Effect of Changbudodam-tang with Acupuncture in Treatment of Poly Cystic Ovarian Syndrome: A Case Series
Sujin Shin1, Yeji Shin2 and Kyungjin Lee3*
1Department of Korean Medicine, Graduate School, Kyung Hee University, Korea
2She’s Oriental Medicine Clinic, Korea
3Department of Herbal Pharmacology, College of Korean Medicine, Kyung Hee University, Korea
Submission: February 15, 2021; Published: March 02, 2022
*Corresponding author: Kyungjin Lee, Department of Herbal Pharmacology, College of Korean Medicine, Kyung Hee University, Korea
How to cite this article: Sujin S, Yeji S, Kyungjin L. Effect of Changbudodam-tang with Acupuncture in Treatment of Poly Cystic Ovarian Syndrome: A Case Series. J Complement Med Alt Healthcare. 2022; 11(4): 555816. DOI: 10.19080/JCMAH.2022.11.555816
Abstract
Background: Polycystic ovarian syndrome (PCOS) is a common endocrine disorder in women and can lead to complications associated with the reproductive system and metabolism. Current treatments such as metformin and oral contraceptive pills are controversial in terms of effectiveness and side effects. In traditional Korean medicine, Changbudodam-tang (CDT) is used in patients with PCOS, particularly in obese women for the management of hormone and lipid levels. Moreover, low-frequency electronic acupuncture (EA) specifically affects PCOS symptoms by reducing insulin resistance and modulating endogenous regulatory systems. However, there have been few published studies in which CDT and acupuncture were used together for the treatment of PCOS in obese patients. Herein, we report nine cases of obese women with PCOS who were treated with CDT and acupuncture.
Methods: Patients were assessed for the duration of menses, size of the follicle and ovulation, body mass index (BMI), and percent body fat.
Results: CDT and acupuncture treatment resulted in a decrease in weight and BMI, and showed recovery or improvement of the menstrual cycle in the state of amenorrhea or oligomenorrhea.
Conclusion: This study showed that CDT with acupuncture may be considered as an alternative treatment for obese women with PCOS.
Keywords: Polycystic ovary syndrome; Traditional Korean medicine; Changbudodam-tang; Acupuncture therapy; Case reports
Introduction
Polycystic ovarian syndrome (PCOS) is a common endocrine disorder [1,2] in women with its prevalence between 6% and 10% [1,3,4]. Women with PCOS have reproductive abnormalities such as menstrual cycle disturbance [5], infertility [6], and metabolic disorders such as marked insulin resistance (IR) [7], type 2 diabetes mellitus [2], dyslipidemia [8], and cardiovascular disease [9]. Studies have demonstrated that obesity significantly exacerbates the metabolic and reproductive systems in PCOS [10]. It is also known that IR, which leads to compensatory hyperinsulinemia, plays a key role in the pathogenesis and development of PCOS [11]. Insulin-sensitizer, such as metformin and oral contraceptive pills (OCPs) are used to treat PCOS to reduce hyperinsulinemia and correct metabolic abnormalities [12,13]. However, side-effects such as nausea, vomiting, and diarrhea are commonly observed in patients using metformin [14], and long-term usage of OCP can evoke liver toxicity, venous thromboembolism, or cardiovascular disease [15].
