Efficacy of Osteopathic Manipulative Treatment (OMT) Vs Physiotherapy in Chronic Lateral Epicondylitis
Altadonna Giulio1, Cappelli Davide1, Orlandi Magli Antonella2, Raffa Debora2, Spinnato Paolo3, Filardo Giuseppe4,5, Tedeschi Roberto2 and Benedetti Maria Grazia 2*
1Collegio Italiano di Osteopatia (C.I.O.), Parma, Italia
2Physical Medicine and Rehabilitation Unit, IRCCS Istituto Ortopedico Rizzoli, Bologna, Italy
3Diagnostic and Interventional Radiology, IRCCS Istituto Ortopedico Rizzoli, Bologna, Italy y
4Applied and Translational Research Center, IRCCS Istituto Ortopedico Rizzoli, Bologna, Italy
5Faculty of Biomedical Sciences, Università Della Svizzera Italiana, Lugano, Switzerland
Submission: August 19, 2022; Published: September 19, 2022
*Corresponding author: Maria Grazia Benedetti, Physical Therapy and Rehabilitation Unit, IRCCS Istituto Ortopedico Rizzoli, Via Pupilli 1, 40136 Bologna, Italy
How to cite this article: Altadonna G, Cappelli D, Orlandi Magli A, Raffa D, Spinnato P, et al. Efficacy of Osteopathic Manipulative Treatment (OMT) 002 Vs Physiotherapy in Chronic Lateral Epicondylitis. J Complement Med Alt Healthcare. 2022; 11(4): 555818. DOI: 10.19080/JCMAH.2022.11.555818
Abstract
Background: Several rehabilitative treatments have been proposed for Lateral Elbow Tendinopathy (LET). Therapeutic exercise showed the greatest beneficial effects together with patient education, and multimodal treatment subject specific. In recent years, osteopathic manipulative treatment (OMT) has been proposed as treatment for LET. The aim of the study was to focus on this emerging approach by comparing it to more traditional physiotherapy.
Methods: Thirty-two patients with a diagnosis of LET were enrolled and randomly assigned to two groups: the OMT group and the physiotherapy group. In the former, patients underwent OMT according to the common techniques. In the latter, patients underwent a physiotherapy protocol consisting in stretching and strengthening exercises, and laser therapy. Outcome measures included the Patient-Rated Tennis Elbow Evaluation (PRTEE), the Mayo Elbow Performance, and VAS for pain. Assessment was carried out at baseline (T0), after 1 (T1) and 3 (T2) months. In addition, an ultrasound assessment of the elbow common extensor tendon was performed at T0 and T2.
Results: Both the OMT and the Physiotherapy group showed a statistically significant improvement along the follow-up for VAS for pain and PRTEE score. No significant difference was found for the Mayo Score in the Physiotherapy group. Ultrasound assessment confirmed the presence of abnormalities of vascularization, echogenicity, and thickness of the tendon at T0, partially reduced at T2.
Conclusion: OMT and physiotherapy resulted both effective in the treatment of LET, offering a significant clinical improvement which helped patients recovering their functional activities in the short-term follow-up.
Keywords: Lateral elbow tendinopathy; Osteopathic manipulative treatment; Exercise
Abbreviations: LET: Lateral Elbow Tendinopathy; OMT: osteopathic manipulative treatment; PRTEE: Patient-Rated Tennis Elbow Evaluation; SST: Soft Tissue Technique; MR: Myofascial Release Techniques; MET: Muscle Energy Techniques; HVLA: High-Velocity and Low-Amplitude Techniques
Introduction
Lateral Elbow Tendinopathy (LET), also known as “tennis elbow”, is an “overuse” syndrome [1,2]. It is characterized by weakness and pain on palpation over the lateral epicondyle often radiating distally to the forearm and associated with pain on resisted dorsiflexion of the wrist and/or middle finger, with the symptoms being aggravated by prehension [3]. In the overall population its prevalence is 1-3% with a peak incidence over 40-50 years of age [4]. It can lead to functional limitations during the activities of daily life, and disability [5]. Generally, the muscle involved is the short radial extensor of the carpus, but in some cases the pronator muscles of the forearm also appear to be affected [6]. The average duration of a typical episode is between 6-24 months, but symptom duration does not seem to be related to its severity, and 89% of patients recover within one year [7].
