Role of Ayurvedic Herbs and Panchakarma Procedures in the Management of Cerebral Palsy
Dosani Minaj Nadirbhai1, Prem Prakash Vyas2 and Harish Kumar Singhal3*
1PG Scholar, Department of Ayurveda Pediatrics, India
2Dean Research and Head, Postgraduate Institute of Ayurveda, India
3Associate Professor, Dr. S. R. Rajasthan Ayurved University, India
Submission: April 17, 2023; Published: May 03, 2023
*Corresponding author: Harish Kumar Singhal, Associate Professor, Dr. S. R. Rajasthan Ayurved University, India
How to cite this article: Dosani Minaj N, Prem Prakash V, Harish Kumar S. Role of Ayurvedic Herbs and Panchakarma Procedures in the Management of Cerebral Palsy. J Complement Med Alt Healthcare. 2023; 12(1): 555826.DOI: 10.19080/JCMAH.2023.12.555826
Abstract
Cerebral palsy is a common chronic motor disability prevalent among pediatric population. It describes a group of permanent disorders of movement and posture causing activity limitation that attributed to non-progressive disturbances of sensation, perception, cognition, communication, and behavior as well as by epilepsy and secondary musculoskeletal problems. Cerebral palsy is not a contagious disease. At present treatment modalities are either very costly or employ very complicated procedures like baclofen pump implantation, botulinum toxin injection, selective posterior rhizotomy which have their own limitations. Recent studies prove that Ayurvedic treatment modality through its principals can repair damaged neurons and stimulation for forming new synapses for better functional recovery in Cerebral palsy affected children. This paper review number of research on certain herbs and Panchkarma procedures that found very effective in the management of cerebral palsy.
Keywords: Ayurveda; Basti, Cerebral Palsy; Herbs, Nasya; Panchkarma; Shastik Shali Pinda Swedana
Introduction
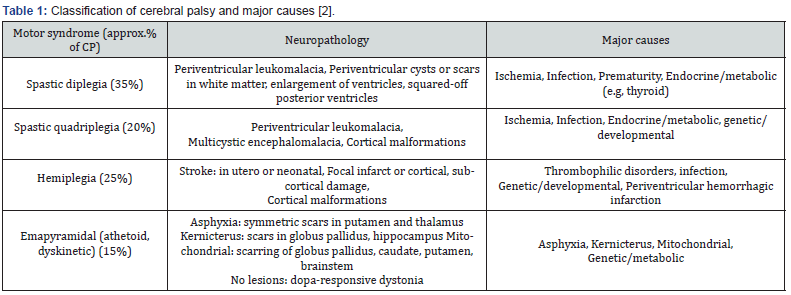
Cerebral palsy is an umbrella term that describes a group of disorders caused by damage to the brain. It describes a group of permanent disorders of movement and posture causing activity limitation that attributed to non-progressive disturbances of sensation, perception, cognition, communication, and behavior as well as by epilepsy and secondary musculoskeletal problems. Cerebral palsy is not a contagious disease. Cerebral Palsy (CP) is the leading cause of chronic disability in children, making them not only physically or mentally handicapped but also making them socially apart. The whole brain is not damaged, only parts of it, mainly parts that control movements. The movements, body positions and related problems can be improved or made worse depending on the treatment [1]. The data indicates that the incidence of CP is 3.6 per 1000 children with a male to female ratio is 1.4:1 [2]. The cerebral palsy being predominantly motor disorder, is often accompanied by other areas of problem like mental retardation- 50-70 % most often in quadriplegia and ataxia CP. Seizures 25-33 % often in spastic hemiplegia & quadriplegia, least in dyskinetic CP. Hearing & speech defects 15-20% common in dyskinetic and quadriplegic CP. Ocular defects 50-70 %, Behavioral problems (Hyperkinetic behavior, aggressiveness, lack of attention) 30-50 % [1]. The major lesions that contribute to CP in preterm infants are intracerebral hemorrhage and periventricular leukomalacia (PVL). There are four types of cerebral palsy - Spastic diplegic (35%) in which muscle stiffness mainly in the legs with the arms less affected or not affected at all. Spastic quadriplegic (20%) is a most severe type of CP that affects both arms and legs and often the torso and face, hemiplegia (25%) in which paralysis on one side of the body and extrapyramidal(15%) in which injury is outside the tract in areas such as the basal ganglia, thalamus and cerebellum and its key component to movement impairment. In general, these four types relate to the part of the brain that has been damaged or affected. The effects of cerebral palsy vary enormously from one person to another, with some people experiencing a combination of two or more types [2].