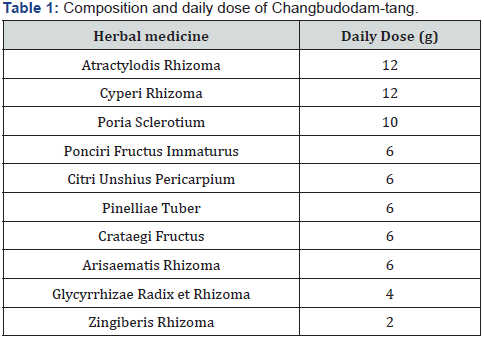
Due to these limitations of current treatment, there is a growing interest in traditional medicine (TM) as an alternative. Recent studies have demonstrated that several herbal formulas targeting PCOS have beneficial effects in treating oligomenorrhea, amenorrhea, and hyperandrogenism [16]. Changbudodam-tang (CDT), also known as Cangfu Daotan decoction in Chinese, is a commonly used prescription for PCOS, particularly in obese women for the management of hormone and lipid levels [17]. It is composed of Atractylodis Rhizoma, Cyperi Rhizoma, Poria Sclerotium, Ponciri Fructus Immaturus, Citri Unshius Pericarpium, Pinelliae Tuber, Crataegi Fructus, Arisaematis Rhizoma, Glycyrrhizae Radix et Rhizoma, and Zingiberis Rhizoma. In addition, low-frequency electronic acupuncture (EA) specifically affects PCOS symptoms by reducing IR [18] and modulating endogenous regulatory systems [19,20]. However, there have been only few published studies wherein CDT and acupuncture were used for the treatment of obese patients with PCOS. In this study, we report nine cases of obese women with PCOS who showed a decrease in weight and body mass index (BMI) and showed recovery or improvement of the menstrual cycle in the state of amenorrhea or oligomenorrhea with CDT, acupuncture, and lifestyle management.
Methods
Study design
Enrollment of the Patients
This study was conducted in She’s oriental medicine clinic (Seoul, Korea). From August 1, 2018, to July 31, 2021, 115 patients visited the She’s oriental medicine clinic for receiving the treatment for oligomenorrhea or amenorrhea. Among them, 19 patients with PCOS fulfilling the inclusion criteria were initially included in this study. Finally, patients who had been on treatment and had undergone menstrual cycles for more than 2 months were included. Therefore, nine women were included in the evaluation. Before starting the treatment, informed consent was signed by the patients.
Criteria for Inclusion
The following patients were excluded from the trial:
i. Patients with oligomenorrhea or amenorrhea due to causes other than PCOS
ii. Patients with androgen-secreting tumor
iii. Patients with severe thyroid abnormalities
iv. Patients with severe chronic diseases such as cancer, tuberculosis, or cardiovascular disease
Therapeutic intervention
CDT treatment
CDT was used to treat patients with PCOS. The daily dose and composition of CDT are presented in Table 1. Each herbal medicine was purchased from Chungdo Herbal Medicine Co., Ltd. (Guri,Korea) and was prepared by Hamsoa Pharmaceutical Co., Ltd. (Seoul, Korea). Herbal medicines were prescribed every 15 days. Fifteen times of CDT daily dose was boiled with 5.98 L purified water for 40 min, and the filtrate was collected. It was prescribed to be taken after the meal, 100 mL twice a day.
Acupuncture treatment
Patients visited She’s oriental medicine clinic and received acupuncture treatment once a week. Acupuncture was performed by specialists in a Korean oriental medicine way. Acupuncture points were selected from the acupoints which are commly used in gynecological diseases according to the textbook Acupuncture medicine [21]. The acupuncture needle (diameter 0.25 mm, length 30 mm, Dongbang medical, Korea) was inserted at a right angle to a depth of 1.5 cm using a needle tube, and low-frequency EA was administered for 15 min. The acupuncture points selected were as follows: bilateral ST7 (Xiaguan), ST25 (Tianshu), ST 29 (Guilai), SP6 (Sanyinjiao), SP11 (Jimen), TE20 (Jiaosun), and GV22 (Xinhui), CV3(Zhongji), CV4 (Guanyuan), CV6 (Qihai), CV12 (Zhongwan).
Lifestyle management
During the treatment period, patients were advised regarding the dietary habits for reduction of body weight, such as avoiding junk foods and consuming a low-calorie diet that includes low-carb and protein-rich foods. In addition, patients were recommended to exercise for more than 30 min at least 2-3 days a week.
