely satisfactory treatment against the disease [29]. Inorganic iodides can be used on early cases and amphotericin B is also recommended as a drug of choice. Both treatment options, however, are not available in the local veterinary service partly because of cost. Even if the drugs are available, early identification of cases is critical for successful therapy. Localized nodules can also be lanced, the pus drained and the nodules packed with a 7% tincture of iodine. In most areas, epizootic lymphangitis is a reportable disease and treatment is not allowed (CFSPH, 2009).
Control and Prevention
The control of epizootic lymphangitis according to the World Organization for Animal Health (OIE) is usually through elimination of infection. This can only be achieved by culling infected equids and applying strict biosecurity measures to prevent spread of the infectious agent [10]. Strict hygienic precautions are essential to prevent spread of epizootic lymphangitis, moreover great care should be taken to prevent spread by grooming or harness equipment, as contaminated bedding should be burned, since the organism may persist in the environment for long time. The disease is eradicated by the humane slaughter of infected horses, disinfection of infected premises and restricting the movement of equids from infected premises [16]. In endemic areas where eradication is not possible, inorganic iodides can be used for therapy in early cases [3]. The methods used to control epizootic lymphangitis in large endemic regions will depend on disease prevalence, methods of husbandry, attitude and the economic capacity of the horse-owning community to bear the costs involved. Cleaning and disinfection will help in preventing the disease from spreading [16].
Conclusion and Recommendations
Epizootic lymphangitis is a debilitating fungal disease seen mainly in equids. The disease results from infection by a dimorphic fungus, Histoplasma capsulatum var. farsiminosum. EPL is endemic in some countries of west, north, and northeast Africa, and Asia where it is mostly diffused in areas characterized by humid and hot climates. The disease is common and has recently been highlighted to be a priority neglected disease of working equids in Ethiopia. The disease can be transmitted by biting flies, e.g. Musca and Stomoxys spp that feed on open, discharging lesions. There are three forms of the disease: cutaneous (skin), ocular, and respiratory forms. The diagnosis of EPL is based on the clinical examination of the lesions, microscopic examination of the yeast form of HCF in pus, serological tests and skin hypersensitivity testing. The impact of EPL was multi-dimensional and encompassed effects upon the horse, the individual owner and the wider society. Intravenous administration of sodium iodide, oral administration of potassium iodide and surgical excision of lesions can be used as a treatment for EPL. Strict hygienic precautions are essential to prevent spread of epizootic lymphangitis moreover great care should be taken to prevent spread by grooming or harness equipment. The disease is eradicated by the humane slaughter of infected horses, disinfection of infected premises and restricting the movement of equids from infected premises [30].
Based on the above conclusion, the following recommendations are forwarded:
a. Owners should be educated on proper use of harness and avoiding any contact of healthy equine with the infected one.
b. In advanced cases equines should be killed in humane way rather than leaving them outdoors since they are source of infection.
c. Low-priced and effective antifungal drugs should be sought to treat the disease which will be readily available to equine owners and drivers both in government and private animal health sectors.
d. The control and prevention of this disease should be the focus of the government.
e. Awareness enhancement education should be provided to equine owners and to the public on importance of early treatment of EPL and preventive measures.






