There is no single disease in Ayurveda that shows exactly similarity with CP. Some conditions explained in Ayurveda, which have shown some similarity with CP are Phakka (A kind of nutritional disorder), Pangulya (locomotor disorders), Mukatva (dumbness), Jadatva (mental disorders), EkangaRoga (monoplegia), Sarvangaroga (quadriplegia), Pakshaghata (hemiparesis) and Pakshavadha (hemiplegia) etc., Vatavyadhi’s (neurological disorders). Spastic CP can be considered as ‘Avarana Janya Vata Vyadhi-Kaphavrita Vata’. As Vata Vyadhi is the most similar condition to CP [3].
Materials and Methods
Materials for present manuscript collected from ancient classics of Ayurveda like Charaka Samhita, Sushruta Samhita, Astanga Sangraha, Astanga Hridaya, Kashyapa Samhita, Harita Samhita, Ayurved Pharmacopeia of India (API) and Ayurved Formulatory of India (AFI) along with modern textbooks like OP Ghai, Nelson Textbook of Pediatrics, etc (Table 1).
To explore the neuroprotective activity, nootropic activity, anticonvulsant activity, neuro-regernative activity, analgesic activity of various Ayurveda Herbs and utilization of various Panchkarma procedures in the management of cerebral palsy various search engines like Ayush research portal, PubMed, Medlar, Open Med, In Med, Scopus, Google Scholar were studied from 1960 to till date.
Neuroprotective Activity
Saponins are the main active constituents of extract of Bacopa monnieri which are responsible for its pharmacological actions like nootropic, neuroprotective etc. [4-7]. In an pilot clinical study, it was proved that Bacopa monnieri improve the scores of PWBI (greater wellbeing of the patient), Barthels index (improvement in daily living activities) and significant increase in the scores of positive and negative affect schedules (PANAS) after an intervention of 4 weeks [8].
Studies have shown that W. somnifera extracts exhibit numerous therapeutic effects including inflammation and oxidative stress reduction, memory and cognitive function improvement [9].
During a study, when aqueous extract of the roots of Glycyrrhiza glabra Linn administer to nitrite water induced hypoxic rats then it shows that extract administration Glycyrrhiza glabra Linn. (yashthimadhu) restored the decreased levels of brain enzymes such as glutamate and dopamine and decreased acetylcholinesterase (AChE) activity. Levels of antioxidant enzymes such as superoxide dismutase, glutathione peroxidase etc. were reduced due to hypoxia and were restored by administration of ethanol extract of G. Glabra [10]. Neuroprotective effect of Nardotachys jatamansi (Jatamansi) was studied on middle cerebral artery [MCA] occlusion rat model in which thiobarbituric acid reactive substance [TBARS], thiol group, catalase and sodium potassium-ATPase activities were studied. The activities of Na [+] K [+] ATPase and catalase declined significantly by MCA occlusion. The neuro behavioral activities like spontaneous motor activity also decreased significantly in MCA occlusion group [11].
In chronic foot-shock stressed rat model study Pueraria tuberosa (Roxb. ex Willd.) DC(Vidarikanda) plant showed neuroprotective action. These findings suggest significant anxiolytic and anti-stress properties of PTE. [12]. The study conducted on male rates, through Y maze and shuttle box tests models to evaluate the neuroprotective activity of Acorus calamus (Vacha). The result shows that there is enhancement of memory power [13]. The ethanolic A. calamus rhizome extract (0.5 mL/ kg, i.p.) potentiated pentobarbitone-created sleep periods, which provides marked (40–60%) protection against PTZ-induced convulsion [14]. Emblica officinalis (Amalaki) depletes iNOS and COX-2 levels by inhibiting NF-κB activation thus reduction of elevated expression level of Bax is there [15].
Nootropic Activity
C. prostratus (CP) (Shankhpushpi) contains volatile oil; fatty alcohols; flavonoids, i.e. kaempferol; hydroxy cinnamic acid; β-sitosterol; and carbohydrates s., which possess nootropic activity of this plant. An alkaloid convolvine, which is found in this plant, also blocks the cholinergic muscarinic receptors. Convolvine also aids in potentiating the effect of arecoline, thereby imparting nootropic abilities to CP [16]. The pilot study was conducted by using elevated plus maze (EPM) and stepdown models in mice to evaluate nootropic activity of CP. Results shows that the aquomethanolic, ethanolic and petroleum ether extracts isolated from CP are responsible for nootropic activity [17]. An experimental study was conducted using subjects like high plus maze where methanol extract of Celastrus paniculatus (Jyotishmati) whole plant administered to rats which shows significant Nootropic activity. It improved the learning and memory of rats [18].
In a study the elevated plus maze and the passive avoidance paradigm was used to evaluate nootropic activity of Nardotachys jatamansi (Jatamansi). An ethanolic extract of N. jatamansi administered for seven successive days to both young and aged mice. It significantly improved learning and memory in young mice and reversed the amnesia induced by diazepam and scopolamine [19,20].
