Summary
Objective: To determine the epidemiological profile and progression of patients admitted for obstetric complications to a multi-purpose intensive care unit in a rural African setting.
Patients and Methods: The records of patients hospitalized in intensive care for obstetric complications at the Thierno Birahim Ndao Regional
Hospital in Kaffrine from 1 January 2022 to 31 December 2024 were analyzed. The parameters studied were epidemiology, main reasons for
admission, treatment and patient outcomes.
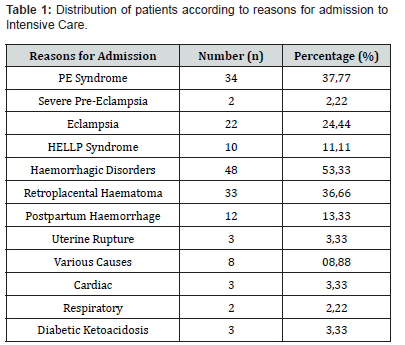
Results: During the study, 90 women were admitted to the multi-purpose intensive care unit (35% of all hospitalizations). The most common
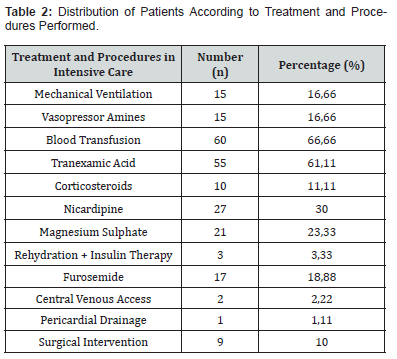
causes of admission were obstetric haemorrhages (53.33%) and hypertensive disorders of pregnancy (37.77%). The main therapeutic
interventions were blood transfusion (66.66%), antihypertensive treatment with nicardipine (30%) and magnesium sulphate (23.33%), and
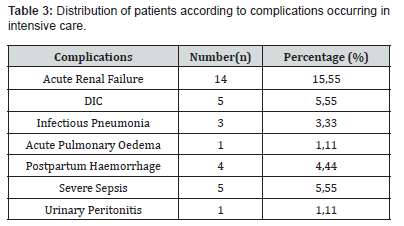
vasopressor amines (16.66%). Twenty-four patients (26.66%) experienced complications during hospitalisation. We observed seven maternal
deaths (7.77%).
Conclusion: The most common obstetric conditions encountered in intensive care in rural areas are obstetric haemorrhage and hypertensive
disorders of pregnancy. Better management of these complications would reduce maternal morbidity and mortality.
Keywords:Obstetric Complications; Intensive Care; Morbidity; Mortality
Abbreviations:HBP: High Blood Pressure; APE: Acute Pulmonary Oedema; ARF: Acute Renal Failure; MLS: Mean Length of Stay; DIC: Disseminated Intravascular Coagulation; PE: Pre-Eclampsia
Introduction
Obstetric complications are common causes of admission to intensive care units in developing countries, especially in rural areas. They vary between 5 and 20% in some African studies [1], whereas in developed countries they account for less than 1% of hospitalisations [2]. These complications, which are dominated by hypertensive disorders and obstetric haemorrhages, are most often caused by the existence of contributing factors or chronic disease. They are often neither predictable nor preventable by gynaecological and obstetric monitoring during pregnancy. They can be life-threatening for both mother and fetus in the absence of appropriate management procedures. The main objective of this study was to determine the epidemiological profile and outcome of patients admitted to intensive care during pregnancy or postpartum.
Patients and Methods
We conducted a retrospective observational study over a 12-month period (January 2022 to December 2022) in the general intensive care unit at the Thierno Birahim NDAO Regional Hospital Centre (CHRTBN) in Kaffrine. It focused on analysing the records of women admitted to intensive care during pregnancy or postpartum (42 days after delivery). The parameters studied were epidemiological data, main reasons for admission, anaesthetic technique, complications occurring in intensive care, main treatments administered and patient progress. All the data recorded were entered into Excel (MicrosoftTM) and analysed using SPSS (Statistical Package for Social Sciences) version 1. We used the chi-square test to analyses the qualitative data. A p-value of less than 0.05 was considered significant.
