Clinical Analysis of PetCO2 in Predicting Abdominal Lifting and Compression CPR
Hong wei Wang1, Sisen Zhang1*, Ying xin Cen1, XinSha1, Wei Song 2, JingLi3 and Lixiang Wang4
1Department of Emergency, Southern Medical University Affiliated Zhengzhou People's Hospital, China
2Hainan Provincial People's Hospital Emergency Medical Center, China
3Beijing Germari Medical Equipment Co., China
4Emergency Medical Center, General Hospital of Chinese Armed Police Forces, China
Submission: July 26, 2017; Published: August 16,2017
*Corresponding author: Zhang Sisen, Department of Emergency, Southern Medical University Affiliated Zhengzhou People's Hospital, China, Tel: 13937-120-886; Email: 2362176700@qq.com
How to cite this article: Hong w W, Sisen Z, Ying x C, Xin S, Wei S, Jing L, Lixiang W. Clinical Analysis of PetCO2 in Predicting Abdominal Lifting and Compression CPR. J Complement Med Alt Healthcare. 2017; 3(3): 555611. DOI: 10.19080/JCMAH.2017.03.555611
Abstract
Objective: To analyse clinical effect of partial pressure of end-tidal carbon dioxide (PetCO2) in evaluating and predicting abdominal lifting and compression CPR(ALP-CPR).
Methods: 92 patient of cardiac arrest were in tubated and received ALP-CPR performed with a novel abdominal lifting/compression device by monitoring HR, PaO2, PaCO2 and PetCO2 according to the ultimate outcome of CPR, patients were divided into success group and failure group, the number of patients with 30min and 60min survival and the time of ROSC were recorded in successful group, and calculated the recovery success rate. Data according to the Utstein criteria, demographic information, medical data. we hypothesized that an PetCO2 level of 2.67kPa (20mmHg) or more after 20 minutes of standard advanced cardiac life support would predict ROSC.
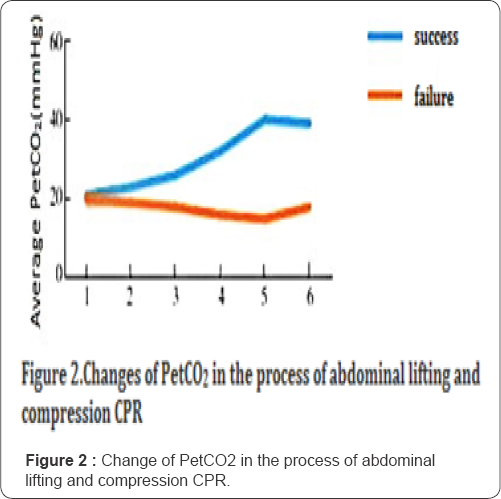
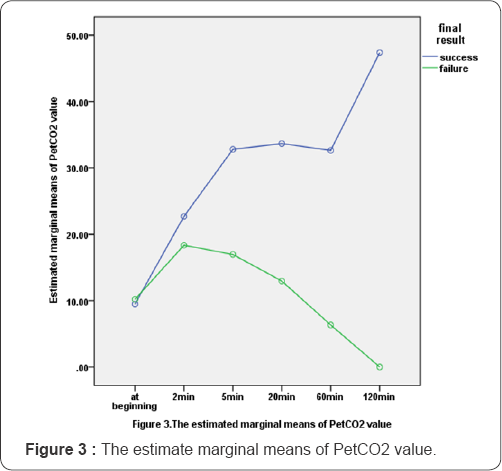
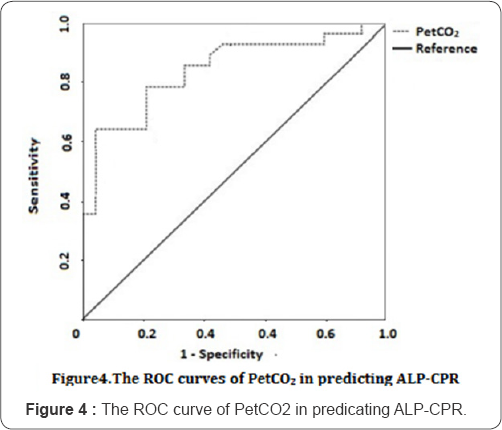
Results: At beginning of ALP-CPR, PetCO2 of both groups were about 9~10mmHg. PetCO2 was gradually rising in successful group during ALP-CPR process and increased slightly at 2~5min after ALP-CPR, then progressively decreased in failure group(P<0.05). PetCO2 values of 2.67kPa (20mmHg) or less discriminated between 37patients with ROSC and 55 patients without (P<0.05), but the successful recovery rate at 60 min after ROSC was 17.4% (16/92) in successful group. The difference of MAP, PaO2 and PaCO2 after ROSC 20min compared with abdominal lifting and compression CPR process was statistically significant (P<0.05), area under the receiver operating characteristic curve(95%CI) is 0. 845, the sensitivity and specificity were respectively 0.80,0.83.