Alcoholic and aqueous extracts of P. tuberosa (Vidarikanda) tuber were studied for nootropic effect in mice and rat models of amnesia induced by scopolamine and diazepam. The inflexion ratio observed was considerably high and comparable with piracetam, the standard drug in an elevated plus-maze experiment. Flavonoids present in the P. tuberosa (Vidarikanda) tuber extracts have been reported for nootropic effect by interacting with cholinergic, adrenergic, serotonergic, and GAB Anergic system [21]. The study was carried out for nootropic activity of Asparagus racemosus (Shatavari), Methanolic extract of A. racemosus roots (MAR) showed nootropic activities in the mice models which inhibited acetylcholinesterase enzyme in prefrontal cortex, hippocampus and hypothalamus and these effects may probably be mediated through augmentation of cholinergic system due to its anti-cholinesterase activity [22].
Anti-Convulsant Activity
Ethanolic extract of the roots of Nardotachys jatamansi (Jatamansi) studied for its anticonvulsant activity that shows significant threshold by N. jatamansi root extract against maximal electroshock seizure in rat model as indicated by a decrease in the extension/flexion ratio. The administration of phenytoin with N. jatamansi root extract resulted in a significant increase in the protective index of phenytoin from 3.62 to 13.17 [23].
During another study, alcoholic tuber extract of Pueraria tuberosa (Roxb. ex Willd.) shows anticonvulsant activity in pentalene tetrazole, strychnine, and maximal electroshock-induced convulsions in animals. Different doses of the extract were compared with the standard drug, diazepam. The medium and high doses show significant anticonvulsant activity as compared to the control group [24].
An experimental study was carried out where aqueous extract Glycerrhiza Glabra (Yastimadhu) extract, diazepam and normal saline were injected intraperitoneal 30 min before pentylenetetrazole in mice. Aqueous extract of G. Glabra root delayed the onset time of the seizure and decreased the duration of the seizure significantly compared to the control group [25].
In a study the methanol extract of Acorus calamus (Vacha) shows anticonvulsant effect through potentiating action of gammaaminobutyric acid (GABA) pathway and by decreasing the span of the tonic extensor period in rats [26]. The purified rhizome was investigated in a maximal electroshock (MES) seizure model, and phenytoin was used as the standard drug. The processed rhizome provides significant anticonvulsant activity by minimizing the span of the tonic extensor period in rats [27].
Neuroregenerative Activity
The experimental study has been done to evaluate the effect of ethanol extract of B. monnieri (Brahmi) (EBm) on cold stress induced neurodegeneration in hippocampus of rats. Histologically, rat brains were divided into 4 groups viz- group 1 consisted of rats which were kept in ideal laboratory conditions, group 2 rats were given EBm in the dose 40 mg/kg, group 3 rats were forced to swim in the cold water for 1 month which generated cold water swim stress in their body, and group 4 were given cold water swim stress for 1 month which was followed by treatment by EBm for about 1 month in the dose of 40 mg/kg. The histopathological study shows that Group 3 cells showed decreased diameter of cells, number of cells per square, and packing density of cells that was indicative of stress-induced damage while group 4 cells showed increased cell diameter, number of cells per square, and cell packing density. Group 4 rats showed the above parameters comparable to that of group 1 rats [28]. This study demonstrated that EBm has got important therapeutic effect in abolishing stressinduced hippocampal damage.
In a 21-day randomized, double blind placebo-controlled study, the pure aqueous extract of the T. cordifolia. (Guduchi) root was found to enhance verbal learning and logical memory [29]. The study was conducted to evaluate neuro-regenerative capacity of Centella asiatica (Mandukparni) using an in vitro experimental model revealed the ability of asiatic acid (AA) to promote the elongation of neuritis [30] in Neonatal rat pups. They were administered with 2-, 4- or 6-ml kg−1 body weight of fresh leaf extract of CeA for 2, 4 or 6 weeks. After the treatment period over the rats killed, their brains were removed. The hippocampal neurons were impregnated with silver nitrate. This study reported that fresh C. asiatica leaf extract significantly increases the dendritic arborisation of hippocampal CA3 neurons in vivo [31].
Anti Spasmodic
The experimental study was conducted to evaluate the antispasmodic activity of guggul on ileum of guinea pig and Wistar rats. The animals were sacrificed, and ileum tissue of guinea pig and rat was isolated and tested for antispasmodic activity using different spasmogens like acetylcholine, histamine, and barium chloride. processed Commiphora mukul (guggul) inhibited the spasms induced by these spasmogens by inhibiting acetylcholine [32]. In a study B. monnieri extract shows spasmolytic activity in smooth muscles due to inhibition of calcium influx [33].