Assessment criteria
At the initial consultation, the menstrual cycle, onset of menstrual period, regularity of the menstrual cycle, and past treatment were investigated using a standardized questionnaire. During each visit, patients were assessed for the duration of menses, size of the follicle, ovulation, and BMI. Regular menstrual cycles were defined as 21-35 days in length. Oligomenorrhea was defined as a menstrual cycle of more than 40 days and amenorrhea was defined as no menstruation in the last 6 months. Ultrasonic scans were performed using the LOGIQ P6 Pro (GE Healthcare, USA) equipped with a GE 4C Convex Probe (Featuring 1.5-4.5 MHz Imaging Frequency) through an abdominal scan. Echo-free round or oval structures in the ovaries were counted as follicles and their sizes were measured. Body weight, percent body fat (PBF), and WHR were measured using an In body 720 (Biospace, Seoul, Korea), following a bioelectrical resistance measurement method. BMI was defined as body weight in kilograms divided by body height in meters squared (kg/m2). Changes in body weight, BMI, and PBF during the treatment period were checked approximately every month. Obesity was defined according to the criteria for the Asia-Pacific region suggested by the World Health Organization (WHO) [22] as follows: normal weight (18.5 ≤ BMI ≤ 22.9 kg/m2), overweight ( 23 ≤ BMI ≤ 24.9 kg/m2), and obese (BMI ≥ 25 kg/m2).
Results
General characteristics of study patients
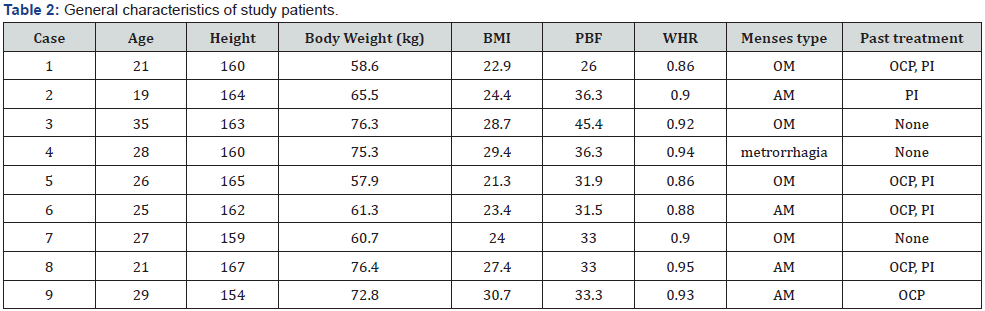
Source: BMI: Body Mass Index; PBF: Percent Body Fat; OM: Oligomenorrhea; AM: Amenorrhea; OCP: Oral Contraceptive Pill; PI: Progesterone Injection; WHR: Waist-to-Hip Ratio.
The general characteristics of the patients included in this study are given in Table 2. The mean age of the nine subjects was 25.7, ranging from 19 to 35 years. PCOS was present in all cases according to the past medical history and current medical condition. Regarding oligomenorrhea or amenorrhea, there were four cases each of oligomenorrhea and amenorrhea and one case of metrorrhagia (intermenstrual bleeding). Six patients received treatments such as OCP and progesterone injection to manage menstrual cycle and hyperandrogenism; however, the treatment was unsuccessful. Three patients had not received any treatment in the past. In terms of obesity, four patients were obese with BMI > 25 kg/m2, three patients were pre-obese with BMI ranging from 23-24.9 kg/m2, and two patients had BMIs within the normal range. However, the WHR of these two patients was above 0.85, which is defined as abdominal obesity according to the WHO criteria [23].
Changes before and after treatment
Treatment period and follow-up period
All patients received treatment for more than 3 months. Three patients received CDT treatment for 4 weeks, five patients for 12 weeks, and one patient for 24 weeks. The patients received acupuncture treatment and lifestyle management during the period of absence of CDT treatment.