Conclusions: The variation of PetCO2 value can be used as a clinical index to evaluate and predict the effect of ALP-CPR, and PetCO2 levels of more than 2.67kPa (20mmHg) after 20 minutes may be used to predict ROSC. The ROSC time is positive correlation with the ROSC rate.
Keywords: Abdominal lifting and compression; Cardiopulmonary resuscitation; Restoration of spontaneous circulation; The end tidal carbon dioxide partial pressure
Introduction
Early high quality and effective cardiopulmonary resuscitation (CPR) is the only effective first-aid measure to treat CA patients and improve their survival rate according to the current American Heart Association and European Resuscitation Council (ERC) CPR Guidelines. Consistent and discouraging low survival rates mandate are assessment of current resuscitative strategies and techniques [1-4]. We have invented a new device that could enhance abdominal wall lifting and compression, which made up for the lack of chest compressions (chest wall trauma or rib fracture). Clinical tests on this device show that it could reach a higher survival rate compared to chest compression in patients with cardiac arrests [5]. More studies are required to fully evaluate this abdominal lifting and compression boosting device before it can be recommended for widespread clinical use, and the most common of all decisions after initiation of CPR remains the decision of when to stop. Various clinical indicators have been used to determine when CPR efforts should be terminated [6-8]. Capnography (capnometry) potentially represents a useful clinical indicator of death that could guide decisions to terminate resuscitative efforts [9-10]. We sought to evaluate the hypothesis that partial pressure of PetCO2 can evaluate and predict non survival in an independent cohort of patients suffering cardiac arrest. In the current study, we aim to seek a high sensitivity, specificity, predictive value and efficient method to evaluate and predict the CA patients be treated by ALP-CPR. We report our results here.
Materials and Methods
Patients
This was a prospective study conducted at emergency medical center of Zhengzhou People's Hospital and Hainan province People's Hospital from September 2014 to October 2016. A total of 92 patients who suffered a sudden cardiac arrest and were treated by a mobile emergency team were included in the present prospective study. The effectiveness, safety, and stability of the abdominal lifting and compression device used in this study have been verified in animal and human experiments [11]. This study was also approved by the Ethical Review Committee of Zhengzhou People's Hospital and Hainan province People's Hospital. All patient relatives or legal guardians received a detailed explanation of the study's possible risks and benefits and were permitted to request discontinuation of the study at any time. The requirements of the Declaration of Helsinki were strictly upheld throughout the research process. It was required that a close relative or legal guardian of the patient provide written informed consent to participate in the study.
The criteria include:
i. Conforms to the ALP-CPR indications and had no contraindications. Indications include: Chest trauma caused cardiac arrest, respiratory muscle well weakness, and respiratory suppression of general anesthesia, especially thoracic deformity, chest fracture (including chest rib fractures appeared in the process of recovery, etc.), hemopneumothorax, and chest compression indication.
ii. Contraindications include: external injury to the abdomen, rupture of the diaphragm, bleeding in the abdominal cavity or internal organs, abdominal aortic aneurysm, and large tumor in the abdominal cavity, injury to the abdominal cavity or internal organs during abdominal compression, massive abdominal mass(such as pregnancy, intestinal obstruction, abdominal organ tumors, a large amount of ascites, giant ovarian cysts), etc.
