Traditional Chinese Medicine in the treatment of Polyneuropathy - A Pilot Study
Dipl NanoSc S Schink1,2*
1Carl Remigius Medical School, Germany
2Klinik am Steigerwald GmbH & Co. KG, Gerolzhofen, Germany
Submission: May 23, 2022; Published: June 14, 2022
*Corresponding author: Sandra Schink, An den Weihern 49, 51467 Bergisch Gladbach; Germany
How to cite this article: Dipl NanoSc S Schink. Traditional Chinese Medicine in the treatment of Polyneuropathy - A Pilot Study. J Complement Med Alt Healthcare. 2022; 11(4): 555817. DOI: 10.19080/JCMAH.2022.11.555817
Abstract
Polyneuropathy is a generalized disease of the peripheral nervous system and most commonly caused by diabetes and alcohol abuse. However, the cause often remains unknown, which means that only symptomatic treatment is available. Pain is treated with moderate success leading to unsatisfying treatment results which also reduce the patients’ quality of life. The pilot study’s aim was to demonstrate that Traditional Chinese Medicine (TCM) can be an opportunity of treating polyneuropathy, improving symptoms and the quality of life. 12 patients were included into the study, treated with a combination of Chinese herbal medicine, acupuncture, moxa, qi gong, dietetics, Japanese overheating bath and lens bath at the Klinik am Steigerwald. Sensitivity, motor skills, reflexes and anamnestic parameters were examined at the beginning. The patients completed the SF-36 questionnaire in order to assess quality of life. Due to the Covid-19 pandemic, there were 2 Dropouts. A significant improvement (p=0.00579) was observed in the area of hypesthesia at the back of the foot/sole. Pain decreased significantly in 7 patients (p=0.01381, n=8). Cold sensation could be restored in at least one segment in 6 patients (60%), warm sensation restored in 5 patients (50%) left and 4 patients (40%) right. At least 3 touch sensation improvements were seen in 5 patients (50%). The quality of life of the patients was also improved by the therapeutic concept. A significant improvement could be achieved in the area of physical function with p=0.00911. The data suggests that there is a positive effect of TCM on idiopathic polyneuropathy as measured by subjective parameters.
Keywords: Polyneuropathy; Chinese Medicine; Acupuncture; Neuropathy
Abbreviations: PNP: Polyneuropathy; TCM: Traditional Chinese Medicine
Introduction
Polyneuropathy (PNP) is a generalized disorder of the peripheral nervous system that causes systemic, motor, or sensorimotor damage to the peripheral nerves. PNP is associated with a prevalence of about 5-8% in adulthood and is therefore the most common disorder of the peripheral nervous system [1]. Approximately 25% of the diagnosed PNP are chronic sensorimotor polyneuropathy, i.e., a chronic polyneuropathy with unclear cause [2]. Most patients with an unclear cause of PNP have chronic axonal degeneration which progresses slowly [3]. It is a typical disorder of late adulthood, affecting patients in their 50–60s. The onset is insidious, with symptoms appearing gradually over months to years. Patients experience sensory loss or paresthesias beginning symmetrically in the feet and ascending proximally. Deep tendon reflexes are reduced or absent. A nerve conduction velocity measurement shows a reduced amplitude or a lack of sural sensory response in 75% of patients [4]. Conventional treatment of neuropathic pain by antiepileptic and tricyclic antidepressant drugs is common [5]. However, meta-analysis showed that only a minority of patients with PNP respond to drug treatment [6] and drug treatment of the reduced sensation is ineffective [5]. A Cochrane analysis in 2017 showed that no adequate, randomized controlled studies for the treatment of chronic idiopathic sensorimotor polyneuropathy have been published to date and that, due to the lack of observational studies, there is no definitive choice of treatment for chronic idiopathic sensorimotor polyneuropathy [7]. Although the WHO has classified PNP as a disease which can be treated effectively by acupuncture, data on PNP and acupuncture are sparse [5]. Studies are needed to show that TCM is a safe and effective method for the treatment of polyneuropathies. This study should show that there is an improvement in the symptoms of polyneuropathy and an improvement of patient’s quality of life.