The main risk factors recognized are the handling of loads >20kg at least 10 times/day, repetitive movements >2h/day [8], and some minor but not negligible factors should be added such as: subjects with rotator cuff problems [9], sports activities such as tennis, age between 45-54 years, use of oral steroids, other tendinopathies, Caucasians, and smoking patients. Numerous studies have shown the absence of inflammatory cells in individuals with LET, while changes in tendon function have been found to be neurogenic (presence of chemical mediators of pain such as substance P and calcitonin due to altered afferent inputs), vascular (neovascularization), and structural (presence of necrotic fibers and high percentage of rapidly contracting fibers). The term LET or lateral tendinopathy is therefore correct while epicondylitis should be abandoned [10].
Regardless of the etiopathogenetic mechanisms, treatments are often only partially successful, and there are controversial results on the benefits of one approach over the others [11,12]. In this scenario, more comparative trials are needed. Since in recent years the osteopathic manipulative treatment (OMT) has spread as a solution to address epicondylitis, the aim of this study was to focus on this emerging treatment approach by comparing it to a more traditional physiotherapy approach.
Materials and Methods
Study Design and Ethics
The clinical trial is a randomized controlled trial open to two groups. The study, approved by the Ethical Committee (N.0006310), was conducted at the outpatient’s clinic of the hospital. Patients enrolled for the study signed an informed consent.
Patients
Patients with diagnosis of chronic LET were consecutively enrolled, according to the inclusion and exclusion criteria. The inclusion criteria were age 25-60 years, diagnosis of LET (clinical tests, ultrasound assessment), pain for at least 3 months. The exclusion criteria were arthritis, autoimmune diseases, presence of calcifications, cervical radiculopathies, dis-metabolic diseases, major elbow instability, previous trauma-fractures-surgery at the upper limb, neurological pathologies, injective therapy at the elbow in the previous 3 months, pathological deformities, psychiatric diseases.
Patients were assigned to one of the two arms according to a block randomization list of 6, encrypted and managed by the data manager. In the study group, patients underwent OMT (OMT group), in the control group (Physiotherapy group) the patients underwent the physiotherapy protocol in the outpatient clinic of the physical therapy and rehabilitation unit of the hospital. In each group treatments were always performed by the same operator.
Treatment
Osteopathic Manipulative Treatment (OMT): Six sessions of treatment were carried out at: the first three at a distance of 7 days, the fourth after 15 days, the fifth after 20 days and the sixth and last after 30 days. Each treatment had a duration of about 45 minutes and the functional rebalancing occurred mainly through soft tissue techniques (Soft Tissue Technique, SST), myofascial release techniques (MR), muscle energy techniques (MET), and high-velocity and low-amplitude techniques (HVLA). The applied techniques were chosen based on the manual evaluation criteria by the operator of the patient and they were tissue-specific and patient-specific.