Analgesic Activity
Withania-Somnifera (Ashwagandha) produced significant analgesic activity for a rat experiencing heat analgesia induced by hot plate method. The analgesic activity of Ashwagandha was potentiated significantly by cyproheptadine, however, paracetamol failed to exhibit any significant change in its activity, suggesting the involvement of serotonin, but not prostaglandins in the analgesic activity of Ashwagandha [34].
Analgesic activity of ethanol extract of A. racemosus (Shatavari) (EEAR) was tested using acetic acid induced writhing model in mice. The extract produced 52.39% (p<0.05) and 67.47% (p<0.01) writhing inhibition in test mice at the dose of 250 mg kg-1 and 500 mg kg-1 body weight which were comparable to the standard drug diclofenac sodium showing 70.65% (p<0.01) writhing inhibition at the dose of 25 mg/kg body weight which shows analgesic effect of A. racemosus [35].
Analgesic activity and potentiation of morphine analgesia were tasted in albino rats by using a hot-wire “techno analgesiometer. The study shows that a mild analgesic effect of T. cordifolia (Guduchi) is due to promising effect of morphine analgesia [36]. In a pilot, study Celastrus paniculatus (Jyotishmati) showed analgesic activity on using hot water tail immersion test in mice and carrageenan pedal edema in rats [37].
Panchkarma Procedures
Panchkarma procedures commonly used and found effective in management of cerebral palsy are Udwartana, Sarvaanga Abhayanga, Shahstishali Pinda Swedana, Naadi Swedana, Baasp Swedana, Parisheka Swedana, Nasya and Basti [38].
Abhyanga
Abhyanga is used as a synonym for oil bath. Abhyanga (massage) acts on muscles and makes them strong. It may thus nourish the superficial and deep muscles and make the muscles strong and joints stable [39]. Prasarini oil, Mahanarayan oil, Mahamasha oil, Ksheerbala oil, Ashwagandha oil having properties like analgesic, anti-inflammatory, anti-spasmodic and stimulatory etc. that found effective to relive spasticity in the external or internal oleation of cerebral palsy affected patient. In a study treatment of cerebral palsy with using of Udwartan with Pinyak, Sarvang Abhyang with Ksheerbala Oil, Nadi Swedana with Vatahara Patra Kwath, Matrabasti with Kshirbala Taila and oral administration of Abhya Ghrita gives significant improvement on gross motor functional scale (78.03%) and17.49% on quality-oflife scale [40].
Swedana
Swedana (sweating/diaphoresis/sudation) is a prerequisite for all Shamana courses, and it provides temporary and lasting relief in many disorders. Many types of Swedana are explained; among them ‘Baashpa sweda’ or ‘Ooshma sweda’ (steam bath) and ‘Naadi sweda’ (tube sweating) are commonly used. In Baashpa Swedana, the patient may be exposed to steam. Sweating produced through fluid that may contain many herbs or other liquids such as Dhanyamla (an alcoholic beverage prepared from grains) or wine or milk etc. in Baashpa Swedana. In Nadi Swedana a pressure cooker (which should be filled with liquids and herbs) is used and the patient is exposed to steam coming out of the spout or a tube which is fitted to a narrow-mouthed pressure cooker over the required body part [41]. Sudation causes excretion of waste metabolites through diaphoresis. Swedana is Mardavtvkar (relieves spasticity), Sandhichestakar (improves joint mobility), Srotonirmaltvakar (cleanses channels) and Kaphavatanirodhaka (pacifies Kapha and Vata) [42].
Shashtik Shali Pinda Swedan
Inducing perspiration by using heated round Pinda (bolus) of special rice i.e., Shashtika Shali prepared in milk and processed with herbal decoction referred as Shashtika Shali Pinda Swedana. This belongs to the category of Agni Swedan as well as Snigdha Swedan. A Pinda (bolus) tied in bolus to rub against the whole body or afflicted part of the body to provide heat, nutrition and strength to the pain afflicted joints, muscles, or body parts [43].
The clinical study was carried out for the management of cerebral palsy with Shashtika Shali Pinda Swedana and Samvardhana Ghrita. The study was carried out in 16 patients, 8 in each group, namely group A (Shashtika Shali Pinda Swedan externally and Samvardhana Ghrita internally) and group B (Samvardhana Ghrita internally) for 35 days duration. Group A showed better results in improving motor system skills by improving muscle power and reducing hypertonia and tendon reflexes [44].
Parisheka Swedan
Stream pouring or sprinkling or showering of warm Kwatha (decoction or herbal extract) prepared with herbs which destroy or pacify Vata or Vata-Kapha morbidity over the body is called Parisheka [45]. The clinical trial was conducted Parisheka- Upanaha (PU) Group: 38 subjects were treated with Abyanga with Tila Taila and Dashamoola Parisheka followed by Salavana Upanaha sweda. Control Group- 37 subjects were treated with Abyanga with tila taila and Ushnajala snana followed by Salavana Upanaha swedan. Results: Both the groups showed effect in reducing spasticity on objective and subjective parameters at the level of p < 0.05 but better result was seen in Upanaha along with Parisheka group when compared to the Upanaha alone group [46].