Methods
12 patients with confirmed diagnosis of PNP were enrolled in the study and treated with a combination of Chinese herbal medicine, acupuncture, moxa, Qi Gong, dietetics, Japanese overheating bath and lentil bath at the Klinik am Steigerwald in Germany for an average of three weeks. Every patient received an individual diagnosis with an individual treatment. The most frequently used acupuncture points were St 36 and and St 40. The herbal mixture Lysi-Kush was administered to all patients.
Sensitivity in six skin areas, motor function, reflexes and anamnestic parameters including pain were examined before and 15 weeks after therapy. In addition, the quality of life of the patients was assessed at both times using SF-36. An improvement was defined as a subjective improvement and an aggravation was defined as a subjective aggravation of symptoms.
When evaluating the SF-36 questionnaire, a standardized recoding of the values stated by the patients in the questionnaire is performed. By forming a pre-post difference and determining a mean value, a p-value can be obtained using the paired twosample t-test. The two-sample t-test was also used for the pain scale, anamnestic parameters, and indication of the severity of paresthesias. A p-value of p<0.05 was considered significant. For the evaluation of the measured parameters (temperature, touch, pain and vibration sensation), a confidence interval for the success probability of a binomial distribution is used as an analysis tool. The Clopper-Pearson interval is used to determine the lower boundary pu and the upper boundary po.
Results
Due to the Covid-19 pandemic, only 10 patients could be completed. Of the 10 patients, 5 were male aged 55 – 78 years and 5 were female aged 53 – 80 years, all with idiopathic sensorimotor neuropathy diagnosed. The patients described the typical symptoms of PNP: numbness, burning/burning pain and tingling, foreign body sensation when walking, itching, and a feeling of pressure or even a feeling of stinging. The soles of the feet, the tension and the toes were particularly affected in all patients. All patients experienced significant improvement in symptoms and reported less tingling and pain (Segment 1 p=0.0112 n=8; segment 2 p=0.0058 n=9; segment 3 p=0.0341 n=5; segment 4 p=0.0109 n=5 and segment 5 p=0.0105 n=5) 6 out 10 patients had paraesthesia in the hands and fingers, 4 had a significant improvement (p=0.025). 8 out 10 patients suffered from muscle cramps. A significant improvement has been achieved (p=0.04489). At the end of the study, 6 patients were free of symptoms.
Pain decreased significantly in 7 of 8 patients (p=0.01381). (Figure 1)

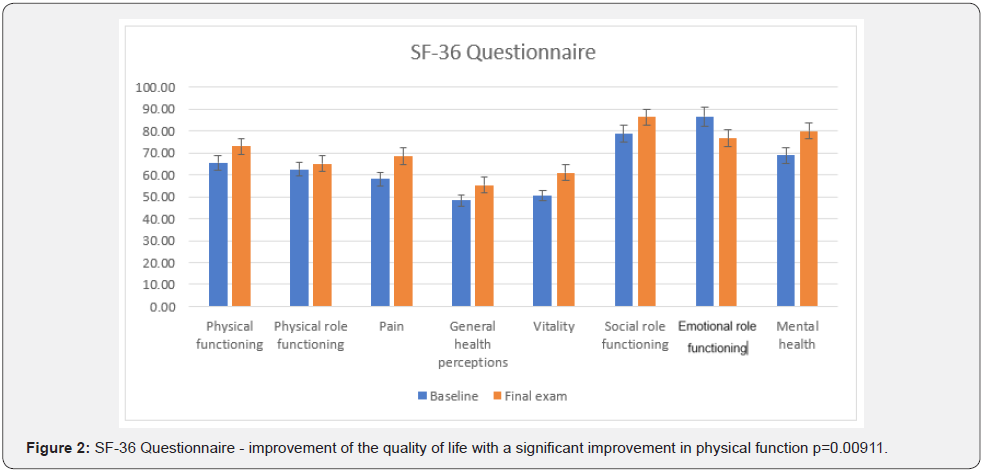
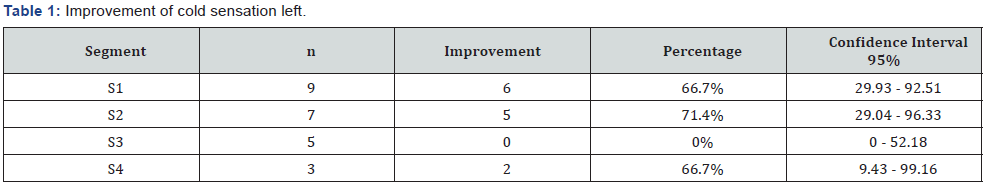
The sensation of cold was restored in at least one segment in 6 patients (60%), the sensation of warmth in 5 patients (50%). (Table 1 & 2)
The sensation of touch was restored in at least one segment on the left leg in 7 patients (70%) and on the right leg in 8 patients (80%).
