The Treatment of Chinese Medicine on Adolescent Alopecia
Tsz Man Tong and Chuen Heung Yau*
School of Chinese Medicine, the University of Hong Kong, Hong Kong
Submission: November 28, 2022; Published: December 19, 2022
*Corresponding author: Chuen Heung Yau, School of Chinese Medicine, the University of Hong Kong, Hong Kong
How to cite this article: Tsz Man T, Chuen Heung Y. The Treatment of Chinese Medicine on Adolescent Alopecia. J Complement Med Alt Healthcare. 2022; 11(5): 555821. DOI: 10.19080/JCMAH.2022.11.555821
Abstract
Hair is made of a kind of protein called keratin. Potential causes of hair loss in teenagers include genetic factors, hormonal imbalances, and underlying medical conditions, stressful or just not eating right .In some cases, hair loss can be reversible with proper treatment. Most of time, it will influence the youngster’s confidence in social activities. They usually feel inferior and don’t want to go out to play with friends. Also they prefer to wear a cap most of time even in indoors. However western medicine does not show a significant effect on it. Here through a case report, introduce the methods and curative effects of traditional Chinese medicine in the treatment of adolescent alopecia.
The study was carried out over 10 months with oral intake of Chinese Medicine treatment and external use of Chinese Medicine on whole body on daily basis. The results showed a marked improvement in the hair loss on the patient.
Keywords: Treatment; Chinese Medicine; Adolescent; Alopecia
Introduction
Hair is made of a kind of protein called keratin [1]. Potential causes of hair loss in teenagers include genetic factors, hormonal imbalances, and underlying medical conditions, stress or eating disorder [2]. In some cases, hair loss can be reversible with proper treatment. Most of the time it will influence the youngster’s confidence in social activities [3]. This article introduces the unique methods and curative effects of traditional Chinese medicine in the treatment of alopecia by illustrating with a case report.
Etiology
Alopecia can be divided into two types, which are scarring (cicatricial) and nonscarring (no cicatricial). Nonscarring alopecia is reversible whereas scarring alopecia is permanent. They can be differentiated by performing a detailed physical examination, medical history recording or scalp biopsy [4].
Alopecia maybe due to congenital and acquired conditions. The common cause of adolescent alopecia is mostly nonscarring. It includes tinea capitis, alopecia areata, trauma due to traction alopecia or trichotillomania, and telogen effluvium [5].
Pathophysiology
Depending on the types of alopecia, tinea capitis is caused by fungi infection in the hair follicles. While alopecia areata can be considered as an autoimmune disorder that triggers by genetic basis and environment [6].
Although traction alopecia and trichotillomania are behavior disorders, there are studies showing that likely to be multiple genes confer vulnerability to traction alopecia and trichotillomania. Some of these genes have also been identified in other forms of obsessive-compulsive behavior [7].
For telogen effluvium, stress occurs on the anagen hair follicle, which shifts the hair cycle into the resting, or telogen phase, leading to a large amount of hair loss over a short period of time [8].
Nutritional deficiency is another cause of alopecia, it includes protein insufficiency, vitamin excess or deficiency, zinc, iron and essential fatty acid deficiency, etc. Since protein in the form of keratin is the basic component of hair, inadequate intake of protein and other nutrients has been confirmed to be associated with hair conditions. It may affect the color, texture and elasticity of hair, which are the factors leading to hair loss [9].
Other causes of alopecia include drug history, psychosocial history, history of hair care used and present health and medical condition of the patient, etc [10].
Examination
Besides the physical examination of hair and scalp, practitioners can perform a pull test on patient. It is performed by grasping approximately 40- 60 hairs from multiple locations of the scalp using the thumb and forefinger. At the same time, a gentle traction is applied away from the scalp. Positive result shows that when more than 10% of hairs can be pulled from the scalp. This implies active hair shedding and suggests a diagnosis of telogen effluvium, anagen effluvium, or alopecia areata [11].
On the other hand, one should pay attention to the behaviour of patient to differentiate from traction alopecia and trichotillomania. Parents should observe whether their children have the habit of pulling their hairs, and most importantly take concerns on children to see if they encounter any difficulties or under stress at school or other social occasions. Conditions that causing hair loss is diverse, therefore laboratory tests should be performed when the history or physical examination findings suggest an underlying comorbidity, tinea capitis is one of the examples [12].
