Summary
Introduction: Placental abruption is defined as the premature detachment of a normally inserted placenta. It is a hemorrhagic complication that may engage the maternal-fetal prognosis. Its management is multidisciplinary but remains delicate both obstetrically and anesthetically.
Methodology: We conducted a retrospective and descriptive study over an 18-month period from January, 2023 to July, 2024. The data included epidemiological variables and anesthetic elements in perioperative.
Results: We collected 39 cases of placental abruption. The prevalence of placental abruption was 3.1%. The average age of patients was 27.9 years. The gestational age was on average 34.2 WG (weeks of gestation). A maternal rescue was indicated in 55.2% of cases. Paucigests and pauciparous women were the most represented with 36.7% and 43% respectively. Clinical anemia was noted in 33.3% of cases with a mean hemoglobin level of 9.26 g/dL and extremes of 4.5 and 12.9 g/dL. General anesthesia with rapid sequence intubation was the most used anesthetic technique in 73.3%. Ketamine was the most commonly used hypnotic. Blood transfusion was done in 25.64% of patients with whole blood. A hysterectomy of hemostasis was performed in 10.26% of the patients. No deaths on the operating table were noted.
Conclusion: This study highlights the need to make available anesthetic products in sufficient quantities for efficient perioperative management of patients in a state of shock, to equip blood banks with equipment and maternity wards with diagnostic assistance devices.
Keywords:Placental Abruption; Hemorrhagic Shock; Anesthesia; Ziguinchor
Abbreviations:SDGs: Sustainable Development Goals; WG: Weeks of Gestation; SBP: Systolic Blood Pressure; DIC: Disseminated Intravascular Coagulation; FFP: Fresh Frozen Plasma; RCB: Red Blood Cells
Introduction
Obstetric emergencies include all pathologies of sudden onset that can be life-threatening or functional in a pregnant woman and directly related to pregnancy or childbirth. Their care is multidisciplinary involving: obstetricians, neonatologists, anesthesiologist-resuscitators and emergency physicians. The placental abruption is one of these emergencies. It is a paroxysmal accident of renal vascular syndromes that consists of a premature detachment of the placenta normally inserted while the fetus is still uterus [1]. In 2020, nearly 800 women died per day from preventable causes related to pregnancy and childbirth. Nearly 95% of maternal deaths occurred in low- and middle-income countries. Reducing maternal mortality is therefore a priority objective in reproductive health, especially in developing countries [2]. In Senegal, policies and strategies have been developed to improve the health of the most vulnerable populations, particularly women, newborns and children. Maternal and child health still remains a challenge, even if significant progress has been made in view of the Sustainable Development Goals (SDGs).
The maternal mortality ratio increased from 392 to 153 per 100 000 live births between 2010-2011 and 2023. Despite progress in the fight against maternal mortality, progress is still not sufficient. The reduction of maternal mortality is thus still part of the Sustainable Development Goals (SDGs) for the period 2015-2030 [3]. Women die as a result of complications during and after pregnancy and childbirth. Most of these complications occur during pregnancy and can, in most cases, be prevented or treated. Other complications sometimes appear before pregnancy but are aggravated during pregnancy, especially if they are not managed. The main complications, responsible for nearly 75% of maternal deaths are severe hemorrhages including placental abruption, infections, high blood pressure during pregnancy (preeclampsia and eclampsia), and complications from childbirth and unsafe abortions [2,4]. Anesthetic management when a cesarean is indicated for a placental abruption remains a challenge for the anaesthesiologist resuscitator. It is with this in mind that we conducted this work to evaluate anesthetic practices before a placental abruption at the Peace Hospital in Ziguinchor. The specific objectives were to specify the epidemiological profile and to evaluate anaesthetic management pre, per and post-operative.
