Abstract
Autism spectrum disorder (ASD) is a neurological and developmental disorder. Except Difficulty with communication and interaction with other people, restricted interests and repetitive behaviors, Motor behavioural abnormalities are noticed to be presented in children with ASD as well. We conducted clinical observations on scalp acupuncture treatment on 54 children with ASD motor disorders include spinning, toe walking, hand flapping and obsessed with monotonous activities from 2010 to 2013. After 30 times of the treatments, the results showed that the treatment effect was good, and the younger the age, the better the effect.
Keywords:Scalp Acupuncture; Autistic Children; Motor; Disorders
List of Abbreviations
Autism spectrum disorder (ASD) is a developmental disability that 1 in 160 children worldwide is suffering from [1]. Significant social, communication and behavioural challenges could be noticed in ASD patients. Diagnosis of ASD are mainly made by doctor’s observation on child’s behaviour and developmental history. Autism rating scales, for example Autism Behaviour Checklist (ABC), have been used as tools for diagnosis, interventions monitor, and outcome assessment by evaluating the severity of symptoms [2]. Motor behavioural abnormalities are noticed to be presented in children with ASD. Summary of ASD motor functioning has been published previously [3]. Common abnormalities are categorized into five aspects: gross motor coordination, fine motor coordination, motor stereotypies, postural controls and imitation and praxis (Table 1).

No curable treatment for ASD has yet been found. Interventions including behaviour and communication approaches, dietary approaches, medication, and complementary and alternative medicine (CAM) are widely used, aiming to reduce ASD symptoms and improve living skills [4]. Scalp acupuncture, as one of the commonly used CAM interventions, is believed to be beneficial in treating neuro-related diseases in traditional Chinese medicine perspective [5]. By needling acupoints along different scalp lines or zones, it regulates the flow of Qi and blood, adjusting the internal environment of human system. In modern medical terms, scalp acupuncture improves the cerebral blood flow and make adjustment to certain hormone levels [6]. Previous researches have identified the effect of scalp acupuncture on ASD patients, improvements in language function and self-care ability are shown after treatment [7-9]. In comparison to behavioural and educational interventions, scalp acupuncture treatment is reported to be more effective in reducing ASD symptoms [10]. In this study, we would like to identify the therapeutic effect of scalp acupuncture on autistic children’s motor behavioural abnormalities. A pragmatic clinical study was conducted in traditional Chinese medicine outpatient clinical setting, from May 2010 to June 2013 at Hong Kong Baptist University Chinese Medicine Clinic.
Subjects and methods
Participants
Patients diagnosed with ASD who consulted for Chinese medicine acupuncture treatment at Hong Kong Baptist University Chinese Medicine Clinic were invited to participate. Eligibility criteria included children aged 2-11, with medical diagnosis of ASD by recognized healthcare professional. Severity of ASD symptoms had not been set as cut-off exclusion criteria.
Therapist
Dr. Yau Chuen Heung, registered Chinese medicine practitioner in Hong Kong who has 20 years experience in acupuncture treatment of children with mental disorders, carried out all the assessment and treatment.
Treatment
All participants received 30 sessions of standardized scalp acupuncture treatment. Fourteen acupoints, including mid line (MS1) and lateral line 2 of forehead (MS3), SiShenCong (EX-NH3), BaiHui (GV20), lateral line 2 of vertex (MS9), auditory speech area, and primary auditory cortex, were selected. For each session, patient was held in sit position, scalps were first disinfected using 75% alcohol pad. Therapist then insert one 0.20×25mm disposable sterile needle obliquely onto each acupoint subcutaneous place with a 5mm depth, laying in between the loose areolar connective tissue and aponeurosis layer. For every 15 mins, therapist twirls the needles with “Ping Bu Ping Xie” method. All needles were removed, and patients were discharged after one hour.
Measurement of outcome
Participants’ parents/guardian were asked to fill in the Chinese version Autism Behaviour Checklist before and after 30 sessions acupuncture treatment based on the participant’s daily behaviour. In the checklist there were 57 ASD-related symptoms listed, respondents have to determent how often do the patient perform such symptom and rate in a 5-point scale: no symptoms (0 score), minimal symptoms/seldom shown (1 score), mild symptoms/often shown (2 score), moderate symptoms/usually shown (3 score), severe symptoms/always shown(4 score). Data were collected and inputted into excel for further analysis.
To determent the therapeutic effect of scalp acupuncture on autism children’s motor behavioural abnormalities, four motor-behavioural-related items in the checklist were selected for analysis, including item 16 “rushing forward, spinning, toe walking, finger pinching and flicking”, item 22 “hand flapping, swaying, flicking, arm rocking”, item 30 “toe walking”, and item 50 “obsessed with monotonous activities (like walking back and forth, running, bouncing, knocking)”. The therapeutic effects of scalp acupuncture on different ASD-related motor behavioural abnormalities are evaluated by the following equation:
Statistical analysis
All statical tests performed have been using an alpha level of 0.05. Paired t-test are used to analyse the mean and standard deviation of symptoms score changes. All calculations were performed with Microsoft Excel (Windows, version 2108).