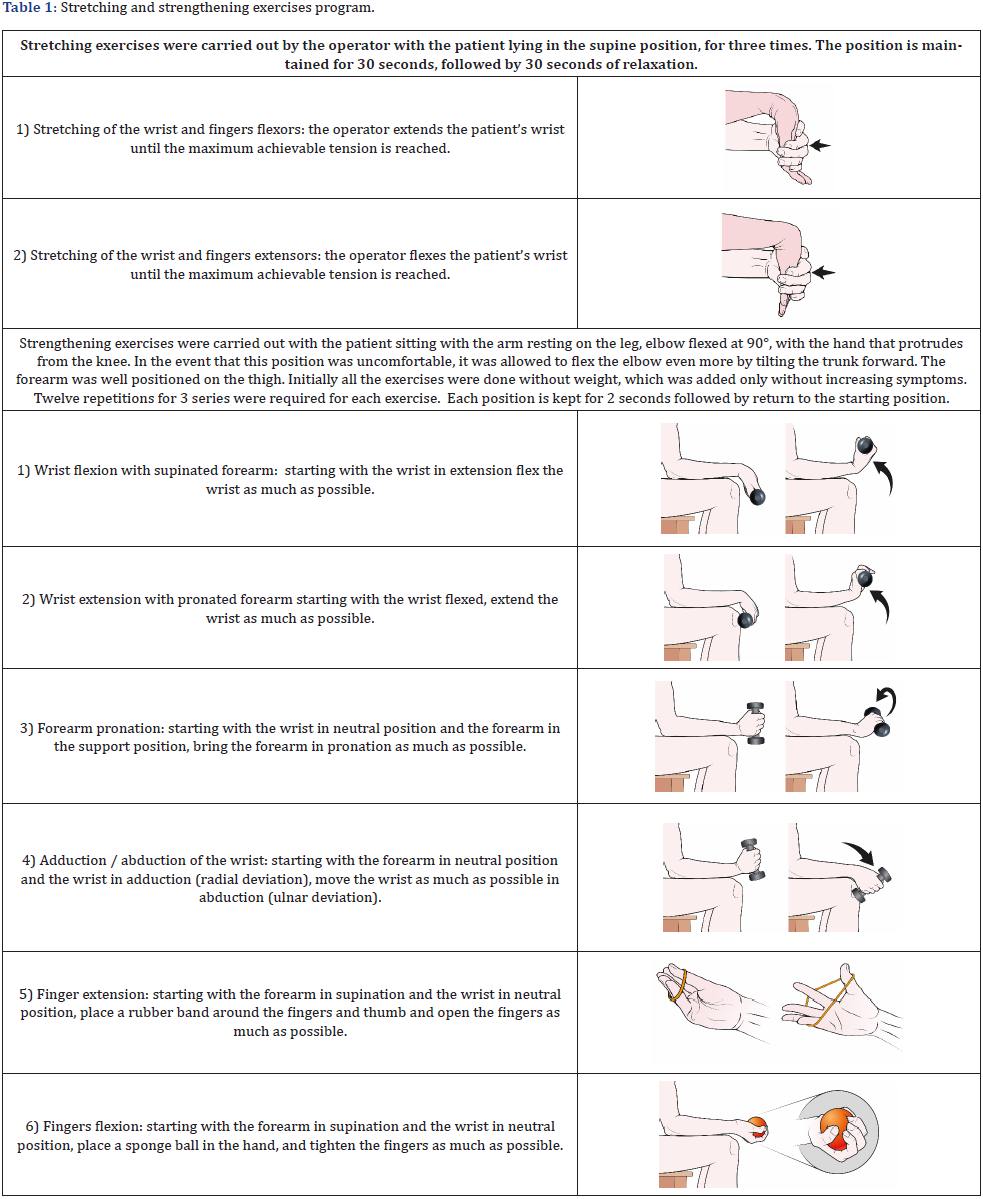
Physiotherapy Protocol: The rehabilitation protocol, as per usual care in our center based on previous studies [12-14] provided sessions of a duration of 30 minutes, carried out daily, for a total of 10 sessions. The session was thus organized: 20 minutes of manual therapy composed of stretching exercises of flexor muscles and wrist extensors, muscular strengthening exercises for the muscles of the forearm, wrist, and fingers, ND-YAG laser therapy session in scan mode (peak fluence: 970-1350 mj / cm2; Frequency 10-30 Hz: Total energy: 3000 J). The stretching and strengthening exercises protocol is illustrated in Table 1.
Outcome Measures: Patients enrolled for the study were assessed by means of the administration of clinical-functional scores at baseline (T0). Assessment was repeated at 1 (T1) and 3 (T2) months of follow-up. The Patient-Rated Tennis Elbow Evaluation (PRTEE), a 15-item questionnaire specifically designed for patients with LET [15] was used for self-assessment of forearm pain and disability as primary endpoint. The items investigate pain (5 items) and the degree of difficulty in performing various activities (6 specific and 4 usual activity items) due to the elbow problem over the preceding week. Each item has 1 response option (0 no difficulty, 10 unable to perform). The scores for the various items are used to calculate an overall scale score ranging from 0(best score) to 100 (worst score). The Mayo Elbow Performance Score, measures elbow function across four domains: pain (45 points), stability (10 points), range of motion (20 points), and daily functional tasks (25 points). Scores are categorized as 90- 100 = excellent, 75-89 = good, 60-74 = fair, 0-59 = poor [16].
Furthermore, to confirm the LET diagnosis, an ultrasound assessment was carried out at T0 with a linear US probe with musculoskeletal settings, considering the following parameters: vascularization, echogenicity, and the thickness in mm of the affected tendon (elbow common extensor tendon). Calcifications or other abnormalities were also reported. The vascularization and echogenicity parameters were defined on a visual scale, always evaluated by the same operator (P.S. with 10 years of experience in musculoskeletal imaging). Both echogenicity and vascularization expressed the inflammations of the tendon. Indeed, inflammatory changes in tendons result in a hypervascularization detectable at power-color-Doppler, as well as a reduction of echogenicity of the tendon’s fibers. These parameters have been semi-quantitatively graded as follows: 0 normal findings, 1 mild alteration, 2 moderate alteration, 3 severe alteration, based on the extension and severity of the abnormalities. The ultrasound assessment was repeated also at T2.