The sensation of pain was restored in 5 patients (50%) on the left and 6 patients (60%) on the right.
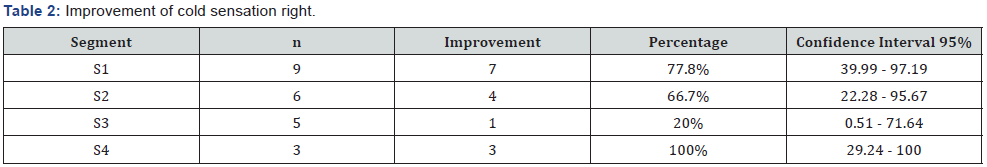
The patients’ quality of life was also improved by the therapy concept. A significant improvement was achieved in the area of physical function (p=0.00911). (Figure 2)
Discussion
Typical symptoms such as numbness, paraesthesia and pain were described by the patients. The symptoms began symmetrically in the feet and rose proximally to partly, stocking height”. Damage to the peripheral nerves leads to sensory disturbances, which may vary depending on the degree and duration of the damaging effect in the peripheral nerve. Improvements in temperature, touch and pain perception were achieved, but confidence intervals are very large due to the low number of patients. With a longer study and more patients, the width of the confidence intervals would decrease, and the values would become more significant.
In the case of chronic diseases such as polyneuropathy, it makes sense to use a combination of acupuncture and phytotherapy [8,9].
The phytotherapy is a major component of TCM. The blends are multi-component blends. The benefits of Chinese herbal therapy are based on thousands of years of experience and the pharmacological effects are still not fully understood. Forouzanfar & Hosseinzadeh [10] suggest in their review from 2018 that the most pathways involved in the analgesic effects of herbal remedies are antioxidant, anti-inflammatory, antiapoptotic, neuroprotective and calcium inhibitory actions [10]. Herbal remedies used in the Lysi-Kush blend are attributed an anti-inflammatory, analgesic, antioxidant, partly neuroprotective effect, and calcium inhibitory actions. Whether even nerve regeneration has taken place would have to be verified in further studies with the measurement of nerve conduction velocity.
Contemporary neural imaging studies have confirmed the importance of the endogenous opioid system and the central nervous system in acupuncture analgesia. Positron emission tomography scans demonstrate that acupuncture produces short- and long-term increases in limbic system μ-opioidbinding potential and reduction in clinical pain [11]. Increased blood circulation to the vasa nerve and the dependent capillary beds that supply the nerve cells may contribute to the effect of acupuncture [12] and thus contribute to the improvement of the symptoms of polyneuropathy. In addition to the analgesic effect of acupuncture, an anti-inflammatory effect is discussed as well as the stimulation of neuroendocrinological and neuroimmunological mechanism and regulatory influence of the adrenal cortex, either by direct nerve activation or indirectly via hypothalamic pituitary glandular axis [8].
Moxa treatment stimulates the hypothalamus and the adrenal cortex and, in addition, local tissue circulation is promoted and the immune system and metabolism are activated [9]. This may increase the positive effects such as pain reduction and antiinflammatory effects. In an experiment with diabetic rats, Yin et. al. found that when Moxa was used at the point St 36, nerve conduction velocity and nerve growth factor concentration increased significantly [13]. This suggests that Moxa exerts a protective function on the peripheral nerves through the expression of nerve growth factors [13].