Results
During this period, 90 patients were admitted to intensive care for obstetric complications, representing 35% of hospitalisations. The average age was 24 (range 15-40). In our series, there was a clear predominance of multiparous women (65%). The main medical histories found were asthma (1 case), high blood pressure (HBP) (2 patients), cardiomyopathy (3 cases) and diabetes (3 cases). The main maternal complications leading to admission to intensive care are shown in (Table 1). The most common was obstetric haemorrhage (48 cases), including 33 cases of HRP, 12 cases of HPP and 3 cases of uterine rupture. The second most common cause of admission was pre-eclampsia syndrome, with 34 cases (37.77%). Other reasons included cardiac problems (3 cases), renal problems (2 cases) and diabetic ketoacidosis (3 cases). (Table 1) shows the distribution of patients according to the reasons for hospitalisation. The majority of patients were admitted in the postpartum period (91%) and 14 patients (15.55% of cases) had given birth vaginally. General anesthesia was the most commonly used anaesthetic technique (89% of cases). In terms of intensive care treatment, 15 patients (16.16%) received respiratory support with orotracheal intubation and antihypertensive treatment based on nicardipine was initiated in 27 patients (30% of cases). Blood transfusions and tranexamic acid were used in 66.66% and 61.11% of cases, respectively. Fifteen patients (16.16%) received vasopressor amines and three underwent haemodialysis. (Table 2) shows the distribution of patients according to the treatment administered in intensive care. Twenty-four patients (26.66%) experienced complications during their stay in intensive care. The most common complications were acute renal failure (14 cases), infectious pneumonia (4 cases), disseminated intravascular coagulation (5 cases) and severe sepsis (5 cases). (Table 3) shows the distribution of patients according to complications. The average length of stay in intensive care (ALOS) was 3.63 ± 1.82 days (range 1-13 days). The outcome was favorable in 83 cases; 07 patients died, representing a mortality rate of 7.77%. The causes of maternal death recorded were DIC (04 cases), severe sepsis (02 cases) and APE (acute pulmonary oedema) on ARF (acute renal failure) (01 case). There was a significant relationship between mortality and mechanical ventilation in intensive care, with a p value = 0.000. Mortality was closely linked to the occurrence of ARF (p = 0.047) and DIC (p = 0.000). The analytical study of mortality in our series identified several factors associated with poor prognosis. These were mainly the presence of DIC, ARF and the use of mechanical ventilation in patients.
PE: Pre-Eclampsia
ARF: Acute Renal Failure; DIC: Disseminated Intravascular Coagulation; APE: Acute Pulmonary Oedema
Discussion
Over the period, 90 patients were hospitalized for obstetric complications, with the incidence of these conditions in intensive care, among all admissions to the department, being 35%. Fall in Senegal found a lower frequency of 18.5% [3]. The prevalence of obstetric conditions in intensive care is higher in African studies: Cameroon 6.1% [1] and Benin 34% [4]. In contrast, in developed countries, it is less than 1% [2]. The hospitalisation of women in intensive care in an obstetric context may depend not only on the severity of the clinical picture, but also on the availability of care. It is lower in regions where maternity wards are associated with intensive care units. It is in countries that are most lacking in intensive care facilities that the needs are greatest. These obstetric emergencies constitute a health problem and reflect the level of development of the health system in these countries. The average age of patients was 24, and the majority of patients (47%) were between 20 and 30 years old, was found in most African series with an average age between 21 and 26 years old [1,4].In our series, the main reasons for admission to intensive care were identical to those found in developing countries: haemorrhagic disorders (53.33%), including 33 cases of HRP, 12 cases of HPP and 3 cases of uterine rupture, followed by hypertensive disorders (37.77%). Tchaou in Benin found 21.7% of haemorrhagic disorders and 16.4% of hypertensive disorders [4]. In our study, 65 patients (66%) received blood transfusions and tranexamic acid was administered in 61.11% of cases. Bah in Senegal and Keiz et al. reported transfusion rates of 37.9% and 66.2% respectively [5,6]. Fifteen per cent of patients in the study by Mahutte et al. [7] received vasoactive amines, primarily for haemorrhagic shock, and 21.4% in the series by Bah [6]. In our study, 16.66% of patients received vasopressor amines. The main indication for amines in our study was haemorrhagic shock.