Statistical Analysis
The sample estimate was carried out through a Power Analysis. The primary endpoint was considered (PRTEE), with a minimum significant difference of 5 points. Based on the standard deviation of this score (4.1) derived from the literature [17], considering a significance of 0.05 and a power of 0.9, the number of patients was settled to 16 per group, for a total of 32 patients. By expecting the possibility of having dropouts in the study design 36 patients were scheduled in total (18 per group). All continuous data were summarized in terms of mean ± standard deviation, while categorical variables were summarized in terms of frequency and percentage. The Shapiro-Wilk test was used to assess the normal distribution. The Levene test was used to assess the homoscedasticity. The Student T- Test for unpaired data was used to compare age, basal VAS pain, PRTEE, Mayo scores between the two groups. The categorical variables (side, sex) were analyzed through the Fisher Chi Squared for the study of the frequencies.
Repeated measures ANOVA with Sidak post-hoc test was used to assess the difference along the follow ups in each group of continuous variables. Friedman test with Wilcoxon post-hoc test was used to assess the difference along the follow ups in each group of ordinal variables. One Way ANOVA was used to compare the groups showing continuous, normally distributed, and homoscedastic data; the Mann-Whitney non-parametric test was used otherwise. To compare the groups, the Delta percentage of change with respect to the basal value during follow up was also used. The statistical analysis was performed using the statistical package for social sciences (IBM SPSS Statistics for Windows, Version 19.0. Armonk, NY: IBM Corp) by an expert statistical consultant from our institute.
Results
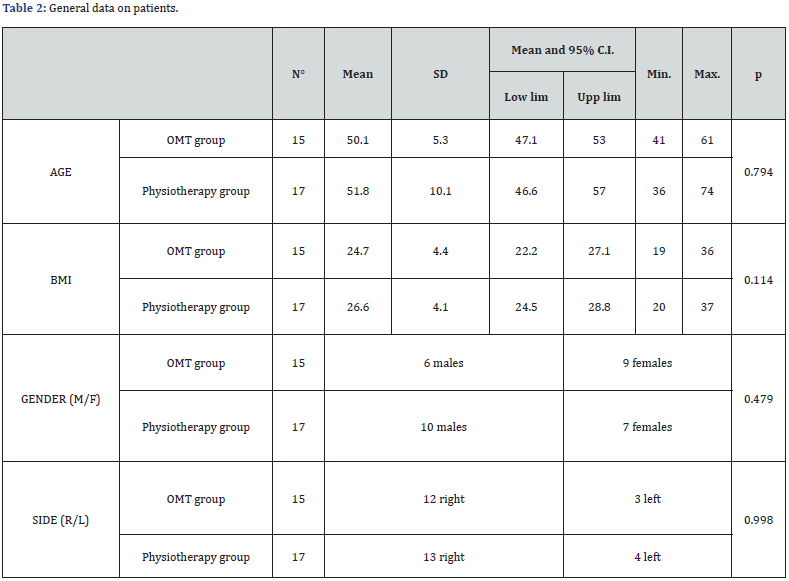
Thirty-six patients were recruited for the study. Two patients dropped out for further diagnostic assessment that led to another diagnosis (screening failures), and 2 patients did not complete the follow-up assessment. Thirty-two patients were included in the study, 15 in the OMT group and 17 in the physiotherapy group. Individual general data are reported in Table 2. No statistical difference was found for general data between the two groups. Statistical analysis did not show any difference between groups at any follow-up (Table 3), except for a significant difference for VAS Pain at T0. For this reason, delta values were calculated and no difference was found between T0-T1 and T0-T2 for both groups (Figure 1).