Exclusion criteria:
i. Contraindication to the use of ALP-CPR, no indication for resuscitation or a do not resuscitate order.
ii. Disease that might significantly affect assessment of effectiveness (e.g., chronic wasting diseases such as malignancy or severe tuberculosis) and informed consent not obtained. Adults of both genders with a body weight of 40~150 kg meeting American Heart Association (AHA) guidelines for cardiopulmonary arrest seen in the emergency department were eligible for inclusion [12].
Study design
In compliance with 2016 expert consensus on ALP- CPR and the 2010 American heart association (AHA) guidelines,AmodelCPR-LW1000abdominallifting/compression device (patent number: ZL 2009 2 0164343.6,ZL 2009 2 0160376.3,ZL 2014 3 0044027.1) invented by Professor Li-xiang Wang of the General Hospital of Armed Police Forces' Emergency Medical Center and produced by the Beijing Germari Medical Equipment Co., Ltd., was used to perform ALP-CPR [13] (details of the study are reported in the Appendix). Detailed operation method introduction: a display panel, pressure application handles, and a negative pressure device make up of the device. Operators hold the pressure application handles and place the compression plate on the patient's abdomen. After turning on the device, negative pressure is generated which causes a tight bond between these pressure plates and the patient's abdomen. The operator then presses an indicator light prompted by an audio signal with a frequency of 100 times/minute, and the instrument performs alternate vertical downward compressions and upward lifting actions. The duration of compression and lifting was performed in a 1:1 ratio, the pressure was approximately 186 mmHg when the indicator light was on, and lifting force was approximately 112 mmHg. All patients were intubated and an end tracheal tube was immediately connected to the capnometer, multi-function cardiograph monitor was dynamically monitored. We monitored PetCO2 continuously and recorded it during ALP-CPR, Measurements of PetCO2 were taken using the side stream method with the infrared capnometer integrated into the LIFEPACK 12 defibrillator monitor or with BCI Capnocheck Model 20600A1.
Observational index
Multi-function cardio monitor, CO2 detector and other equipment monitoring to evaluate ALP-CPR effect; The commissioner collected and recorded the information before, during and after resuscitation, and the professional statisticians analyze the parameters of ROSC. We defined return of spontaneous circulation (ROSC) in accordance with the Utstein style ('any ROSC'-palpabile pulse on carotid artery, regardless of duration, and ROSC with admission to hospital).Termination of lifesaving treatment: lifesaving treatment was considered successful and terminated with the appearance of an autonomous aortic pulse, moist facial complexion, the appearance of autonomous respiration, and shrinking pupils and reappearance of a light reflex, or the appearance of eyeball motion and limb spasms [14]. If after continued routine lifesaving efforts for at least 30 minutes no pulse or autonomous breathing was noted, lifesaving treatment was terminated after obtaining informed consent from family members.
Monitoring index
Heart rate (HR), MAP, PaO2, PaCO2 were measured during pre- CPR, CPR, and post-CPR periods, and PetCO2 was also monitored at different times, dynamically. Life at 30 and 60 minutes after ROSC was also recorded.
Statistical analysis
Descriptive statistics are presented as meantstandard deviation for continuous variables. Analysis for caterogical variables were performed using X2 test and exact Fisher test. Comparisons between groups were performed using t-test (normal distribution) and shapiro-Francia test (normality test failed). For PetCO2, Sensitivity and specificity were calaculated using standard formulae, multivariate analysis of repeated measurements with PetCO2 at different time, receiver operating characteristic (ROC) curves were obtained. The greater the area under the ROC curve (AUROC), the better the predictive value of PetCO2, All statistical tests were two-sided with significance, the null hypothesis was considered to be rejected at P values less than 0.05 in all tests. All analyses were performed using SPSS 19 statistical software (IBM Corp., Armonk, NY, USA).