Change in Body weight, BMI, PBF
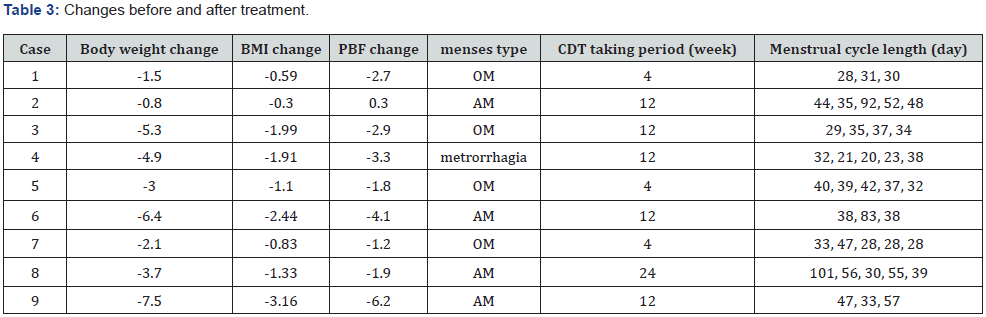
Source: BMI, Body Mass Index; PBF, Percent Body Fat; OM, Oligomenorrhea; AM, Amenorrhea; CDT, Changbudodam-tang.
All patients showed a decrease in weight. The average change in body weight was -3.91 kg. Accordingly, the BMI of all the patients was reduced. The average change in BMI was -1.52 kg/ m2. In addition, the PBF of all the patients decreased. The average change in PBF was -2.64. Changes in Body weight, BMI, PBF of the patients are given in Table 3.
Changes in the menstrual cycle
Within the treatment period, the normal menstrual cycle was restored in all cases. The average interval between the two menses was 42.55 days after treatment. Changes in the menstrual cycle of the patients are given in Table 3. Ultrasound confirmation revealed that the menstrual patterns of all patients changed from anovulatory menstruation to ovulatory menstruation.
Discussion
We report nine cases of obese women with PCOS who showed a decrease in body weight and BMI and depicted recovery or improvement of the menstrual cycle in the state of amenorrhea or oligomenorrhea with CDT treatment and acupuncture. In this study, nine patients who were diagnosed with PCOS using the Rotterdam criteria and had received treatment for more than 2 months were included. Changes in the menstrual cycle and ovulation corresponding to weight change were checked. With regards to obesity, comparisons were made using body weight, BMI, and PBF. Obesity is associated with IR and compensatory hyperinsulinemia, and with multiple factors that may affect hypothalamic-pituitary function, metabolism, or regulators of sex steroids [24]. Studies have also suggested that obese women are more likely to be insulin resistant than their lean counterparts [25], and are more likely to be anovulatory. Moreover, they experience abnormal menstrual cycles [26]. Weight loss in obese patients induces significant reductions in C-reactive protein and interleukin-6 concentrations in relation to IR improvement [27]. Therefore, lifestyle interventions to lose weight, such as dietary control and exercise, are recommended as first-line treatment in overweight patients with PCOS [28]. In this study, all patients showed a decrease in weight after the treatment. The average change in body weight was -3.91 kg. Accordingly, the BMI and PBF of all patients were reduced. The average change in BMI and PBF was -1.52 kg/m2 and -2.64. Weight loss and reduction of BMI and PBF seem to have an effect on normal menstrual cycle recovery in PCOS patients.
Within the treatment period, the normal menstrual cycle was restored to an average of 42.55 days. Also, ultrasound confirmation revealed that the menstrual patterns of patients changed from anovulatory menstruation to ovulatory menstruation. Hyperinsulinemia stimulates androgen production in the ovarian theca cells by acting as a co-gonadotropin [29] and increasing the release of luteinizing hormone [30]. Herbal medicines used in TM can improve the symptoms of patients by simultaneous actions on various body organs. Moreover, different herbal compounds may show synergistic interactions [31]. CDT is a commonly used prescription for the treatment of PCOS, particularly in obese women, for the management of hormone and lipid levels [17]. Studies show that CDT can lower IR, normalize serum hormone levels, improve follicular development and endometrial blood flow, and increase pregnancy rates in infertile patients with PCOS [32]. Also, acupuncture and specifically low-frequency EA affects PCOS symptoms by reducing IR [18] and modulating endogenous regulatory systems such as endocrine system, neuroendocrine system, and the sympathetic nervous system without any negative side effects [19,20].