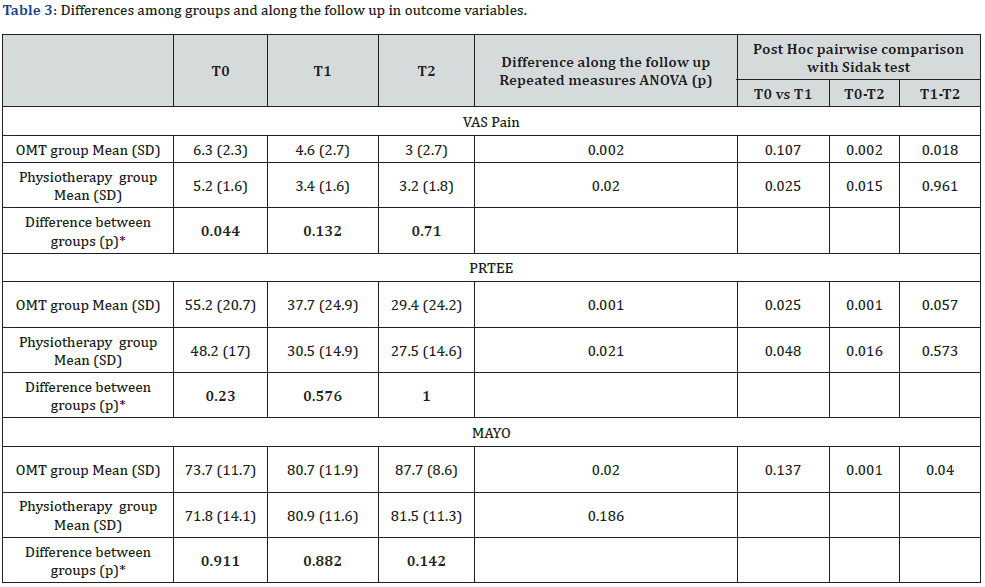
*One Way ANOVA
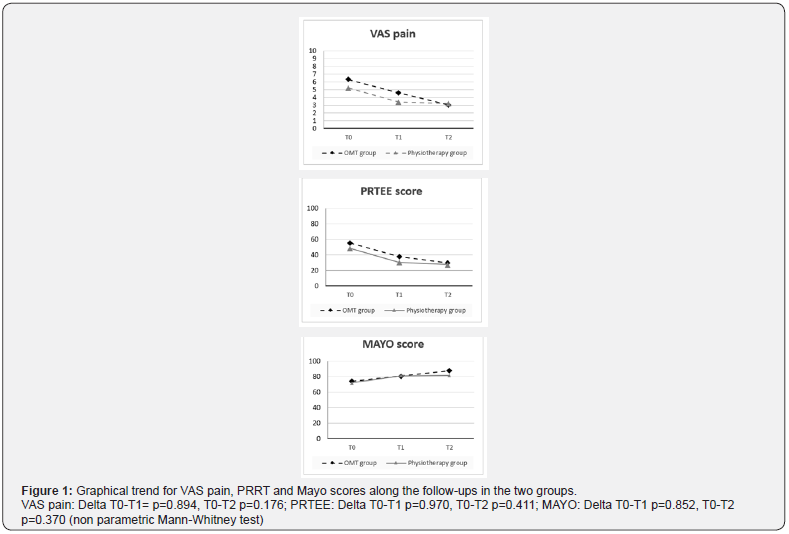
Both the OMT and the Physiotherapy groups showed a statistically significant improvement along the follow-up for the VAS for pain and the total PRTEE score. No significant difference was found for the Mayo Score in the Physiotherapy group. Data are reported in Table 3. Post hoc pairwise analysis evidenced that VAS improved in the Physiotherapy group between T0-T1 and T0-T2, without difference between T1-T2. No improvement was found in the OMT group between T0-T1, while pain decreased between T0- T2 and T1-T2.
The PRTEE score increased along all the follow up in both the OMT and the Physiotherapy group with a significant decrease between T0-T1 and T0-T2, without significant changes between T1-T2. The Mayo score in the OMT did not change significantly between T0-T1, while an improvement was present both between T0-T2 and T1-T2. Tendon ultrasound evaluation was taken respectively in 14 patients in the OMT group and in 16 in the Physiotherapy group at T0, and in 8 patients and 10 patients at T2. Although an improving trend in the parameters assessed was present, no significant difference between groups both at T0 and T2 was found except for the reduction of the parameter hypo intensity at T2 in the Physiotherapy group (Table 4).

*Mann-Whitney non-parametric test
Discussion
The main findings of this randomized controlled trial are that both OMT and a more classical physiotherapy approach are effective interventions for the treatment of chronic LET, offering a significant clinical improvement which helped patients recovering their functional activities in the short-term followup, without requiring more invasive treatments. These data add to a controversial literature where several approaches have been previously documented with heterogeneous reports and conflicting evidence. Among the rehabilitation treatments of LET, although they are well recognized as effective [17], there is no agreement about which one may be more beneficial [11,12,18].
Current evidence seems to be in favor of therapeutic exercise through eccentric, concentric and isometric exercises, and exercise has been shown to be more effective than ultrasound and massage [19,20]. Isometric exercise seems to be more effective to address pain and disability but not in terms of grip strength and perception of the subject [1,12,21]. Finally, ultrasound has not shown to be more effective than placebo in terms of decrease in pain and general improvement perceived by the patient. Similarly, shock waves were no more effective than placebo or other therapies [22,23]. Orthosis does not seem to be effective while dry needling is more effective than placebo and short-term ultrasounds [11,24].
The manipulations of wrist, elbow, and cervico-thoracic region can be useful in the short term in the reduction of pain, but they are difficult to evaluate due to their little specificity and there is insufficient evidence [10,25,26]. Stretching and strengthening exercises seem to have a better short-term effect than ultrasound or massage and there seems to be no difference between isotonic or isometric exercise compared with stretching exercises [13,27]. Another commonly used approach is the laser treatment. Laser has proved effective in reducing pain [14,28,29]. The Kinesio Taping could have positive effects on high and medium intensity work resistance [30]. Finally, orthobiologic injective treatments are emerging, although with still controversial findings [31,32].