Results
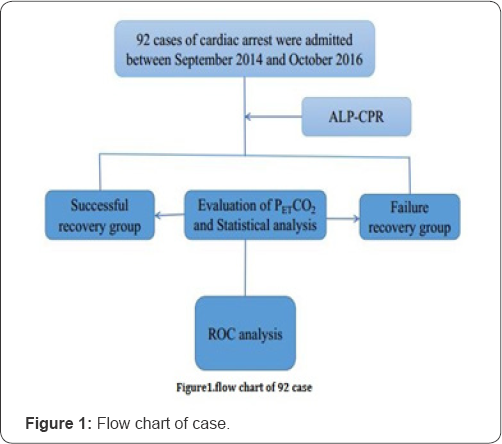
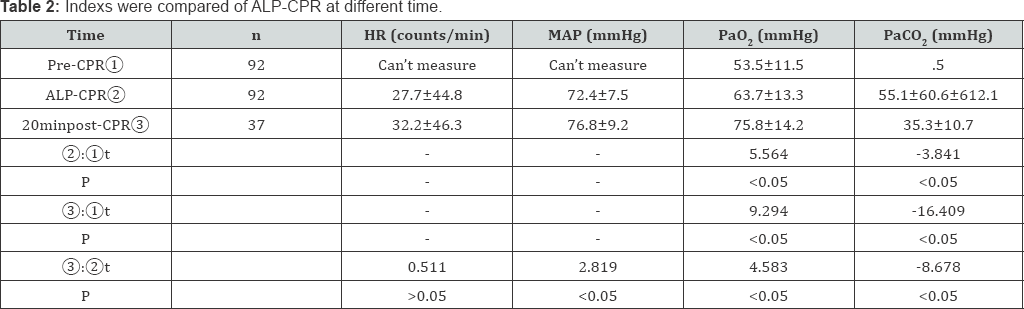
During the period of evaluation, our centre was involved in 92 emergency interventions in which there was absence of signs of circulation at the start of intervention. Ultimately, 37patients were resuscitated.20min after ROSC was achieved in 37 patients (40.2%). yet, by the binomial distribution theory, 30 and 60min after ROSC overall survival to hospital admission occurred in 17.4% (16 patients), which has no statistically significant difference with 17.5% (7/40) [15] in pre-experiment (P>0.05). patients' HR, MAP, PaO2 and PaCO2 were significantly improved during ALP-CPR (P<0.05). 20min after ROSC MAP, PaO2 and PaCO2 were all higher than those in the ALP-CPR process (P<0.05) (Table 1) At beginning of ALP-CPR, PetCO2 of both groups were about 9 " 10mmHg (P>0.05). PetCO2 was gradually rising in success group during ALP-CPR process and increased slightly at 2~5min after ALP-CPR, then progressively decreased in failure group (P<0.05). PetCO2 values of 2.67kPa (20mmHg) or less discriminated between the 37 patients with ROSC and 55 patients without (P<0.05), but the success recovery rate at 60 min after ROSC was 17.4% (16/92) in successful group. The difference of MAP, PaO2 and PaCO2 after ROSC 20min compared with abdominal lifting and compression CPR process was statistically significant (P< 0.05).When a 20minute PetCO2 value of 2.67 kPa (20mmHg) or less was used as a screening test to predict ROSC, area under the receiver operating characteristic curve (95%C1) is 0.845, the sensitivity and specificity were respectively 0.80, 0.83 (Figure 1-4) Table 2 ROSC, return of spontaneous circulation; ALP-CPR, abdominal lifting and compression cardiopulmonary resuscitation. ALP-CPR, abdominal lifting and compression cardiopulmonary resuscitation; HR, heart rate; MAP, mean arterial pressure; PaO2, arterial oxygen partial pressure; PaCO2, arterial partial pressure of carbon dioxide;1 mmHg=0.133 kPa.