Basti
Basti is the most important among the Panchkarma in the treatment of CP. No other treatment has the capacity to pacify and regulate the force of Vata apart from Basti. Improvement in muscle bulk, power, tone and developmental milestone with Anuvasana Basti [47]. A clinical study reveals that Mustadi Rajayapana Basti along with Baladi Yoga provided mild improvement in 93.44% patients CP with the outcome measures being mental status, fine and gross motor functions, and daily life activities [48].
Nasya
Nasya is the process of administration of medicines through nostrils [49]. Nasya has a definite role in treatment of CP because it is said to be beneficial in various Shiro Roga’s (diseases of head/brain) [50] Commonly used medicines for Nasya are Panchendriyavardhan Tailam, Dhanvantaram Tailam, Anu Tailam, Shadbindu Tailam and Shunthi Churna (powder of Zingiber officinale) for Pradhamana Nashya (nasal administration of herbal powders. Pratimarsa Nasya (nasya of small dose/nasya used for daily purpose) may have beneficial effects in patients of CP as it provides strength to Shira (head) and Shirogata Indriyas (sense organ in head) as it can be used as Snehana(oleation) as well as Shodhan (curative) [51]. A clinical study was carried out where nasya with Ashtamangal Ghrita was given to the patients of the cerebral palsy that shows significant improvement in head holding, sitting, standing, fine motor milestones, mental status, language and overall performance [52].
Discussion
There is not any exact reference available in Ayurvedic texts for cerebral palsy. However, considering the Ayurvedic disease classification and their sign and symptoms, Cerebral palsy can be compared with Vatavyadhi or Vatavikar diseases of the nervous system) which specifically afflict the Shiro-Marma which may be noticeable in various clinical forms as Pakshaghat, Ekangaroga, Pangu, Sarvangroga, Aakshepka etc. However, it is not curable, but with Ayurvedic treatment there is overall improvement in the quality of life with better life expectancy. T. cordifolia, B. monnieri, C. prostratus used as a Rasayana to improve the immune system and body resistance against infections [53]. The regenerative tonic property of W. somnifera is due to its multiple pharmacological actions like anti-stress, neuroprotective, analgesic, and antiinflammatory etc. [54]. Methanolic extract of C. prostratus plant also exhibited anti-convulsant activity, as characterized by reduction in the mean recovery time of convulsions therefore it can be use in patient in cerebral palsy associated with convulsion [55]. B. monnieri causing a faster functional recovery of muscle action potential in response to neuromuscular stimulation [8]. Emblica officinalis is one of the most potent and nutritious drugs which causes nourishment of the body [56]. W. somnifera is a well-known Ayurvedic Rasayana and belongs to a sub-group of Rasayanas known as Medhya Rasayanas which not only nourishes brain but also increase mental/intellectual capacity [57]. A clinical study was carried out on 184 patients herbal composite was given which was constituting equal part (100mg) of Acorus calamus Herpestis monnieri, Cassia angustifolia, Nardostacachys jatamansi and Convolvulus pluricaulis in each 5ml in dose. The results show that there was marked improvement in motor power, muscle tone, mental capability and intelligent quotient (IQ) in 96.7% cases [58,59].
After analyzing the mode of action of various Panchakarma procedures it has been clear that Panchakarma along with internal medications has significant role in the management of CP. Vata has been explained to be vitiated by trauma (Abhighata) and injury to vital organ (Marmabhighata) [60,61]. Abhyanga and Shastikashali Pinda Sveda causes muscle relaxation by soothing sensory nerve endings. They produce a hyperemic effect causing the arterioles to dilate limbs and make the body strong with well-developed musculature. Abhyanga causes movements of the muscles, thereby accelerating the blood supply, which in turn helps in relieving the muscular fatigue and reduces stiffness [48]. According to modern science, Basti (trans rectal route); the rectum has a rich blood and lymph supply and drugs can cross the rectal mucosa like other lipid membrane and by entering general circulation, it acts on whole body. Basti may block neuromuscular transmission by binding to acceptor sites on motor or sympathetic nerve terminals, entering the nerve terminals, and inhibiting the release of acetylcholine [61].
The medicine that is put into the nostril moves up to the Sringataka Marma and spreads to the interior of the head and the junctions where all the channels related to eye, ear, and nose are situated together. The olfactory nerves of the nose relate to the higher centers of brain i.e., limbic system that include amygdaloidal complex, hypothalamus, and basal ganglia etc. Thus, drugs administered to nostrils directly goes to higher centers the brain and affects nervous system and endocrine system by controlling doshas [62,63].