Testing the nutritional level in blood, a complete blood count, and complete metabolic panel can be performed for diagnosis of nutritional deficiency induced alopecia [13].
Management and treatment
Oral antifungal medication and shampoo can be given to patient with tinea capitis. It can decrease the carriage of visible spores and help to prevent reinfection [14].
The most common treatment for patients aged 10 or below with alopecia areata is topical corticosteroids. It can be used alone or with other topical steroids. Treatment for patients aged 10 or above includes topical sensitizers and intralesional corticosteroids [15].
Management is conservative for traction alopecia and trichotillomania in preschool-aged children. With the careful observation of the behavior of children and gently reminding them, situation can resolve within months in most cases. While behavioral therapy is required for teenagers and adults who are diagnosed with traction alopecia and trichotillomania. With the guidance of a psychologist or psychiatrist, habit reversal training and commitment training have been found to be an effective therapy [16].
Treatment of any underlying disorders and correction of nutritional deficiencies are equally important. By eliminating the underlying disorders and with the supplementation of any deficient nutrients, condition of hair can usually improve significantly [17].
Chinese Medicine for alopecia
Pathogenesis of alopecia in TCM
From the Chinese medicine perspective, alopecia is caused by the emotions of patient, consequences of other chronic diseases and not uncommon to be seen in the postpartum period of women. The above etiological factors lead to the insufficient of blood in the body, especially the weakness of blood vigor in liver and kidney. With the inadequate supply of blood and nutrients in hairs, they start to shed off [18].
Management of alopecia in TCM
In connection with the above factors, therapeutic approach of Chinese medicine includes herbal medicine, acupuncture, plum blossom needle and external therapy [19].
Common herbal medicine used for alopecia are herbs that can replenish qi and blood, and herbs that have the function for tonifying kidney. Depending in the accompanying symptoms of the patient, Chinese medicine practitioners may adjust their formula accordingly [20].
Acupuncture, plum blossom needle and external therapy provide a localized stimulation to the scalp of the patient, they equivalently improve the qi and blood supply in the scalp [21].
Case Features
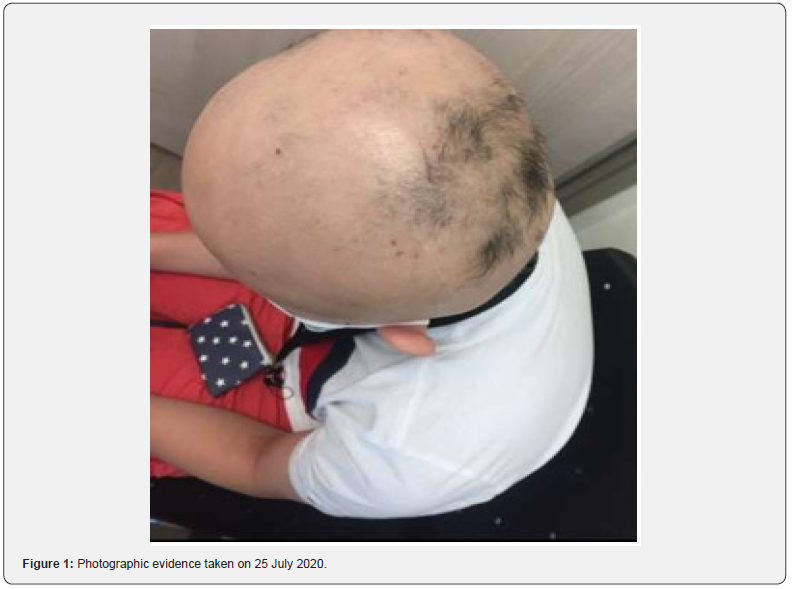
The patient was a 12-year-old male with Asia heritage. He was born in Hong Kong and raised in Japan, He was then returned to Hong Kong in 2019. His first visit to the Chinese Medicine clinic in Gleneagles Hospital was in July 2020. His chief complaints were hair loss, with skin itchiness for three years. The patient experienced hair loss three years ago because of the pressure of studying. He also experienced skin itchiness and chronic diarrhea. Scattered rash can be seen on limbs, and there was a total loss of hair on scalp. He had a good appetite and sleep. The patient had a red tongue with a white coating. His pulse was soft.