Discussion
In 2015 CPR guidelines of American Heart Association recommend that the primary goals of patients with CA is ROSC, and then restoring ventilation, reducing complication, so as to realize the ultimate goal of the hospital survival. Due to complex etiology, medical conditions, rescue time and other restrictions, resulting in different hospitals CA rescue level is uneven [16]. Therefore, finding a rapid, accurate and effective method of resuscitation is a challenge for medical workers. Investigators have suggested that there is a close correlation between PetCO2 and cardiac output, stroke volume, and coronary and cerebral perfusion pressure during CPR. Kalenda [17] first reported a decrease in PetCO2 in patients who could not be resuscitated, and a significant rise in PetCO2 in those patients in whom ROSC could be achieved. Falk and coworkers [18] found that PetCO2 decreased from mean of 1.4% before arrest to 0.4% after the onset of cardiac arrest. It then increased with CPR and ROSC. Sanders and colleagues [19] found that PetCO2 level predicted successful resuscitation after in hospital and out of hospital cardiac arrest. In our study we found that PetCO2 was gradually rising in success group during ALP-CPR process and increased slightly at 2~5min after ALP-CPR, then progressively decreased in failure group (P<0.05). PetCO2 values of 2.67kPa (20mmHg) or less discriminated between the 37 patients with ROSC and 55 patients without (P<0.05), and when a 20minute PetCO2value of 2.67kPa (20mmHg) or less was used as a screening test to predic ROSC, the sensitivity, specificity were all high. We also found that PetCO2 values under 1.9 kPa (14.3mmHg) after 20 minutes of >ALP-CPR are incompatible with ROSC. This is time of the end of haemo dynamic phase of ALP-CPR. These values may represented irreversible hemodynamic collapse, with inadequate coronary or myocardial perfusion pressure, or may represent perfusion pressures supplied too late (after the haemo dynamic phase), with consequent irreversible tissue damage [20,21]. Our study data, combined with the findings of other investigators, provide strong support for a resuscitation thresholds 2.67 kPa (20 mmHg) after 20 minutes of ALP-CPR. Values at 20 minutes reflect the patient's' response' to resuscitation efforts. We recommend 20-minute (final PetCO2) to be ranked in Utstein-style reports. The results of the study confirm that PetCO2 can play a pivotal role in the multi factorial decision-making process of whether to discontinue resuscitative efforts. Application of our findings could improve clinical prediction rules in the field and reduce the number of patients with cardiac arrest who undergo prolonged, futile resuscitation efforts; furthermore, there is less cost involved in the transfer of the patient to the hospital.
Conclusion
PetCO2 levels should be monitored during ALP-CPR and could be regarded as having prognostic value for determining the outcome of resuscitative efforts. PetCO2 levels should be monitored during CPR and considered as a useful prognostic value for determining the outcome of resuscitative efforts and when to cease CPR in the field. Based on our study findings, we believe that PetCO2 monitoring should be included in advanced cardiac life support and ranked in Utstein-style reports to provide insight into the condition of patients suffering cardiac arrest.
Acknowledgements
This study was supported by the All-Military Medical Technology 12th Five-Year Plan optional topic project (BWS11J077); national utility model patent (ZL.200920160376, ZL.200920164343.6); Henan Province medical technology breakthrough project (201303221); Zhengzhou technological leadership personnel focal project (131PLJRC682).
