Relation Between Post Stroke Depression (PSD) and CT- Scan and MRI Findings and Estimation of Functional Degradation in Patients 2-7 Months after Stroke
Ghasem Fattahzadeh ardalani1, Parviz Molavi2, Abolfazl Atalu1*, Robab Azizi3 and Morteza Delkhosh Reihany3
1Department of Neurology, Ardabil University of Medical Science, Ardabil,Iran
2Department of Psychiatry, Ardabil University of Medical Sciences, Ardabil,Iran
3Anesthesiologist, Fellowship of palliative care,Tabriz University of Medical Science, Tabriz,Iran
Submission: April 17, 2019; Published: May 06, 2019
*Corresponding author: Abolfazl Atalu, 1-Department of Neurology, Faculty of Medicine, Ardabil University of Medical Science, Ardabil, Iran,
How to cite this article: Fattahzadeh Ardalani Gh, Molavi P, Atalu A, Azizi R, Delkhosh-Reihany M. Relation Between Post Stroke Depression (PSD) and CT- Scan and MRI Findings and Estimation of Functional Degradation in Patients 2-7 Months After Stroke. J Complement Med Alt Healthcare. 2019; 9(3): 555762. DOI:10.19080/JCMAH.2019.09.555762
Abstract
Background: Stroke is a syndrome characterized by acute onset of neurological symptoms for more than 24 hours. PSD is the most common mood disorder in patients that its prevalence in women was more than men. The aim of this study was to determine the relation between PSD and CT-scan and MRI findings and the degree of functional degradation in patients after the stroke.
Methods: This descriptive-analytical study was performed on patients with stroke. All of them had depression based on Beck’s depression test. Necessary information including cardiovascular risk factors, type of ischemia, involved hemisphere, involved artery and extent of conflict were recorded in a checklist and the functional degradation in patients is calculated by scores of the Modified Rankin Scale (MRS). Collected data analyzed by statistical methods in SPSS version 21.
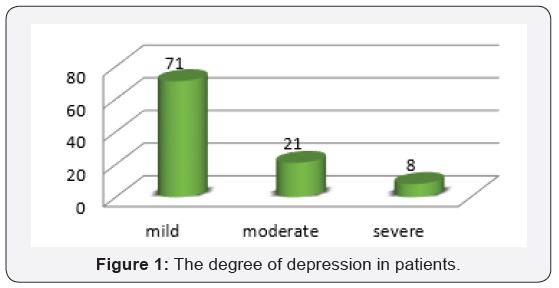
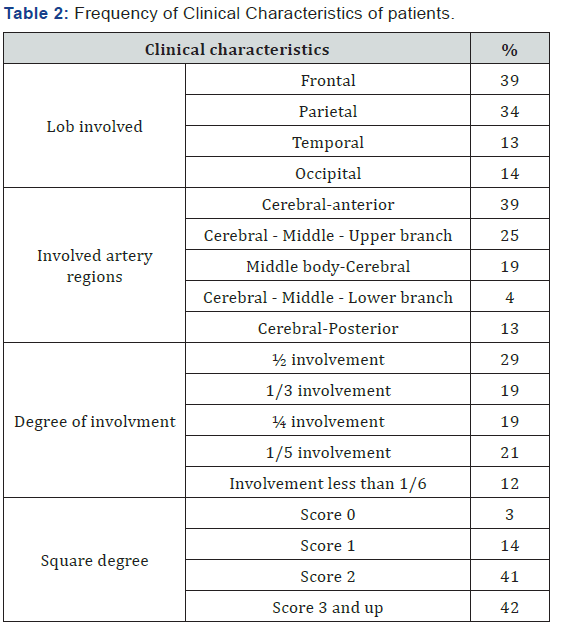
Results: In this study, 100 patients (43 males and 57 females with an average age of 63.97 years) were studied. Of all patients, 71% had mild depression. Of all patients, 80% had ischemic lesions, 56% had involvement in right hemisphere, 39% in frontal and 39% in the cerebral- anterior.