In the way of thinking of Chinese Medicine, the patient was diagnosed as alopecia and was considered as suffering from qi and blood deficiency syndrome.
Treatment
The treatment approach was to replenish qi and blood, as well as to strengthen the spleen of the patient.
Oral
An oral Chinese Medicine prescription was given to the patient on daily basis for over 10 months. The patient came to the clinic for follow-up consultation in every 1-2 weeks, with a mild change of the treatment plan according to the condition of the patient.
The Chinese Medicine prescription is as follow:
Ginseng and Bai-zhu Atractylodes Formula (Shen Ling Bai Zhu San) 12g
Processed Tuber Fleeceflower Root (Processed Heshouwu) 10g
Mongolian Milkvetch Root (Huangqi) 10g
Liquorice Root (Gancao) 10g
Glabrous Smilax (Tufuling) 2.5g
White Peony Root (Baishao) 5g
Yanhusuo Tuber (Yanhusuo) 5g
Costusroot (Muxiang) 5g
Common Jujube (Dazao) 10g
It is in powdered form (Nongs’ concentrated Chinese Medicine granules). The instruction of intake was twice a day after meal, by dissolving the powder in 250mL of hot water.
External
External use of Chinese Medicine is also prescribed to the patient for atopic use on scalp and body on daily basis.
The prescription is as follow:
Argy Wormwood Leaf (Aiye) 50g
Lightyellow Sophra Root (Kushen) 40g
Belvedere Fruit (Difuzi) 40g
Tree Peony Root (Mudanpi) 40g
Chinese Goldthread Rhizome (Huanglian) 20g
Japanese Honysuckle Flower Bud (Jinyinhua) 30g
Results
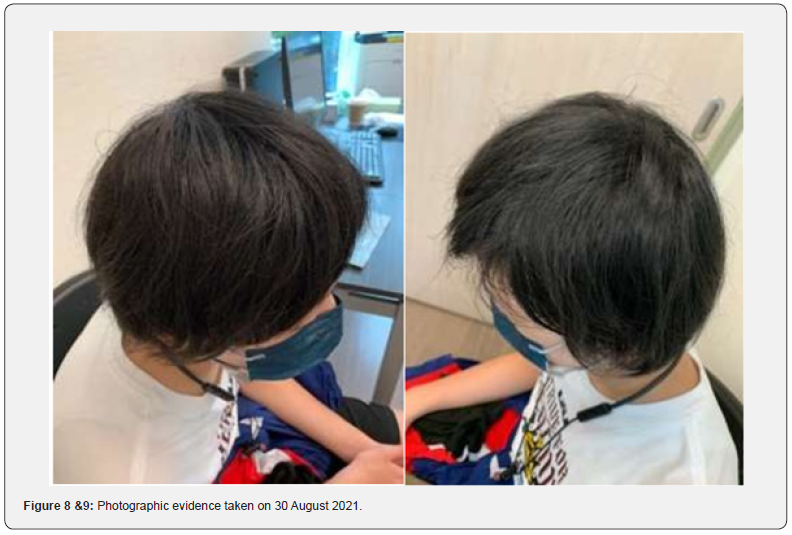
As observed from Figure 1 to 7, favourable results were observed over the period of treatment. With the intake of Chinese Medicine for the first two weeks, fine hair started to be grown over the head of the patient (See Figure 1). With the continuous treatment over 6 months, there were continuous hair growth (See Figure 2-5). Accompanying symptoms of diarrhea and skin rashes were also improved. By the completion of treatment after 10 months, there was complete hair growth over the scalp of the patient (See Figure 6-7).


Discussion
From the Chinese Medicine perspective, the patient was suffering from the dysfunction of spleen. The generation of qi and blood from spleen is affected, it at the same time disturbs the transportation of water and dampness in the body. Insufficient supply of qi and blood leads to hair loss, while the accumulation of dampness in the body give rise to the symptoms of diarrhea and skin rashes.

Patient has a spleen deficiency physique, which counts for the cause of chronic diarrhea. The patient suffers from nutritional deficiency (deficiency of qi and blood) due to chronic diarrhea, which in turn leading to hair loss.