In conclusion, our study depicted that the normal menstrual cycle was restored in all patients within the treatment period. Patients’ menstrual cycles appeared to have normalized because they lost weight and had lower IR. Moreover, because acupuncture is related to the reduction of androgen levels, it may affect the normalization of follicular growth and maturation processes, and hence lead to ovulation [32]. Therefore, this study showed that CDT with acupuncture may be considered as an alternative treatment for obese women with PCOS. However, our study has certain limitations. First, as a retrospective case series study, it was difficult to set the conditions for treatment to the patients from the beginning and to provide treatment for the same period. Second, it was not confirmed whether the blood test findings had improved. Third, the changes in the menstrual cycle after the treatment period could not be continuously observed in all cases. More diverse case reports in the future are warranted for considering CDT with acupuncture treatment as an alternative when obesity is combined with oligomenorrhea, amenorrhea, and infertility.
References
- Ricardo A, Keslie SW, Reyna R, Key JT, Eric SK, et al. (2004) The prevalence and features of the polycystic ovary syndrome in an unselected population. The Journal of clinical endocrinology and metabolism 89(6): 2745-2749.
- Dumitrescu R, Mehedintu C, Briceag I, Purcarea VL, D Hudita D (2015) The polycystic ovary syndrome: an update on metabolic and hormonal mechanisms. Journal of medicine and life 8(2): 142-145.
- Asunción M, Calvo RM, Millan JL, Sancho J, Morreale HF (2000) A prospective study of the prevalence of the polycystic ovary syndrome in unselected Caucasian women from Spain. The Journal of clinical endocrinology and metabolism 85(7): 2434.
- Kandarakis ED, Kouli CR, Bergiele AT, Diandra FA, Tsianateli TC (1999) A survey of the polycystic ovary syndrome in the Greek island of Lesbos: hormonal and metabolic profile. The Journal of clinical endocrinology and metabolism 84(11): 4006-4011.
- Balen AH, Conway GS, Kaltsas G, Techatrasak K, Manning PJ, et al. Polycystic ovary syndrome: the spectrum of the disorder in 1741 patients. Human reproduction (Oxford, England) 10(8): 2107-2111.
- Costello MF, Misso ML, Wong J, Hart R, Rombauts L, et al. (2012)The treatment of infertility in polycystic ovary syndrome: a brief update. The Australian & New Zealand journal of obstetrics & gynaecology 52(4): 400-403.
- DeUgarte CM, Bartolucci AA, Azziz R (2005) Prevalence of insulin resistance in the polycystic ovary syndrome using the homeostasis model assessment. Fertility and sterility 83(5): 1454-1460.
- Wild RA, Painter PC, Coulson PB, Carruth KB, Ranney GB (1985) Lipoprotein lipid concentrations and cardiovascular risk in women with polycystic ovary syndrome. The Journal of clinical endocrinology and metabolism 61(5): 646-951.
- Meyer C, McGrath BP, Teede HJ (2005) Overweight women with polycystic ovary syndrome have evidence of subclinical cardiovascular disease. The Journal of clinical endocrinology and metabolism 90(10): 5711-5716.
- Lim SS, Norman RJ, Davies MJ, Moran LJ (2013)The effect of obesity on polycystic ovary syndrome: a systematic review and meta-analysis. Obesity reviews : an official journal of the International Association for the Study of Obesity 14(2): 95-109.
- Kandarakis ED, Dunaif A (2012) Insulin resistance and the polycystic ovary syndrome revisited: an update on mechanisms and implications. Endocrine reviews 33(6): 981-1030.
- Nardo LG, Rai R (2001) Metformin therapy in the management of polycystic ovary syndrome: endocrine, metabolic and reproductive effects. Gynecological endocrinology : the official journal of the International Society of Gynecological Endocrinology 15(5): 373-380.
- Teede H, Tassone EC, Piltonenet T, Malhotra J, Mol BW, et al. (2019) Effect of the combined oral contraceptive pill and/or metformin in the management of polycystic ovary syndrome: A systematic review with meta-analyses. Clinical endocrinology 91(4): 479-489.
- Bouchoucha M, Uzzan B, Cohen R (2011) Metformin and digestive disorders. Diabetes & metabolism 37(2): 90-96.