Conclusion: The results showed that depression in women is more than men. The prevalent degree of depression was mild, the form of stroke was ischemic type and the most area involved was right hemisphere of the brain.
Keywords: Stroke; Depression; Ischemia; Hemorrhage
Introduction
Cerebrovascular disease is an acute neuropathic disorder caused by abnormal blood flow to a part of the brain tissue that occur due to brain vessel obstruction as a result of blood coagulate or a rupture one of its feeding vessels. Post stroke depression is the most common and important neuropsychiatric consequences of stroke, which can result in longer hospital stay, compromise the effectiveness of rehabilitation, and reduce the patient’s quality of life [1]. According to the WHO report, the four main reasons for mortality in 2030 will be heart failure, stroke, chronic obstructive pulmonary disease and lower respiratory tract infections. Stroke is a non-communicable disease among the elderly population that is the third leading cause of death in developed countries after coronary artery diseases and cancers [2]. The stroke is divided into two types of ischemic and hemorrhagic. Ischemic type is the most common cause of strokeand caused by formation of a localized clot or an embolism from another place such as the heart.3 Multiple risk factors such as systolic and diastolic hypertension, hypercholesterolemia , using smoking , alcohol and oral contraceptive pills, diabetes, and genetic factors have main role in the incidence of stroke but most of the strokes are multi factorial which influenced by polygenic and environmental factors [3]. The occurrence of stroke leads to occupational, social and mood disorders in patients. The PSD is the most common mood disorder in patients with stroke. The prevalence of PSD is estimated to be about 41.3% [4-5]. Depression is one of the disabling psychological complications of stroke which has devastating effects on all social, occupational, interpersonal, emotional and cognitive aspects of patients. PSD is common and several risk factors such as the location of the lesions in the left hemisphere, female gender, younger agegroup, history of depression and stroke and being alone are related to PSD. The most likely occurrence of depression occur in the first 2 years after stroke and its pick is in the first 3 to 6 months [6-7]. Some of studies have suggested depression as the main cause of death in stroke patients.7 Also female gender , age less than 60 years old , live alone, divorce, alcoholism , inability to return to work, decreased social activity , change in communication with others and size of brain lesions are the risk factors for post stroke depression [4,6-7]. Studies have shown that the use of antidepressants has reduced the incidence of stroke complications and improved its outcome. Therefore, timely diagnosis of depression and quick actions in its treatment are effective in reducing recurrence of stroke, mortality and improving the quality of life of patients [6,8]. Considering the importance of post stroke depression in the prognosis of patients and its mortality and also considering the burden of disease, the aim of this study was to investigate the relation between PSD and CT-scan and MRI findings and estimation of functional degradation in patients 2 to 7 months after stroke.
Method
This descriptive analytical study was done on 100 patients with post stroke depression who hospitalized in the neurology department of Alawi hospital in Ardabil city in 2016. Stroke confirmation was performed by a neurologist based on clinical symptoms and imaging. We used beck questionnaire included 21 questions about physical, behavioral and cognitive symptoms of depression. The questions in this questionnaire were scored based on 0-3 and the degrees of depression were classified from mild to severe. To determine the degree of functional degradation (degree of disability and dependency) we used Modified Rankin Scale (MRS) which included 6 questions with a score of 0-6. The collected data were analyzed by statistical methods in SPSS version 17.