Appendix
Preliminary swine study using the abdominal lifting/ compression device
In the preliminary study ofthe abdominal/lifting compression device, 30 pigs were randomly divided into 2 groups with 15 pigs in each group. A coronary arrest model was produced by asphyxia as a result of clamping the trachea, and abdominal lifting and compression cardiopulmonary resuscitation (ALP- CPR) was performed in one group and standard CPR in the other group. Electrocardiogram (ECG), pulse oxygen saturation (SpO2), arterial partial pressure of oxygen (PaO2), end-tidal partial pressure of carbon dioxide (PE1CO2), aorta systolic blood pressure (SBP), diastolic blood pressure (DBP), central venous pressure (CVP), and tidal volume (VT) were monitored continuously from 10 minutes before asphyxia to the end of the experiment. The aorta mean arterial pressure (MAP), coronary perfusion pressure (CPP), and minute ventilation (MV) were calculated from the aforementioned data. Arterial blood samples were collected for blood gas analysis at 10 minutes before asphyxia, 10 minutes after asphyxia, and at 5, 10, and 20 minutes after resuscitation. Restoration of spontaneous circulation (ROSC) rate, 24-hour survival rate, and 24-hour neurological function score were the outcome measures. There were no significant differences in all mentioned indexes between the 2 groups at 10 minutes before and 10 minutes after asphyxia. At 2 minutes after the resuscitation, the MAP and CPP in the standard CPR group were significantly higher than those in the ALC-CPR group (MAP: 43.60±12.91 vs. 33.40±6.59 mmHg, respectively, P <0.05; CPP: 21.67±11.28 vs. 11.80±4.16mmHg, respectively, P< 0.01). The VT and MV in the ALC-CPR group were significantly higher than in the standard CPR group (VT: 111.6 ±18.12 vs. 56.60±7.76 ml, respectively; MV: 11.17 ± 1.81 vs. 5.54 ± 0.79L/min, respectively, both, P < 0.01). At 20 minutes after resuscitation, pH, PaO2 in ALC-CPR group were significantly higher than in the standard CPR group (pH: 7.16±0.16 vs. 7.01±0.14; PaO2: 82.73±13.20 vs. 58.33±17.77mmHg; respectively), HCO3- and base excess (BE) were significantly lower (HCO3-: 27.71±3.11 vs. 21.044±3.62mmol/L; BE: -4.78±4.30 vs. -10.23±2.12mmol/L, respectively) (all, P< 0.05). PaCO2, K+, and lactic acid were significantly lower in the ALP-CPR group than in the standard CPR group (PaCO2: 49.40±15.60 vs. 79.80±15.35mmHg; K+: 7.18±1.76 vs. 8.55±1.02mmol/L; lactic acid: 8.17±1.46 vs. 10.39±1.92mmol/L, respectively) (all, P< 0.05). The ROSC rate and 24-hour survival rate in ALC-CPR group were significantly higher than on the standard CPR group (ROSC rate: 80.0 vs. 26.7%, P < 0.01; 24 hour survival rate: 60.0 vs. 13.3%, respectively, P < 0.05). The 24-hour neurological function score was significantly lower in the ALP-CPR group than in the standard CPR group (1.11 ± 0.33 vs. 3.50±0.70, respectively, P < 0.01). These data lead us to conclude that ALP-CPR was at least as effective as standard CPR and that a clinical study was warranted.
The previous study about standard vs. abdominal lifting and compression CPR
The ALP-CPR group (n=40) compared with STD-CPR group (n=43), found that the two groups had similar baseline characteristics. After CPR, 9(22.5%) and 7(16.3%) patients in the ALP-CPR and STD-CPR groups, respectively, obtained ROSC (P=0.581). At 30 minutes, 7(17.5%) and 4(9.3%) patients, respectively, in ALP-CPR and STD-CPR groups survived (P=0.340). At 60 minutes after ROSC, 7(17.5%) and 2(4.7%) patients, respectively, in the ALP-CPR and STD-CPR groups survived (P=0.081). The ALP-CPR group had a significantly higher heart rate and lower mean arterial pressure (MAP) then the STD-CPR group (heart rate: 106.8 vs. 79.0, P< 0.001; MAP: 60.0 vs. 67.3 mm Hg, P=0.003). The post-treatment PCO2 was significantly lower in the ALP-CPR than in STD-CPR group (52.33 vs. 58.81, P=0.009). PO2 was significantly increased after ALP-CPR (45.15 to 60.68, P< 0.001), but was not changed after STD-CPR. PO2 after CPR was significantly higher in the ALP-CPR group (60.68 vs. 44.47, P< 0.001).These data lead us to conclude that abdominal lifting and compression cardiopulmonary resuscitation device is as effective as STD-CPR with respect to ROSC.
References
- Link MS, Berkow LC, Kudenchuk PJ, Halperin HR, Hess EP, et al. (2015) Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 132(18 Suppl 2): S444-S464.
- Fernandez LI, Urki'a C, Lopez Mesa JB, Juan Manuel Escudier, Ignacio Manrique, et al. (2016) European Resuscitation Council Guidelines for Resuscitation 2015: Key Points.. Revista Espanola De Cardiologi'a 69: 588-594.