Among all these options, the osteopathic Manipulative Treatment (OMT) is emerging as one of the suitable noninvasive approaches to address LET [33,34]. The osteopathic approach is based on the tissue self-healing capacity in a proper homeostatic condition [35]. To this purpose, the evaluation of the patient and the osteopathic treatment should consider also structures that are distant from the area affected by the symptom/pathology, according to a functional, mechanical/anatomical, neurological, and metabolic approach [36].
This allows the identification of what in osteopathy takes the name of “primary somatic dysfunction”, understood as myofascial alteration, and functional compensation that can be related to the symptom [37]. From an osteopathic point of view, the lateral tendinopathy of the elbow can be interpreted as the result of a functional overload of the elbow, which is often associated with myofascial restrictions at shoulder, cervical and thoracic spine, with consequent functional overload of the distal part of the upper limb during daily movements. These restrictions also represent an obstacle to the lymphatic flow resulting in difficulties in eliminating catabolites and inflammation mediators.
As with any manual technique, the effect of the OMT can also be attributed to pain modulation through the activation of descending pain inhibition systems. Osteopathic treatment could uniquely influence cellular function, direct muscle contraction and critical processes such as healing from a wound by cellular mechanisms. The OMT treatment is not easily repeatable since it is operator dependent in its evaluation part and because it is not possible to objectify pressure, tissue features, application times, etc., although the osteopathic rationale is based on concepts of well-known and documented physiology. This is the reason for which in the present study a single operator carried out all OMT treatments.
In this study a similar outcome was documented for both treatments, suggesting the potential of the osteopathic approach to offer similar results than the more classic physiotherapic approach. The base of this results could be related to the correlation between osteopathic treatment and self-healing mechanisms [38], restoring the proper functional conditions of the limb, even though specific mechanisms are difficult to be documented. Understanding the molecular mechanisms through which the MR and other osteopathic techniques work would help to define the foundations of their clinical efficacy [38]. Also, the data show that the OMT treatment can be alternative to standard physiotherapy treatment with fewer sessions, with a saving of time and resources, and the treatments are well tolerated by patients.
This study presents some limitations. The osteopathic assessment is very operator dependent. This implies that findings in the present study could not be reproducible, and other studies confirming the results of this work would be desirable. A further limit is the sample size, since the statistical analysis of the ultrasound evaluation was conditioned by the low number of evaluations carried out. However, the most important outcome in these patients is the clinical improvement, rather than tissue related changes which have not been clearly correlated with neither pain nor functionality. Finally, the Mayo score, compared to other scores, seems to be the one less able to describe the trend over time of the groups taken into consideration with respect to the studied pathology, but it was not the only assessment tool considered to this purpose. Beside these limitations, this study still offered important data, and represent one of the few RCTs in this challenging field where osteopathic treatments are rarely documented with a proper study design.
Conclusion
This study demonstrated the effectiveness of the osteopathic treatment which produced results overlapping with those of standard physiotherapy treatment at a short-term followup. Accordingly, this study poses the foundations for further trials to evaluate the inclusion of osteopathic treatment among possible intervention for LET. OMT and traditional rehabilitative intervention intervene on perfectly complementary aspects: the first is oriented to restore the general homeostatic conditions in order to enhance intrinsic self-healing capabilities, the second acts directly on the tendon impairment and therefore on the pathology itself. Future studies should explore the possibility of integrating both approaches to optimize the results and more effectively address patients affected by LET.
Declarations Section
Availability of supporting data: The protocol and the dataset analyzed during the current study is available from the corresponding author on reasonable request.
Competing interests: The authors report no declarations of interest.
Funding: This research had the Institutional financial support for scientific research 5x1000 2019.
Authors’ contributions: GA, DC, AOM, and MGB contributed to conception and design of the study; AOM, DR and PS to data acquisition, GA and MGB to data analysis and interpretation; GA, GF and RT contributed to draft the manuscript; GF and MGB contributed to the critical revision for important intellectual content. All authors read and approved the final version of the manuscript.
Acknowledgements
The authors wish to thank prof. M. Marcacci for having allowed the realization of this trial, Mauro Fornari and Giovanni Amadasi of the Collegio Italiano di Osteopatia (C.I.O.) for the support and contributions in the osteopathic field. In addition, we thank all those who have contributed to the realization of this trial in particular, Roberto Rotini, Patrizia Pelotti, Lorenzo Cavazzuti, Andrea Cotti and Mrs. Giuliana Nervuti, of the Istituto Ortopedico Rizzoli, for her precious and generous help, and Elettra Pignotti, statistical engineer for the support in statistical analysis.