Quality of life is affected by PNP, mainly by pain, restriction of daily activities and regular tiredness [14]. In this pilot study, quality of life was also affected at the beginning of the study, particularly in the area of general health, pain and vitality. The treatment with TCM had a positive impact on well-being and quality of life. Because of reduction of pain, an improvement in body perception and unsteady gait there was an improvement of quality of life. For a better body perception and unsteady gait Qi Gong may contributed due to an increase in blood circulation. Increased blood circulation, which several research studies support the proposal, enhances delivery of oxygen and nutrients to cells of the body and increases the efficient removal of waste products form the cell. These processes may help nourish diseased or stressed tissue, increasing the efficiency of body functions including immune response, finally enabling the body to heal itself. Qi Gong also may increase the efficiency of delivery of drugs in the bloodstream [15].
There seems to be synergistic effects in the multimodal treatment concept of TCM. In the case of chronic diseases, to which polyneuropathy belongs to, a combined therapy of acupuncture and phytotherapy is useful. [8,9].
More research is required to separate benefits of therapy by phytotherapy, acupuncture and Qi Gong.
Conclusion
The long-term positive effect of TCM was shown by the followup examination (average 15 weeks after the end of treatment). Further research is needed to determine whether the positive effect lasts longer and whether nerve fibers may regenerate. But the data suggest that there is a positive effect of TCM in idiopathic polyneuropathy. It has been shown that the multimodal concept of TCM can be clinically useful in polyneuropathy patients who have not responded to conventional pharmaceutical therapies.
Acknowledgements
The author wishes to thank the Klinik am Steigerwald in Germany for this Pilot-Study for supporting this work.
Conflict of Interest
The author declares no conflict of interest.
References
- Sommer C, Geber C, Young P, Frost R, Frank B, et al. (2018) Polyneuropathien Ursachen. Dtsch Arztebl Int 115: 83-91.
- Heuß D (2019) Diagnostik bei Polyneuropathien, S1-Leitlinie Deutsche Gesellschaft fur Neurologie (Hrsg).
- McLeod J, Tuck R, Pollard J, Cameron J, Walsh J (1984) Chronic polyneuropathy of determined cause. J Neurol Neurosurg Psychiatry 47(5): 530-535.
- Singer MA, Vernino SA, Wolfe GI (2012) Idiopathic neuropathy: new paradigms, new promise. Journal of the Peripheral Nervous System 17(Suppl): 43-49.
- Schröder S, Liepert J, Remppis A, Greten JH (2007) Acupuncture treatment improves nerve conduction in peripheral neuropathy.Eur J Neurol 14(3): 276-281.
- Attal N, Bouhassira D (2015) Pharmacotherapy of neuropathic pain: which drugs, which treatment algorithms? Pain 156(Suppl 1): 104-114.
- Warendorf_J, Vrancken_AFJE, van Schaik_IN, Hughes_RAC, Notermans_NC (2017) Drug therapy for chronic idiopathic axonal polyneuropathy. Cochrane Database of Systematic Reviews.
- Bachmann J (2008) Chinese medicine in orthopedics (1st Edn) Elsevier GmbH, Urban Fischer Verlag, München, Germany.
- Strich R, Rarreck T, Zhang Z (2011) TCM in der Sportmedizin. Karl F Haug Verlag in MVS Medizinverlage Stuttgart GmbH & Co. KG, Stuttgart, Germany.
- Forouzanfar F, Hosseinzadeh H (2018) Medicinal herbs in the treatment of neuropathic pain: a review. Iran J Basic Med Sci 21(4): 347-358.
- Dorsher PT (2011) Acupuncture for chronic pain. Techniques in Regional Anesthesia and Pain Management 15(2): 55-63.
- Litscher G, Wang L, Huber E, Nilsson G (2002) Changed skin blood perfusion in the fingertip following acupuncture needle introduction as evaluated by laser Doppler perfusion imaging. Lasers in medical science 17(1): 19-25.
- Piao Y, Liang X (2012) Chinese Medicine in Diabetic Peripheral Neuropathy: Experimental Research on Nerve Repair and Regeneration. Evid Based Complement Alternat Med Article ID 191632: 13.
- Zis P, Sarrigiannis PG, Rao DG, Hewamadduma C, Hadjivassiliou M (2016) Chronic idiopathic axonal polyneuropathy: a systematic review. J Neurol 263(10): 1903-1910.
- Sancier KM (1999) Therapeutic Benefits of Qigong Exercises in Combination with Drugs. Journal of Alternative and Complementary Medicine 5(4): 383-389.






