Results
Participant characteristics
Data are collected from 54 patients with autism spectrum disorders, 48 are male and 6 are female. Patients began their acupuncture treatment on the age of 2 to 8. The youngest child was 2 years and 1 month old, while the oldest one was 8 years and 8 months old. Participants are grouped according to the age they receive acupuncture treatment. 13 participants belong to the group “2-year-old to 2-year-old and 11 months”, 16 belong to “3-year-old to 3 year-old and 11 months”, 14 belong to “4 year- old to 4-year-old and 11 months”, and 11 belong to “above 5 year-old”.
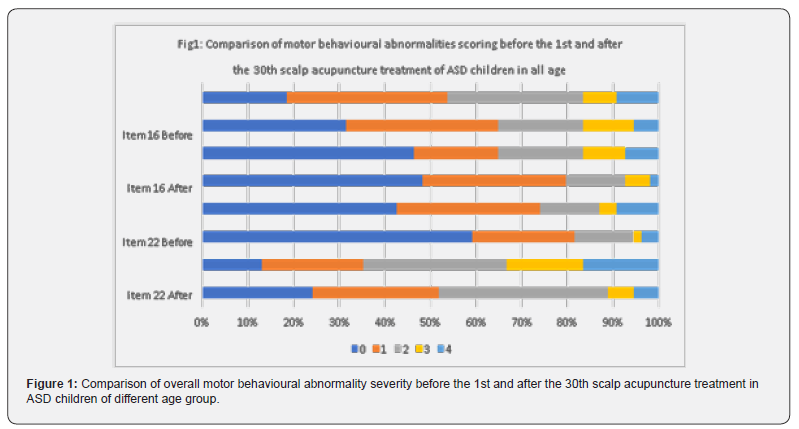
The change of motor behaviour abnormalities severity in ASD children before and after 30 times scalp acupuncture are shown in Table 2 and Figure 1. P-value of all test items are less then 0.05. Before treatment, motor behavioural abnormalities “obsessed with monotonous activities” (item 50) scored the highest, with mean score 2.02. Followed by “rushing forward, spinning, toe walking, finger pinching and flicking” (item 16) and “hand flapping, swaying, flicking, arm rocking” (item 22), scoring 1.54 and 1.13 respectively. A relatively lower mean score 1.06 were found for “toe walking” (item 30). The mean scores of all the four motor behavioural symptoms decreased after the 30th acupuncture. Item 30 obtained the highest effective rate (35.09%) among four. Items 22 and 50 hold an effective rate of 27.87% and 30.28% respectively. A relatively lower effective rate 18.07%, were found for item 16.


The relationship between early treatment and improvement of the overall motor behavioural symptoms is analysed. Samples are grouped according to the age they began treatment, effective rate of treatment of different age group are calculated (Table 3 & Figure 2). P-value of age group “2”, “3” and “5” are less than 0.05. In comparison, we notice that the effective rate decreases with age. Children receive acupuncture treatment at 2-year-old to 2-yearold and 11 months (age group “2”) obtain the highest effective rate (37.62%). Followed by those received treatment at 3-year-old to 3-year-old and 11 months (30.56%). The relatively lower effective rate (23.19%) is obtain for group of children above 5-year-old. The relationship between early treatment and improvement of the four motor behavioural symptoms are analysed separately. Samples are grouped according to the age they began treatment, effective rate of treatment of different age group are calculated (Table 4). Significant therapeutic effects are shown on age group “2”, “3” and “5” on item 30, toe walking. Effective rate of 47.83%, 36.36% and 40.00% are obtained accordingly. Relationship between early treatment and improvement of toe walking symptom is not clearly shown. Therapeutic effect of different age group on tested item 16, 22 and 50 are generally not significantly shown.


Discussion
Motor behavioural abnormalities present in a significant proportion of ASD children. Interventions are suggested to be beneficial to reduce the severity of related symptoms. In this study, we try to identify the therapeutic effect of scalp acupuncture on autism children’s motor behavioural abnormalities. In the first session, we compare the motor symptoms severity in ASD children before and after 30 times scalp acupuncture. Results shown that there is an observable improvement (ER:27.42%) for the overall motor behaviour. In comparison, toe walking is the most improved symptoms, while other analysed motor abnormalities also have a significant improvement. It is strongly believed that scalp acupuncture achieves a therapeutic effect on ASD children’s motor behaviour abnormalities.
In the second session, we identify whether early scalp acupuncture intervention leads to a better therapeutic effect on ASD children’s motor abnormalities. Early interventions on ASD patients have been proved to be outcome favouring in general [11], and early scalp acupuncture intervention were reported to be beneficial on treating commanding speech and social problems [12]. Our study results briefly showed a decreasing trend of scalp acupuncture therapeutic effect on ASD motor abnormalities along patient’s age. Treatment performed on patients aged 2 to 3 obtain the highest therapeutic effect (ER:37.62%), while patients aged 5 or above obtain a relatively lower effect (ER:23.19%).