References
- RP Nirschl (2015) The epidemiology and health care burden of tennis elbow: a population-based study, Ann Transl Med 3(10): 133.
- R Rotini, M Fontana, L Catamo, F Noia, M Magnani (2000) Lateral epicondylitis: clinical classification and proposal for treatment, Chir Organi Mov 85(1): 57-64.
- P Stratford, D Levy (1994) Assessing Valid Change over Time in Patients with Lateral Epicondylitis at the Elbow 4(2): 88-91.
- ME Pitzer, PH Seidenberg, DA Bader (2014) Elbow tendinopathy, Med Clin North Am 98(4): 833-849.
- U Fredberg, K Stengaard-Pedersen (2008) Chronic tendinopathy tissue pathology, pain mechanisms, and etiology with a special focus on inflammation, Scand J Med Sci Sports18(1): 3-15.
- DM Walz, JS Newman, GP Konin, G Ross (2010) Epicondylitis: pathogenesis, imaging, and treatment, Radiographics 30(1) :167-184.
- BK Coombes, L Bisset, B Vicenzino (2009) A new integrative model of lateral epicondylalgia, Br J Sports Med. 43(4): 252–258.
- RM Van Rijn, BMA Huisstede, BW Koes, A Burdorf (2009) Associations between work-related factors and specific disorders at the elbow: a systematic literature review, Rheumatology (Oxford) 48: 528-536.
- AG Titchener, A Fakis, AA Tambe, C Smith, RB Hubbard, et al. (2013) Risk factors in lateral epicondylitis (tennis elbow): a case-control study, J Hand Surg Eur 38(2): 159-164.
- B Vicenzino, JA Cleland, L Bisset (2007) Joint manipulation in the management of lateral epicondylalgia: a clinical commentary, J Man Manip Ther 15(1): 50-56.
- LM Bisset, B Vicenzino (2015) Physiotherapy management of lateral epicondylalgia, J Physiother 61(4): 174-181.
- D Trudel, J Duley, I Zastrow, EW Kerr, R Davidson, et al. (2004) Rehabilitation for patients with lateral epicondylitis: a systematic review, J Hand Ther 17(2): 243-266.
- JA Martinez-Silvestrini, KL Newcomer, RE Gay, MP Schaefer, P Kortebein, et al. (2005) Chronic lateral epicondylitis: comparative effectiveness of a home exercise program including stretching alone versus stretching supplemented with eccentric or concentric strengthening, J Hand Ther 18(4): 411-419.
- O Oken, Y Kahraman, F Ayhan, S Canpolat, ZR Yorgancioglu, et al. (2008) The short-term efficacy of laser, brace, and ultrasound treatment in lateral epicondylitis: a prospective, randomized, controlled trial, J Hand Ther 21(1): 63-67.
- A Cacchio, S Necozione, JC MacDermid, JD Rompe, N Maffulli, et al. (2012) Cross-cultural adaptation and measurement properties of the italian version of the Patient-Rated Tennis Elbow Evaluation (PRTEE) questionnaire, Phys Ther 92(8): 1036-1045.
- UG Longo, F Franceschi, M Loppini, N Maffulli, V Denaro (2008) Rating systems for evaluation of the elbow, Br Med Bull. 87(1): 131-161.
- YJ Kim, SM Wood, AP Yoon, JC Howard, LY Yang, et al. (2021) Efficacy of Nonoperative Treatments for Lateral Epicondylitis: A Systematic Review and Meta-Analysis, Plast Reconstr Surg. 147(1): 112-125.
- M Bateman, JP Evans, V Vuvan, V Jones, AC Watts, et al. (2021) Protocol for the development of a core outcome set for lateral elbow tendinopathy (COS-LET), Trials 22: 339.
- S Karanasios, V Korakakis, R Whiteley, I Vasilogeorgis, S Woodbridge, et al. (2021) Exercise interventions in lateral elbow tendinopathy have better outcomes than passive interventions, but the effects are small: a systematic review and meta-analysis of 2123 subjects in 30 trials, Br J Sports Med 55(9): 477-485.
- DY Wen, BJ Schultz, B Schaal, ST Graham, BS Kim (2011) Eccentric strengthening for chronic lateral epicondylosis: a prospective randomized study, Sports Health 3(6): 500-503.