Conclusion
The treatment approach is limited in Western Medicine, and there are possible side effects with the medication. By understanding the underlying causes and determine the syndrome differentiation of the patient, positive results can be seen from patients following with Chinese Medicine treatment. In order to maximize the benefit of patients, it is important to develop the cooperation between Chinese and Western medicine.
References
- Bereiter-Hahn J, Gedeon Matoltsy A, Sylvia Richards K (1986) Biology of the integument. 1st ed. New York: Springer-Verlag Berlin Heidelberg.
- Lin RL, Garibyan L, Kimball AB, Drake LA (2016) Systemic causes of hair loss. Ann Med 48(6): 393-402.
- Ghanizadeh A (2008) Comorbidity of psychiatric disorders in children and adolescents with alopecia areata in a child and adolescent psychiatry clinical sample. Int J Dermatol 47(11):1118-1120.
- Phillips TG, Slomiany WP, Allison R (2017) Hair Loss: Common Causes and Treatment. Am Fam Physician 96(6): 371-378.
- Cranwell W, Sinclair R (2018) Common causes of paediatric alopecia. Aust J Gen Pract 47(10): 692-696.
- Petukhova L, Cabral RM, Mackay-Wiggin J, Raphael C, Angela MC, et al. (2011) The genetics of alopecia areata: what’s new and how will it help our patients? Dermatol Ther 24(3): 326-336.
- Chattopadhyay K (2012) The genetic factors influencing the development of trichotillomania. J Genet 91(2): 259-262.
- Headington JT (1993) Telogen effluvium. New concepts and review. Arch Dermatol 129(3): 356-363.
- McKenzie CA, Wakamatsu K, Hanchard NA, Forrester T, Ito S (2007) Childhood malnutrition is associated with a reduction in the total melanin content of scalp hair. Br J Nutr 98: 159-164.
- Mubki T, Rudnicka L, Olszewska M, Shapiro J (2014) Evaluation and diagnosis of the hair loss patient: Part I. History and clinical examination. J Am Acad Dermatol 71(3): 415.e1-415.e15.
- Dhurat R, Saraogi P (2009) Hair evaluation methods: merits and demerits. Int J Trichology 1(2): 108-119.
- Xu L, Liu KX, Senna MM (2017) A Practical Approach to the Diagnosis and Management of Hair Loss in Children and Adolescents. Front Med (Lausanne) 4: 112.
- Sharma VK (1996) Pulsed administration of corticosteroids in the treatment of alopecia areata. Int J Dermatol 35: 133-136.
- Chen X, Jiang X, Yang M, Urbà G, Xiufang L, et al. (2016) Systemic antifungal therapy for tinea capitis in children. Cochrane Database Syst Rev 2016(5): CD004685.
- Trost LB, Bergfeld WF, Calogeras E (2006) The diagnosis and treatment of iron deficiency and its potential relationship to hair loss. J Am Acad Dermatol 54(5): 824-844.
- Sarah HM, Hanam FZ, Hilary ED, Martin EF et al. (2013) Habit reversal training in trichotillomania: guide for the clinician. Expert Rev Neurother 13(9): 1069-1077.
- Castelo-Soccio L (2014) Diagnosis and management of alopecia in children. Pediatr Clin North Am 61(2): 427-442.
- Huang Y, Liang CZ, Zhang Y (2007) Pharmacological studies of CP and its application indermatology. Yunnan. J Tradit Chin Med Mater Med 28: 42-44.
- Tang G, Xiong J, Fan Q, Guo H, Zhou X, et al. (2020) Plum-blossom needle plus Chinese herbal medicine for alopecia areata: A protocol for systematic review and meta-analysis. Medicine (Baltimore) 99(41): e22515.
- You Q, Li L, Ma X, Gao T, Xiong S, et al. (2019) Meta-Analysis on the Efficacy and Safety of Traditional Chinese Medicine as Adjuvant Therapy for Refractory Androgenetic Alopecia. Evid Based Complement Alternat Med 2019: 9274148.
- Chen Q, Tao Y, Wang L, Zhang J, Sun B, et al. (2020) A randomized controlled clinical study of acupuncture therapy for Seborrheic alopecia in young and Middle Ages: Study protocol clinical trial (SPIRIT compliant). Medicine (Baltimore) 99(17): e19842.






