- Grmec S, Krizmaric M, Mally S, Kozelj A, Spindler M, et al. (2007) Utstein style analysis of out-of-hospital cardiac arrest-bystander CPR and end expired carbon dioxide. Resuscitation 72(3): 404-414.
- Rudner R, Jalowiecki P, Karpel E, Dziurdzik P, Alberski B, et al. (2004) Survival after out-of-hospital cardiac arrests in Katowice (Poland): outcome report according to the "Utstein style”. Resuscitation 61(3): 315-325.
- Zhang S, Liu Q, Han S, Ziran Zhang, Yan Zhang, et al. (2016) Standard versus Abdominal Lifting and Compression CPR. Evidence-Based Complementray and Alternative Medicine 2016(2016): 1-8.
- Ahrens T, Schallom L, Bettorf K, Ellner S, Hurt G, et al. (2001) End-tidal carbon dioxide measurements as a prognostic indicator of outcome in cardiac arrest. Am J Crit Care 10(6): 391-398.
- Marwick TH1, Case CC, Siskind V, Woodhouse SP (1991) Prediction of survival from resuscitation: a prognostic index derived from multivariate logistic model analysis. Resuscitation 22(2): 129-137.
- Morrison LJ, Visentin LM, Kiss A, Theriault R, Eby D, et al. (2006) Validation of a rule for termination of resuscitation in out-of-hospital cardiac arrest N Engl J Med 355(5): 478-487.
- Orliaguet GA, Carli PA, Janniere D, Janniere D, Sauval P, et al. (1995) End-tidal carbon dioxide during out-of-hospital cardiac arrest resuscitation: comparison of active compression-decompression and standard CPR. Resuscitation 25(1): 48-51.
- Kolar M, Krizmaric M, Klemen P, Stefek Grmec (2008) Partial pressure of end- tidal carbon dioxide successful predicts cardiopulmonary resuscitation in the field: a prospective observational study. Crit Care 12: R115.
- Morino A, Shida M, Tanaka M, Kimihiro Sato, Toshiaki Seko, et al. (2015) Journal of Physical Therapy Science 27(7): 2167-2169.
- Babbs CF (2003) Interposed abdominal compression CPR: a comprehensive evidence based review. Resuscitation 59(1): 71-82.
- Kim DH, Dong YR, Woo SH, Lee WJ, Seol SH, et al. (2015) Acute Mallory- Weiss syndrome after cardiopulmonary resuscitation by health care providers in the emergency department. Journal of Acute Disease 4(4): 326-328.
- Field JM, Hazinski MF, Sayre MR, Chameides L, Schexnayder SM, et al. (2010) Part 1: executive summary: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 122(18 Suppl 3): S640-656.
- Wang GT, Zhang SS, Liu qing (2015) Clinical application of abdominal pressure cardiopulmonary resuscitation: a report of 40 cases. Chin J Emerg Med 24: 1264-1267.
- Kayser RG, Ornato JP, Peberdy MA (2008) Cardiac arrest in the Emergency Department:a report from the National Registry of Cardiopulmonar. Resuscitation 78(2): 151-160.
- Kalenda Z (1978) The capnogram as a guide to the efficacy of cardiac massage. Resuscitation 6(4): 259-263.
- Falk JL, Rackow EC, Weil MH (1988) End-tidal carbon dioxide concentration during cardiopulmonary resuscitation. N Engl J Med 319(10): 607-611.
- Sanders AB, Kern KB, Otto CW, Milander MM, Ewy GA (1989) End-tidal carbon dioxide during cardiopulmonary resuscitation: a prognostic indicator for survival. JAMA 262(10): 1347-1351.
- Ewy GA (2005) Cardiocerebral resuscitation: the new cardiopulmonary resuscitation. Circulation 111(6): 2134-2142.
- Ewy GA (2006) Cardiac resuscitation: when is enough enough? N Engl J Med 355(5): 510-512.






