- L Landesa-Martínez, R Leirós-Rodríguez (2021) Physiotherapy treatment of lateral epicondylitis: A systematic review, J Back Musculoskelet Rehabil 35(6): 463-477.
- C Zheng, D Zeng, J Chen, S Liu, J Li, et al. (2020) Effectiveness of extracorporeal shock wave therapy in patients with tennis elbow: A meta-analysis of randomized controlled trials, Medicine (Baltimore) 99(30): e21189.
- S Karanasios, GK Tsamasiotis, K Michopoulos, V Sakellari, G Gioftsos (2021) Clinical effectiveness of shockwave therapy in lateral elbow tendinopathy: systematic review and meta-analysis, Clin Rehabil 35(10): 1383-1398.
- SJ Kachanathu, AM Alenazi, AR Hafez, AD Algarni, AM Alsubiheen (2019) Comparison of the effects of short-duration wrist joint splinting combined with physical therapy and physical therapy alone on the management of patients with lateral epicondylitis, Eur J Phys Rehabil Med 55(4): 488-493.
- AC Reyhan, D Sindel, EE Dereli (2020) The effects of Mulligan’s mobilization with movement technique in patients with lateral epicondylitis, J Back Musculoskelet Rehabil. 33(1): 99-107.
- P Zunke, A Auffarth, W Hitzl, M Moursy (2020) The effect of manual therapy to the thoracic spine on pain-free grip and sympathetic activity in patients with lateral epicondylalgia humeri. A randomized, sample sized planned, placebo-controlled, patient-blinded monocentric trial, BMC Musculoskelet Disord 21: 186.
- P Hoogvliet, MS Randsdorp, R Dingemanse, BW Koes, BMA Huisstede (2013) Does effectiveness of exercise therapy and mobilisation techniques offer guidance for the treatment of lateral and medial epicondylitis? A systematic review, Br J Sports Med. 47(17): 1112-1119.
- A Zati, BC Colori, D Fortuna, L Gelsomini, TW Bilotta (2008) Lateral elbow epicondylitis (tennis elbow): comparison between high intensity LASER Therapy and TENS in a clinical study, Medicina dello sport 61(2): 207-222.
- Z Simunovic, T Trobonjaca, Z Trobonjaca (1998) Treatment of medial and lateral epicondylitis--tennis and golfer’s elbow--with low level laser therapy: a multicenter double blind, placebo-controlled clinical study on 324 patients, J Clin Laser Med Surg 16(3): 145-151.
- S Zhang, W Fu, J Pan, L Wang, R Xia, et al. (2016) Acute effects of Kinesio taping on muscle strength and fatigue in the forearm of tennis players, J Sci Med Sport 19(6): 459-464.
- G Filardo, B Di Matteo, E Kon, G Merli, M Marcacci (2018) Platelet-rich plasma in tendon-related disorders: results and indications, Knee Surg Sports Traumatol Arthrosc 26: 1984-1999.
- WD Murrell, S Tulpule, NA Yurdi, A Ezekwesili, N Maffulli, et al. (2022) Orthobiologics for the Treatment of Tennis Elbow, In: G Filardo, BR Mandelbaum, GF Muschler, SA Rodeo, N Nakamura (Eds.), Orthobiologics: Injectable Therapies for the Musculoskeletal System, Springer International Publishing, Cham pp: 191-204.
- C Koh, MA Seffinger (2016) Muscle Energy Technique Improves Chronic Lateral Epicondylitis, J Am Osteopath Assoc 116(1): 58.
- S Küçükşen, H Yilmaz, A Sallı, H Uğurlu (2013) Muscle energy technique versus corticosteroid injection for management of chronic lateral epicondylitis: randomized controlled trial with 1-year follow-up, Arch Phys Med Rehabil 94(11): 2068-2074.
- S Paulus (2013) The core principles of osteopathic philosophy, International Journal of Osteopathic Medicine 16(1): 11-16.
- S Walkowski, M Singh, J Puertas, M Pate, K Goodrum, et al. (2014) Osteopathic manipulative therapy induces early plasma cytokine release and mobilization of a population of blood dendritic cells, PLoS One 9: e90132.
- T Liem (2016) A.T. Still’s Osteopathic Lesion Theory and Evidence-Based Models Supporting the Emerged Concept of Somatic Dysfunction, J Am Osteopath Assoc 116(10): 654-661.
- M Zein-Hammoud, PR Standley (2015) Modeled Osteopathic Manipulative Treatments: A Review of Their in Vitro Effects on Fibroblast Tissue Preparations, J Am Osteopath Assoc 115(8): 490-502.






