Results
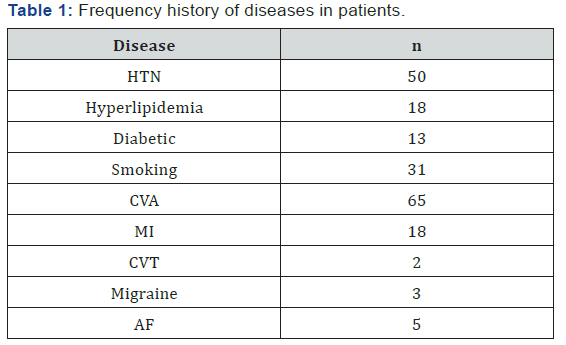
Of all patients, 57% were female and the rest were male. 77% of the patients were over 50 years of age and the average age of the patients were 63.14 ± 14.67 years (range 32-86). In 80% of patients the stroke was ischemic, and the rest was hemorrhagic. 56% of the patients had right hemisphere involvement and the rest of them had left hemisphere involvement. 71% of patients had mild depression (Figure 1). 18% of patients had a historyof myocardial infarction, 50% hypertension and 65% had CVA for the first time (Table 1). The results showed that the most involved lob was the frontal lobe and the most involved artery was the cerebral- anterior region with 39%, respectively. In 29% of patients, 50% of the brain pathway was damaged. The average score of MRS in patients was 2.53±1.25 and the highest degree of disability and dependency was related to score 2 with 41% (Table 2).
Discussion
In this study, 44% of patients had left hemisphere damage, 35% had history of stroke and 57% were women. The results of this study showed that 71% of patients had mild depression and 21% had moderate depression. In Glamkovski et al. [9] study, the prevalence PSD was 66% that of them 51% had mild depression and 15% moderate to severe depression which was lower than the present study [9]. In the study of Robinson et al. [10] the prevalence of major depression was 21.7% and minor depression was 19.5% and in the study of Rajashekaran et al. [11] , the prevalence of major depression was 64.2% and in this study the prevalence of severe depression was 8% which was lower than that of Robinson and Rajashekaran studies [10-11]. In the study of Arseniou et al. [12], the incidence of PSD was reported between 6% to 79% [12]. In Iranmanesh et al. [13] study, the incidence of depression in women was significantly higher than men. In another study by Marie et al. [14] in Sweden, Ohira et al. [15] in Japan, the incidence of PSD was more common in women than in men [13-15]. Similar to other studies in this study, the prevalence of depression was more common in women. The findings of this study showed that the prevalence of PSD in women was more than men and female gender is a risk factor for PSD. In this study, the average age of patients was 63.97 which was similar to the study of Lashkaripoor et al.[16] with an average age of 69.62 [16]. CT- scan and MRI findings showed that 80% of patients had ischemic lesions 56% right hemisphere involvement, 39% frontal involvement and 39% had involvement of the anterior branch of the brain. In the study of Rajashekaran et al. [11], involvement of left cerebral lob lesions was 67.9% and focal and multifocal lesions were 64.3% and 35.7%, respectively [11]. In studies conducted by Sato et al. [18], Srivastava et al. [17] there was no significant relationship between location of lesions in stroke and depression [17-18]. However, in some studies there was a significant relationship between them [19-20]. In this study, more than half of the patients with right hemisphere involvement and most of the patients had ischemic lesion. In Gozzi et al. [21] study, 86% of patients had ischemic stroke and 53% had left lobe involvement. Dalvelan et al [1] in a study on patients in Iran showed that the prevalence of post stroke depression in Iran was 76.9% and was lower than the present study. Ebrahimi Rad et al [22] in a study in Ramsar showed that the prevalence of post stroke depression in patients was 45% which was lower than the present study [22].
Conclusion
It seems that due to the prevalence of mild PSD and its more prevalence among women as compared to men, women need more attention and care to recognizing and treating depression. The results showed that the prevalence of post stroke depression in this province was higher than the national average and it is necessary to identify the possible causes by carefully studying and planning to reduce it in the future.
References
- Dalavand S, Ghanei R (2018) Prevalence of poststroke depression in Iranian patients: a systematic review and meta-analysis. Dovepress pp. 3073-3080.
- Abbasi V, Amani F, Aslanian R, Hoseinkhani A, Zakeri A (2017) Epidemiological Study of Stroke in Ardabil, Iran: A Hospital Based- Study. Journal of Neurological Disorders & Stroke 5(2): 1-5.