Conclusion
It concluded that disabilities in cerebral palsy affected patients can be prevented and maximum movement of the affected part can be achieved if Ayurvedic treatment modality is incorporated with physiotherapy in early intervening period along with Panchakarma procedures. In this way, Ayurveda provides an effective, untoward free and cheaper treatment option for cerebral palsy affected children.
References
- Parthasarathy A (2013) IAP Textbooks of Pediatrics, 5th edition, New Delhi, Jaypee Brothers Medical Publishers (P) Ltd. 407-408.
- Robert M Kliegman, Joseph St (2020) Nelson textbook of pediatrics,21st edition, Geme Philadelphia, Elsevier 3168
- Rathia S, Kori VK, Rajagopala S, (2015) A clinical study to assess the effect of samvardhana ghrita and yoga basti in cerebral palsy. Pharma Science Monitor 6(4): 108-117.
- Chopra RN, Nayar L, Chopra IC (2007) Glossary of Indian Medicinal Plants. Council of Scientific and Industrial Research, New Delhi 32: 1956-1992.
- Chatterji N, Rastogi RP, Dhar ML (1959) Chemical examination of Bacopa monneri Wettst.: parti-isolation of chemical constituents. Indian J Chem 3: 24-29.
- Shastri MS, Dhalla NS, Malhotra CL (1959) Chemical investigation of Herpestis monneri Linn (Brahmi). Indian J Pharmacol 21: 303-304.
- Russo A, Borrelli F (2005) Bacopa monniera, A reputed nootropic plant: An overview. Phytomedicine 12: 305-317.
- Ramakrishnan K.S, Sathya, Sajgotra E (2017) Efficacy of Brahmi in Cognitive Function - A Comparison Between Cerebral Palsy Children and C.V.A Patients, International Journal of Innovative Research in Science, Engineering and Technology 6(4): 6945-6952.
- Wongtrakul J, Thongtan T, Kumrapich B, Saisawang C, Ketterman AJ (2021) Neuroprotective effects of Withania somnifera in the SH-SY5Y Parkinson cell model. Heliyon 7(10): e08172.
- Muralidharan P, Balamurugan G, Babu V (2009) Cerebroprotective Effect of Glycyrrhiza Glabra Linn. Root Extract”. Bangladesh Journal of Pharmacology 4 (1): 60-64.
- Salim S, Ahmad M, Zafar KS, Ahmad AS, Islam F (2003) Protective effect of Nardostachys jatamansi in rat cerebral ischemia. Pharmacol Biochem Behav 74(2): 481-486.
- Pramanik SS, Sur TK, Debnath PK, Bhattacharyya D (2010) Effect of Pueraria tuberosa tuber extract on chronic foot shock stress in Wistar rats. Nepal Med Coll J 12(4): 234-238.
- Naderi G, Khalili M, Karimi M, Soltani M (2010) The Effect of Oral and Intraperitoneal Administration of Acorus calamus L. Extract on Learning and Memory in Male Rats. J. Med. Plants 9 (34) :46-56
- Vohora SB, Shah SA, Dandiya PC (1990) Central nervous system studies an ethanol extract of Acorus calamus rhizomes. J Ethnopharmacol 28(1): 53-62.
- Sankaran M, Velusamy V, Mani K, Amla (2013): A novel ayurvedic herb as a functional food for health benefits”- A mini review, International Journal of Pharmacy and Pharmaceutical Sci 5(1):1-4.
- Sethiya NK, Nahata A, Mishra SH, Dixit VK (2009) An update on Shankhpushpi, a cognition boosting Ayurvedic medicine. J. Chin. Integr. Med 7(11): 1001-1022.
- Rawat MSM, Kothiyal P (2011) Comparative nootropic effect of Evolvulus alsinoides and Convolvulus pluricaulis. Int J Pharma Bio Sci 2: 616-621.
- Sudha PGH, Shashidhar CH, Sridevi VJ, Suthakaran R (2009) Anti-inflammatory activity of Celastrus paniculatus seeds. Int J Pharmtech Res 1(4): 1326-1329.
- Bhattacharyya SK, Bhattacharyya D (1982) Effect of restraint stress on rat brain serotonin. J Bio sci 4: 269-274.
- Joshi H, Parle M (2006) Nardostachys jatamansi improves learning and memory in mice. J Med Food 9(1): 113-118.
- Rao NV, Pujar B, Nimbal SK, Shantakumar SM, Satyanarayana S (2008) Nootropic activity of tuber extract of Pueraria tuberosa (Roxb). Indian J Exp Biol 46(8): 591-598.