- Domecq JP, Prutsky G, Mullan RJ, Sundaresh V, Wang AT, et al. (2013) Adverse effects of the common treatments for polycystic ovary syndrome: a systematic review and meta-analysis. The Journal of clinical endocrinology and metabolism 98(12): 4646-4654.
- Arentz S, Abbott JA, Smith CA, Bensoussan A (2014) Herbal medicine for the management of polycystic ovary syndrome (PCOS) and associated oligo/amenorrhoea and hyperandrogenism; a review of the laboratory evidence for effects with corroborative clinical findings. BMC complementary and alternative medicine 14: 511.
- Weimin Y, Xue L, Chen K, Min Z, Cai X, et al. (2021) Effects of Cangfu Daotan Decoction on obese polycystic ovary syndrome and its mechanism. Steroids 165: 108740.
- Kim SK, Lee G, Shin M, Han JB, Moon HJ, et al. (2006) The association of serum leptin with the reduction of food intake and body weight during electroacupuncture in rats. Pharmacology, biochemistry, and behavior 83(1): 145-149.
- Victorin ES, Mannerås L, jedel E (2008) Acupuncture in polycystic ovary syndrome: current experimental and clinical evidence. Journal of neuroendocrinology 20(3): 290-298.
- Andersson S, Lundeberg T (1995) Acupuncture--from empiricism to science: functional background to acupuncture effects in pain and disease. Medical hypotheses 45(3): 27-281.
- World Health Organization. Regional Office for the Western Pacific. (2000). The Asia-Pacific perspective : redefining obesity and its treatment. Health Communications Australia.
- World Health Organization. (2011). Waist circumference and waist-hip ratio : report of a WHO expert consultation, Geneva, 8-11 December 2008.
- Legro RS (2012) Obesity and PCOS: implications for diagnosis and treatment. Seminars in reproductive medicine 30(6): 496-506.
- Dunaif A, Segalet KR, Futterweit W, Dobrjansky A (1989) Profound peripheral insulin resistance, independent of obesity, in polycystic ovary syndrome. Diabetes 38(9): 1165-1174.
- Naderpoor N, Shorakae S, Joham A, Boyle J, Courten B, et al. (2015) Obesity and polycystic ovary syndrome. Minerva endocrinologica 40(1): 37-51.
- Kopp HP, Kopp CW, Festa A, Krzyzanowska K, Kriwanek S, et al. Impact of weight loss on inflammatory proteins and their association with the insulin resistance syndrome in morbidly obese patients. Arteriosclerosis, thrombosis, and vascular biology 23(6): 1042-1047.
- Lisa JM, Samantha KH, Robert JN, Teede JL (2011) Lifestyle changes in women with polycystic ovary syndrome. The Cochrane database of systematic reviews 3(3): CD007506.
- Barbieri RL, Makris A, Randall RW, Daniels G, Ryan KJ, et al. (1986) Insulin stimulates androgen accumulation in incubations of ovarian stroma obtained from women with hyperandrogenism. The Journal of clinical endocrinology and metabolism 62(5): 904-910.
- Maqbool M, Gani I, Geer MI (2019) Insulin Resistance and Polycystic ovary Syndrome: A Review.
- Williamson EM (2001) Synergy and other interactions in phytomedicines. Phytomedicine : international journal of phytotherapy and phytopharmacology 8(5): 401-409.
- Ding CF, Wang CY, Yang X, Zheng RH, Yan ZZ, et al. (2014) Effect of modified cangfu daotan decoction in improving endometrial receptivity in infertility patients with polycystic ovarian syndrome]. Zhongguo Zhong xi yi jie he za zhi Zhongguo Zhongxiyi jiehe zazhi = Chinese journal of integrated traditional and Western medicine 34(11): 1297-301.
- Julia J, Victorin ES (2013) Polycystic ovary syndrome: effect and mechanisms of acupuncture for ovulation induction. Evidence-based complementary and alternative medicine 2013: 762615.






