- Aminoff MJ, Greenberg D, Simon RP (2015) Clinical Neurology 9/E: McGraw Hill Professional.
- Hasanzadeh R, Hosseini SH, Abedini M, Enayati H (2014) The Relationship of Possible Risk Factors in Prevalence of Post Stroke Depression. Journal of Mazandaran University of Medical Sciences 24(111): 60-66.
- Sun N, Li QJ, Lv DM, Man J, Liu XS, et al. (2014) A survey on 465 patients with post-stroke depression in China. Archives of psychiatric nursing 28(6): 368-371.
- Vogel CH (1995) Assessment and Approach to Treatment in Post‐Stroke Depression. Journal of the American Academy of Nurse Practitioners 7(10): 493-497.
- Bourgeois JA, Hilty DM, Chang CH, Wineinger MA, Servis ME (2004) Post stroke neuropsychiatric illness: an integrated approach to diagnosis and management. Current treatment options in neurology 6(5): 403-420.
- Loubinoux I, Kronenberg G, Endres M, Schumann Bard P, Freret T, et al. (2012) Post‐stroke depression: mechanisms, translation and therapy. Journal of cellular and molecular medicine 16(9): 1961-169.
- Glamcevski MT, Pierson J (2005) Prevalence of and factors associated with post stroke depression: a Malaysian study. Journal of Stroke and Cerebrovascular Diseases 14(4): 157-161.
- Robinson RG, Spalletta G (2010) Poststroke depression: a review. The Canadian Journal of Psychiatry 55(6): 341-349.
- Rajashekaran P, Pai K, Thunga R, Unnikrishnan B (2013) Post-stroke depression and lesion location: a hospital based cross-sectional study. Indian journal of psychiatry 55(4): 343-348.
- Arseniou S, Arvaniti A, Samakouri M (2011) Post-stroke depression: recognition and treatment interventions. Psychiatriki 22(3): 240-248.
- Iranmanesh F, Vazirynejad R, Gadari F, Rajabpoor N (2012) Prevalence of post-stroke depression and its relationship with risk factors for stroke. Journal of Fasa University of Medical Sciences 2(2): 66-70.
- Eriksson M, Asplund K, Glader EL, Norrving B, Stegmayr B, et al. (2004) Self-reported depression and use of antidepressants after stroke: a national survey. Stroke 35(4): 936-941.
- Ohira T, Iso H, Satoh S, Sankai T, Tanigawa T, et al. (2001) Prospective study of depressive symptoms and risk of stroke among Japanese. Stroke 32(4): 903-908.
- Lashkaripour K (2008) Prevalence of post stroke depression and its relationship with disability and lesion location. Journal of Fundamentals of Mental Health 10: 191-199.
- Srivastava A, Taly AB, Gupta A, Murali T (2010) Post-stroke depression: prevalence and relationship with disability in chronic stroke survivors. Annals of Indian Academy of Neurology 13(2): 123-127.
- Sato R, Bryan RN, Fried LP (1999) Neuroanatomic and functional correlates of depressed mood: The Cardiovascular Health Study. American journal of epidemiology 150(9): 919-929.
- Singh A, Black SE, Herrmann N, Leibovitch FS, Ebert PL, et al. (2000) Functional and neuroanatomic correlations in post stroke depression: the Sunnybrook Stroke Study. Stroke 31(3): 637-644.
- Shimoda K, Robinson RG (1999) The relationship between post stroke depression and lesion location in long-term follow-up. Biological Psychiatry 45(2): 187-192.
- Gozzi SA, Wood AG, Chen J, Vaddadi K, Phan TG (2014) Imaging predictors of post stroke depression: methodological factors in voxelbased analysis. BMJ open 4(7): e004948.
- Ebrahimi Rad R, Nasiri M, Gholizadeh B, Arabpour M, Fotokian Z, et al. (2016) Study prevalence and risk factors for early post stroke depression. ZJUMS 24: 115-124.






