Antihypertensive treatment with intravenous nicardipine was used in 30% of cases. In Bah’s series [6], it was administered in 35% of cases. Nicardipine, which is a calcium channel blocker, remains the most widely used molecule in our study, as it helps prevent maternal complications of high blood pressure (stroke, eclampsia, pulmonary oedema) [8]. Three per cent (3%) of patients underwent dialysis in Bah’s study [6] and in our study, three patients (3.3%) underwent dialysis despite the 14 cases of ARF reported. In fact, the therapeutic management of ARF consisted primarily of well-conducted vascular filling to optimize blood volume and the administration of diuretics in cases of persistent oligoanuria. Diuretics play an important role in the management of ARF [9]. In our series, 18.88% of patients received intravenous furosemide. With regard to surgical interventions after admission to intensive care, the study by Keizer et al. [5] (7%) found that in our study, 9 patients (10%) underwent emergency surgery after admission, five (5.15%) of whom underwent hysterectomy and one patient underwent JJ stent placement following accidental sectioning of both ureters. Obstetric pathology can lead to serious complications that may be life-threatening. In our study, we found 24 cases (26.66%) of complications occurring during hospitalisation. These were mainly ARF (14 cases), DIC (5 cases), sepsis (5 cases) and postpartum haemorrhage (4 cases). These complications were often related to the low level of healthcare and the severity of the patients’ clinical condition. In our study, the mean length of stay (MLS) was 3.63 ± 1.82 days (range 1-13 days). Some series in the literature report an MLS in intensive care ranging from 3.2 days [3] to 5.7 days [10]. The patients were admitted to a multi-purpose intensive care unit, rather than to continuous monitoring units where parturient have much less severe parameters than in intensive care units. In our study, the maternal mortality rate was 7.77% (07 cases), with the leading cause of death being DIC (05 cases), most often complicating massive haemorrhages. Seventeen patients (9.6%) died in the study by Owono Etoundi in Cameroon [1]. Fall in Senegal noted a mortality rate of 5.8% in his study, including 2 cases of DIC and 2 cases of septic shock [3]. In the study by Gilbert et al. eight women died during their stay, including two from postpartum haemorrhage and one patient from respiratory failure [1]. Fall in Senegal noted a mortality rate of 5.8% in his study, including two cases of DIC and two cases of septic shock [3]. In the study by Gilbert et al. eight women died during their hospital stay, including two from postpartum haemorrhage and one from respiratory failure [11]. The factors identified in our study as contributing to death were renal failure (p=0.047), DIC (p=0.000), and the use of mechanical ventilation (p=0.000).
Conclusion
The frequency of admission to intensive care for obstetric conditions varies greatly from one region to another and is higher in developing countries. The main reasons for admission are haemorrhage and hypertensive disorders. These results suggest that the availability of local healthcare influences the management strategy for women with severe obstetric complications. Regular study of maternal morbidity and mortality is important for improving professional practices.
References
- Owono-Etoundi P, Junette M, Tchokam L, Celestin D, LK, et al. (2017) Complications obstétricales admises en réanimation: épidémiologie, diagnostic et pronostic. Health Sci Dis 18: 48-
- Bonnet MP, Chantry A, Seco A, Chiesa-Dubruille C, Fresson J, et al. (2015) Admissions obstétricales en réanimation: des leçons à tirer pour l’organisation des soins? Anesth Réanimation 1: A119.
- Fall ML, Diop EN, Barboza D, Diop MN, Diédhiou M, et al. (2020) Prise en charge des urgences obstétricales dans une réanimation périphérique en Afrique subsaharienne exemple du CHR de Ziguinchor. RAMUR 25(2): 33-38.
- Tchaou BA, Hounkponou NFM, Salifou K, Zoumenou E, Chobli M, et al. (2015) Les urgences obstétricales à l’hôpital universitaire de parakou au bénin: aspects cliniques, thérapeutiques et é European Scientific Journal 11(9): 260-272.
- Keizer JL, Zwart JJ, Meerman RH, Harinck BIJ, Feuth HDM, et al. (2006) Obstetric intensive care admissions: a 12-year review in a tertiary care centre. Eur J Obstet Gynecol Reprod Biol 128(1-2): 152-15
- Bah MD, Sow D, Gaye I, Diaw M, Traoré MM, et al. (2023) Le’s complications obstétricales en réanimation: profil clinique et aspcets thé Ann Mar Méd Urg & Réa 13: 15-20.
- Mahutte NG, Murphy-Kaulbeck L, Le Q, Solomon J, Benjamin A, et al. (1999) Obstetric admissions to the intensive care unit. Obstet Gynecol 94(2): 263-26
- Mpika GB, Itoua C, Ngbale RN, Goddot M (2014) Place de la nicardipine dans la prise en charge de la pré-eclampsie. Med Afri Noire 61(3): 133-139.
- Bonnet MP, Garnier M, Keita H, Compère V, Arthuis C, et al. (2021) Guidelines for the management of women with severe pre-eclampsia. Anaesth Crit Care Pain Med 40: 100901.
- Lelong E, Pourrat O, Pinsard M, Goudet V, Badin J, et al. (2013) Admissions en réanimation des femmes en cours de grossesse ou en post-partum: circonstances et pronostic. Une série rétrospective de 96 cas. La Revue de Médecine Interne 34(3): 141-147.
- Gilbert TT, Smulian JC, Martin AA, Ananth CV, Scorza W, et al. (2003) Obstetric admissions to the intensive care unit: outcomes and severity of illness. Obstet Gynecol 102(5 Pt 1): 897-903.






























