Abstract
Keywords:Echocardiography; Anesthesiology; Morbidity; Mortality; Hemodynamic Instability; Cardiovascular
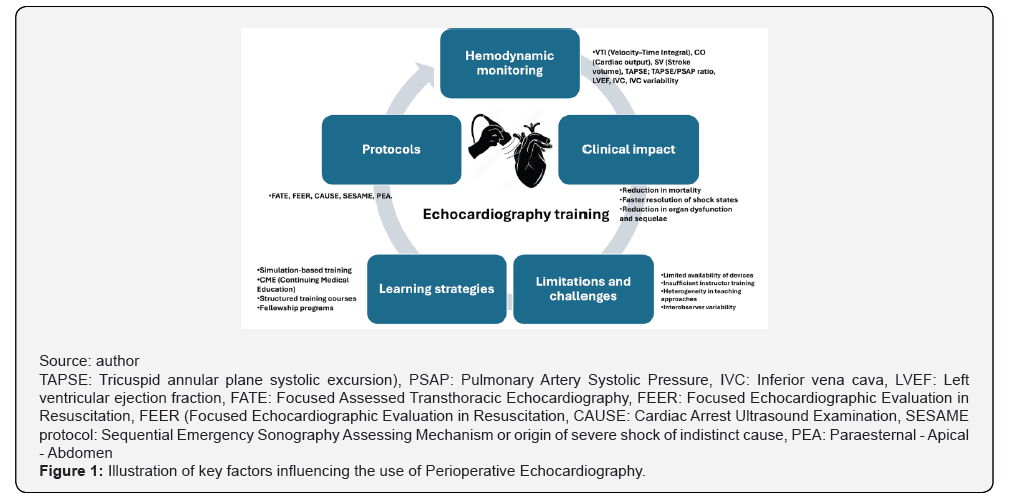
Abbreviations:TAPSE: Tricuspid Annular Plane Systolic Excursion; PSAP: Pulmonary Artery Systolic Pressure; IVC: Inferior Vena Cava; LVEF: Left Ventricular Ejection Fraction; FATE: Focused Assessed Transthoracic Echocardiography; FEER: Focused Echocardiographic Evaluation in Resuscitation; FEER Focused Echocardiographic Evaluation in Resuscitation; CAUSE: Cardiac Arrest Ultrasound Examination; SESAME protocol: Sequential Emergency Sonography Assessing Mechanism; PEA: Paraesternal Apical Abdomen
Introduction
Advances in medicine over recent decades have been remarkable, and the practice of anesthesiology has been no exception. These developments have enabled the optimization of perioperative strategies aimed at reducing morbidity and mortality, among which perioperative echocardiography occupies a prominent role. This tool has become consolidated as a fundamental resource for the modern anesthesiologist, facilitating rapid, dynamic, bedside cardiovascular assessment in scenarios characterized by hemodynamic instability. Its utility extends particularly to perioperative rescue management and guidance of interventions in situations of high risk of circulatory collapse [1]. Nevertheless, despite its increasing use and potential to improve clinical outcomes, a significant educational gap persists. The teaching of perioperative echocardiography remains heterogeneous, poorly standardized, and in many cases neither evaluable nor sustained over time. This situation has prompted explicit reflections on how perioperative echocardiography should be taught and which training standards should be adopted within anesthesiology programs, with the aim of strengthening structured educational models that allow effective training and positively impact patient care [2], even exploring online training modalities as a viable alternative in certain contexts [3] (Figure 1).
The application of practical protocols aimed at answering specific clinical questions has proven particularly useful in improving intraoperative hemodynamic management. Among these, the Focus approach proposes a protocolized evaluation based on basic echocardiographic windows-typically subcostal and apical four-chamber views, as well as parasternal long- and short-axis views-with the purpose of identifying diagnostic targets such as qualitative left ventricular systolic function, right ventricular size and function, the presence of pericardial effusion or tamponade, and an approximation of volume status and preload, including assessment of the inferior vena cava within its clinical context. These are complemented by more advanced but relatively simple-to-measure parameters, such as TAPSE, the TAPSE/PSAP ratio, VTI measurement for cardiac output estimation, and basic lung ultrasound [4]. Integration of these findings with clinical data allows structured hemodynamic reasoning and decision-making that is crucial for the resolution of critical situations in real time. In this context, perioperative echocardiography should no longer be conceived as an optional skill or one reserved exclusively for subspecialists, but rather consolidated as an essential competency in anesthesiology residency training, comparable to the use of the stethoscope in medical practice. This position is supported by evidence of its clinical utility, its ability to modify therapeutic decisions, and its integration into structured protocols such as Focus and cardiac POCUS.
Impact on Resident Training
The early and structured incorporation of basic, reproducible, and supervised training in perioperative echocardiography promotes systematic use of this tool throughout residency. This process contributes to the development of pathophysiological reasoning, enables an integrated understanding of preload, afterload, and contractility, and improves the ability to respond to scenarios of hemodynamic instability, based on parameters obtained through Focus/cardiac POCUS protocols (Figure 1).
Challenges and Limitations
The implementation of perioperative-focused echocardiography programs or protocols faces relevant challenges, including equipment availability, the training of qualified instructors, and heterogeneity in educational models across institutions, all of which hinder routine application. Additionally, the operator-dependent nature of the technique requires adequate supervision and competency-based evaluation to minimize erroneous interpretations. However, these limitations can be addressed through strategies such as continuous instructor training, use of simulation, protocol standardization, and clear definition of educational objectives, thereby enabling safe and sustainable integration of perioperative echocardiography into anesthesiology residency programs.
Conclusion
Perioperative Echocardiography has demonstrated a significant improvement in hemodynamic assessment and real-time decisionmaking, particularly when applied through structured protocols such as Focus and cardiac POCUS. However, its teaching during anesthesiology residency remains heterogeneous and, in many settings, insufficient, despite evidence supporting its clinical and educational value. Integrating perioperative echocardiography as a fundamental and formal competency within residency programs represents a key opportunity to strengthen pathophysiological and hemodynamic reasoning, as well as to improve patient safety. More than an advanced skill, it should be understood as an extension of the clinical examination and perioperative monitoring, whose early and supervised learning may translate into better clinical decisions and more favorable outcomes.
References
- Cowie B (2012) Focused transthoracic echocardiography predicts perioperative cardiovascular morbidity. J Cardiothorac Vasc Anesth 26(6): 989-993.
- Hernandez D, Feinman J (2022) An Unsentimental Education: How Should We Be Teaching Perioperative Echocardiography? J Cardiothorac Vasc Anesth 36(1): 163-165.
- Cabrera Schulmeyer MC, Aranda F, Sanhueza E, Melis N (2024) Educación on-line en anestesiología: Ecocardiografía perioperatoria para América Latina. Rev Chil Anest 53(6): 655-659.
- Spencer KT, Kimura BJ, Korcarz CE, Pellikka PA, Rahko PS, et al. (2013) Focused cardiac ultrasound: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr 26(6): 567-581.






