It suggests that early scalp acupuncture intervention projects a better outcome on treating ASD children’s motor abnormalities, while older patients can still benefit from that. In the third session, we tried to analysed the therapeutic effect of scalp acupuncture on different motor behavioural symptoms on different age group. High therapeutic effects are shown on “toe-walking” across different result-significant age groups, but the relationship between early intervention and treatment effectiveness is missing. Results for other symptoms are generally not significant due to the size of sample, therefore no further relationship is observed.
Therapeutic effect of scalp acupuncture on ASD children has been shown, but its biological mechanism remains unclear. The foundation of scalp acupuncture therapy take reference to traditional Chinese medicine organ-meridian theory and the corresponding underneath cerebral cortex functional locations [13]. It is believed that stimulation of specific scalp acupoint could help adjust the corresponding organ meridian’s Qi and Blood, further regulate the internal environment; stimulation of specific scalp line or zone could excite or inhibit the corresponding brain functional areas, achieving a two-ways regulation effect. Acupoints used in this clinical study are chosen based on reflexology and TCM theory (Table 5). Sishen Chong (EX-NH3) and lateral line 2 of vertex (MS9) appears to be possibly related to the therapeutic effect of scalp acupuncture on ASD children motor behavioural abnormalities.
Previous study suggested that scalp acupuncture produce clinical effect through the trigeminal nerve-meningescerebrospinal fluid-contacting neurons-brain pathway [14]. Another study reported a close connection between scalp acupuncture, trigeminal sensory pathway and reticular formation locus coeruleus and dorsal raphe nucleus, suggesting a biological mechanism on how scalp acupuncture regulate emotion and sensation [15]. Further animal model experiments are suggested to be done to identify the connection between scalp acupuncture and motor control. Limitations exist in the study. First, 54 participants are recruited for treatment, the small sample size may lead to insignificant results. Second, confounding exists as patients may undergo other ASD- related interventions while participating in the study. Importing a matched control group may be able to give a more comprehensive analysis..
Conclusion
This study focuses on observing the therapeutic effect of Scalp Acupuncture on Autistic Children’s Motor Behavioural Disorders. The outcomes of the treatment are good. This improvement of the symptoms may be related to scalp acupuncture improving the neurological function of the brain. The mechanism of action still needs further study.
References
- World Health Organization (2021) autism spectrum disorders: Fact Sheet.
- Bravo Oro A, Navarro-Calvillo ME, Esmer C (2014) Autistic Behavior Checklist (ABC) and Its Applications. Comprehensive Guide to Autism. Springer, New York, NY pp: 2787-2798.
- Bhat AN, Landa RJ, Galloway JC (2011) Current Perspectives on Motor Functioning in Infants, Children, and Adults with Autism Spectrum Disorders. Physical Therapy 91(7): 1116-1129.
- Centers For Disease Control and Prevention (2021) autism spectrum disorders: Treatment.
- Shoukang L (1991) Scalp acupuncture therapy and its clinical application. J Trad Chinese Med 11(4): 272-280.
- Xiang L, Wang H, Li Z (1996) TCD observation on cerebral blood flow dynamics: inference of cerebral palsy with scalp therapy [in Chinese]. Zhen Ci Yan Jiu 21(4): 7-9.
- Allam H, Eldine NG, Helmy G (2008) Scalp acupuncture effect on language development in children with autism: a pilot study. J Altern Complement Med 14(2): 109-114.
- Liu Z (2012) 1523 Scalp Acupuncture Therapy of Children with Autism. Archives of Disease in Childhood 97(Suppl 2): A431-A432.
- Wong VC, Chen WX, Liu WL (2010) Randomized controlled trial of electro-acupuncture for autism spectrum disorder. Altern Med Rev 15(2): 136-146.
- Liu C, Li T, Wang Z, Zhou R, Zhuang L (2019) Scalp acupuncture treatment for children's autism spectrum disorders: A systematic review and meta-analysis. Medicine (Baltimore) 98(13): E14880.
- Corsello C (2005) Early Intervention in Autism. Infants and Young Children 18(2): 74-85.
- Yau C, I, C, Chau Y (2018) The therapeutic effect of scalp acupuncture on natal autism and regressive autism. Chinese Medicine 13(1): 30.
- Wang H (2012) Zen Jiu Xie (9th ed.). Beijing: China Press of Traditional Chinese Medicine.
- Wang S, Liu K, Wang Y, Wang S, He X, Cui X, et al. (2017) A Proposed Neurologic Pathway for Scalp Acupuncture: Trigeminal Nerve-Meninges–Cerebrospinal Fluid–Contacting Neurons–Brain. Medical Acupuncture 29(5): 322-326.
- Zhang, Z, Wang X, McAlonan G (2012) Neural Acupuncture Unit: A New Concept for Interpreting Effects and Mechanisms of Acupuncture. Evidence-based Complementary and Alternative Medicine 2012: 429412-23.






