- Ojha R, Sahu AN, Muruganandam AV, Singh GK, Krishnamurthy S (2010) Asparagus recemosus enhances memory and protects against amnesia in rodent models. Brain Cogn 74(1): 1-9.
- Rao VS, Rao A, Karanth KS (2005) Anticonvulsant and neurotoxicity profile of Nardostachys jatamansi in rats. J Ethnopharmacol. 102(3): 351-356.
- Basavaraj P., Shivakumar B., Shivakumar H (2011) Evaluation of anticonvulsant activity of alcoholic extract of tubers of Pueraria tuberosa (Roxb). Adv. in Pharm. and Toxicol 12(1): 1-9.
- Nassiri-Asl M, Saroukhani S, Zamansoltani F (2007) Anticonvulsant Effects of Aqueous Extract of Glycyrrhiza glabra Root in PTZ-Induced Seizure in Mice. International Journal of Pharmacology 3: 432-434.
- Jayaraman R, Anitha T, Joshi VD (2010) Analgesic and anticonvulsant effects of Acorus calamus roots in mice. Int J Pharm Tech Res 2: 552-555.
- Bhat SD, Ashok BK, Acharya RN, Ravishankar B (2012) Anticonvulsant activity of raw and classically processed Vacha (Acorus calamus Linn.) rhizomes. Ayu 33(1): 119-122.
- Kumar SS, Saraswathi P, Vijayaraghavan R (2015) Effect of bacopa monniera on cold stress induced neurodegeneration in hippocampus of wistar rats: a histomorphometric study. J Clin Diagn Res 9(1): AF05-AF07.
- Bairy KL, Rao Y, Kumar KB (2004) Efficacy of Tinospora cordifolia on learning and memory in healthy volunteers: A double blind, randomized, placebo-controlled study. Iranian J Pharmacol Therapy 3: 57-60.
- Soumyanath A, Zhong YP, Gold SA, Yu X, Koop DR, et al. (2005) Centella asiatica accelerates nerve regeneration upon oral administration and contains multiple active fractions increasing neurite elongation in-vitro. J Pharm Pharmacol. 57(9): 1221-1229.
- Mohandas Rao KG, Muddanna Rao S, Gurumadhva Rao S (2006) Centella asiatica (L.) leaf extract treatment during the growth spurt period enhances hippocampal CA3 neuronal dendritic arborization in rats. Evid Based Complement Alternat Med 3(3): 349-357.
- Kamble R, Sathaye S, Shah DP (2008) Evaluation of antispasmodic activity of different Shodhit guggul using different shodhan process. Indian J Pharm Sci 70(3): 368-372.
- Ganguly DK, Malhotra CL (1967) Some behavioural effects of an active fraction from Herpestis monniera, Linn. (Brahmi). Ind J Med 55: 473-482.
- Sakka Mazen E, Pavelescu M, Grigorescu E (1990) Contributions to the pharmacodynamic study of roots of Withania somnifera Dun species of Pakistani origin. Note III: Testing of analgesic activity of dichlormethanic and methanolic extract from Withania somnifera roots. Rev Med Chir Soc Med Nat Iasi 94(3-4): 603-605.
- Karmakar UK, Sadhu SK, Biswas SK, Chowdhury A, Shill MC, et al. (2012) Cytotoxicity, analgesic and antidiarrhoeal activities of Asparagus racemosus. J Appl Sci 12(6): 581-586.
- Pendse VK, Dadhich AP, Mathur PN, Bal MS, Madam BR (1977) Anti-Inflammatory, immunosuppressive and some related pharmacological actions of the water extract of Neem Giloe (Tinospora cordifolia): A Preliminary Report. Indian J Pharmacol 9: 221-224.
- Ahmad F, Khan RA, Rasheed S (1994) Preliminary screening of methanolic extracts of Celastrus paniculatus and Tecomella undulata for analgesic and anti-inflammatory activities. J Ethnopharmacol 42(3): 193-198.
- Mamidi P, Gupta K (2015) Ayurvedic management of cerebral palsy: Report of two cases with review of literature. Int Res J Pharm 6(1): 73-76.
- Mamidi P, Gupta K (2018) Some efficacious Ayurvedic panchakarma procedures in children with cerebral palsy, Int J Complement Alt Med 11(1): 37-42.
- Sonam, Mahapatra AK, Rajagopala S (2019) Clinical response of Abhaya Ghrita and procedure-based therapy on Gross Motor Functions in children with Cerebral Palsy: An Open Label, Randomized Clinical Trial, Journal of Ayurveda and Integrated Medical Sciences 4 (4).
- Varier PS (2002) Chikitsa Samgraham. Swedanam chapter. 6th ed. Kottakkal: Kottakkal Ayurveda Series 2, India 188-194.
- Shastri KA (2017) Susruta Samhita, chikitsasthan, Chaukhambha Sanskrit sansthan, Varanasi 1: 175.
- Shukla V, Tripathi RD (2017) Caraka Samhita, volume 1, Sutrasthan, Chaukhambha Sanskrit Pratishthan, Delhi 219
- Vyas AG, Kori VK, Rajagopala S, Patel KS (2013) Etiopathological study on cerebral palsy and its management by Shashtika Shali Pinda Sweda and Samvardhana Ghrita. Ayu 34(1): 56-62.
- Shukla V, Tripathi RD, Caraka Samhita (2017) Sutrasthan, Chaukhambha Sanskrit Pratishthan, Delhi 1: 223.
- Arun Raj GR, Uppinakuduru S, Rao PN (2022) Comparative clinical study to assess the effectiveness of Salavana Upanaha Sweda with and without Parisheka on spasticity in children with Cerebral Palsy, Annals Ayurvedic Med 11(1): 22-37.
- Shukla V, Tripathi RD (2017) Caraka Samhita, volume 2, Siddhisthan, Chaukhambha Sanskrit Pratishthan, Delhi 881.
- Shailaja U, Rao PN, Debnath P, Adhikari A (2014) Exploratory study on the Ayurvedic therapeutic management of cerebral palsy in children at a tertiary care hospital of karnataka, India. J Tradit Complement Med 4(1): 49-55.
- Shastri KA (2017) Susruta Samhita, Chikitsasthan, Chaukhambha Sanskrit sansthan, Varanasi 224.
- Shukla V, Tripathi RD (2017) Caraka Samhita, Sutrasthan, Chaukhambha Sanskrit Pratishthan, Delhi 2: 96.
- Shukla V, Tripathi RD (2017) Caraka Samhita, Siddhisthan, Chaukhambha Sanskrit Pratishthan, Delhi 2(958) 92.
- Rajput S, Patni K (2020) Randomized Clinical Trial to Evaluate the Efficacy of Atramental Ghrita Oral and Nasya in the Management of Cerebral Pals, International Journal of Ayurvedic Med 1 (3): 483-490.
- Shukla V, Tripathi RD (2017) Charaka Samhita, Chikitasasthan Chaukhambha Sanskrit Pratishthan, Delhi 2: 29.
- Singh N, Bhalla M, de Jager P, Gilca M (2011) An overview on ashwagandha: a Rasayana (rejuvenator) of Ayurveda. Afr J Tradit Complement Altern Med 8(5): 208-213.
- Kaushik R (2017) Studying the pharmacological basis of an antiepileptic Ayurvedic formulation-Sarasvata churna. Int. J. Green Pharm 11 (2): 62-68.
- Shastri K, Chaturvedi G (1996) Charak Samhita Purvardh, Vidyotini Hindi commentary 22nd edn, Sutrasthan, Chaukhambha Bharti Academy, Varanasi 98.
- Singh RH, Udupa KN (1993) Clinical and experimental studies on rasayana drugs and rasayana therapy. Special Research Monograph, Central Council for Research in Ayurveda, and Siddha (CCRAS), Ministry of Health and Family Welfare, New Delhi.
- Kumar N, Abichandani LG, Thawani V, Gharpure KJ, Naidu MUR, et al. (2016) Efficacy of standardized extract of Bacopa monnieri (Bacognize) on cognitive functions of medical students: a six-week, randomized placebo-controlled trial. Evid Based Complement Alternat Med 4103423.
- Chaudhari KS, Tiwari NR, Tiwari RR, Sharma RS (2017) Neurocognitive Effect of Nootropic Drug Brahmi (Bacopa monnieri) in Alzheimer's Disease. Ann Neurosci 24(2): 111-122.
- Verma J, Singhal HK (2013) Current Trends in Ayurvedic Management of Cerebral Palsy in Children. Journal of Biological & Scientific Opinion 1(3): 282-287.
- Shailaja U, Rao PN, Girish KJ, Arun Raj GR (2014) Clinical study on the efficacy of Rajayapana Basti and Baladi Yoga in motor disabilities of cerebral palsy in children. Ayu 35(3): 294-299.
- Deepti KA, Munnoli BT, Vijaykumar D, Arbar Aziz, Patil Amol (2014) Role of Matra Basti (Enema) over Abhyanga (Massage) and Sweda (Sudation) in Reducing Spasticity in Cerebral Palsy with Suddha Bala Taila - A Randomized Comparative Clinical Study. Int J Ayur Pharma Research 2(2): 47-52.
- Rajput S, Patni K (2019) Pharmacodynamics of Nasya Karma & Its Indications in Pediatric Disorders. International Journal of Scientific Development and Research (IJSDR) 4 (1): 182-185.






