Patients and Methodology
This is a retrospective and descriptive study. It took place over a period of 18 months from January 1st, 2023 to June 30th, 2024. The study population is represented by patients who underwent an urgent cesarean during the period of the study. Were included in our study, the patients undergoing caesarean section in emergency surgery whose diagnosis of placental abruption was made preoperatively or suspected and confirmed post-operatively. The parameters studied were:
a) Epidemiological data: number of patients, age of the
patients, gestational age,
b) The background and the medical history
c) Preoperative data: clinical and biological
d) The type of anesthesia and the anesthetic products used
e) The occurrence of incidents during surgery
f) The notion of intraoperative blood transfusion
g) The use of tranexamic acid
h) Antibioprophylaxis
i) The use of oxytocin
j) The surgical procedures performed
k) Post-operative management
Results
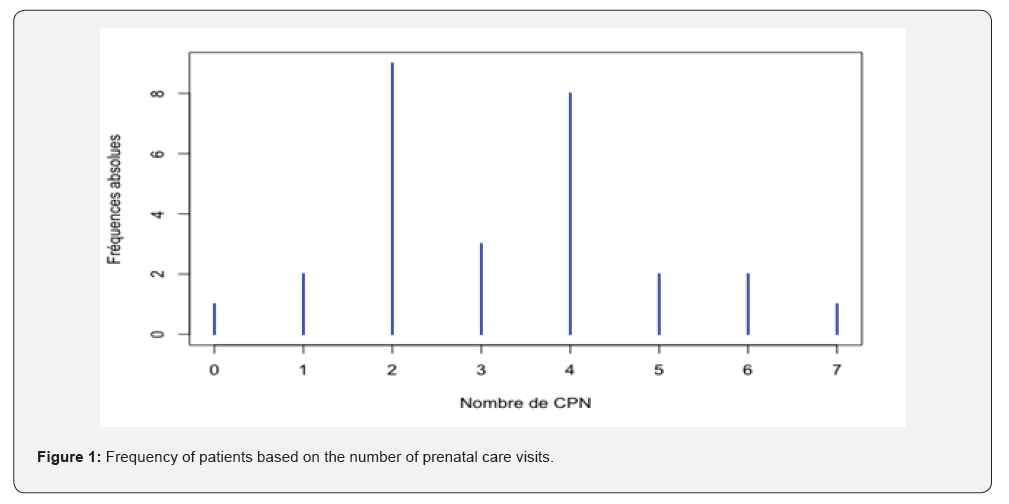
During the study period, 39 cases of placental abruption were diagnosed out of 1 258 births, a frequency of 3.1%. Among the 39 cases, 30 patients were admitted to the operating room for an emergency caesarean section, representing 76.9% of placental abruption cases. The average age of the patients was 27.9 years with extremes of 20 and 39 years. The most represented age group was between 25 and 30 years with a proportion of 58.6%. The gestational age was on average 34.2 weeks of gestation (WG) with extremes of 26 and 42 WG. The indication for a cesarean section was specified in 29 patients. More than half of the indications, 55.2%, were for a maternal rescue. The history of a cesarean section was found in 6.7% of patients. The proportion of primigests was 17% and that of paucigests was 36.7%. More than a quarter of the patients, 26%, were multiparous and 19.6% were large multiparous. Nulliparous accounted for 17% and primiparous 10%. Nearly half, or 43%, were pauciparous followed by multiparous in 20% and large multiparous in 10%. A stillborn child was found in 12% of the patients. Nearly half, or 43.3%, had completed at least 4 prenatal care visits. The (Figure 1) below represents the distribution of patients according to the number of prenatal care visits.
More than a quarter, or 25.64%, of the patients presented with clinical anemia upon examination of the conjunctival mucous membranes. The average shock index was 0.83. One-third of the patients had a shock index greater than or equal to 0.90. The mean haemoglobin level was 9.26 g/dL with extremes ranging from 4.5 to 12.9 g/dL. Eight patients had thrombopenia, half of which had a rate below 100,000/mm3. The delay between admission to the maternity ward and placement in the operating room was specified for 51.28% of patients. The latter ranged from 10 to 60 minutes with an average of 33.6 ± 12.4 minutes. The median was 30 minutes. Half of the patients were taken care of between 25 and 40 minutes after their arrival. Almost half of the patients, or 45.9%, were taken care of within 30 to 45 minutes after their arrival. Almost a third, or 29.7%, was handled between 15 and 30 minutes. General anesthesia was the anesthetic technique performed in 73.3% and spinal anesthesia in 26.7%. The induction of all patients was done in rapid sequence with the hypnotic and suxamethonium combination. Induction was done with the ketamine-midazolam combination in 32% of cases. Ketaminepropofol was used in 28% of cases.
Propofol alone was used in 24% of cases, ketamine alone in 12% and the combination of ketamine and etomidate in 4% of cases. Isoflurane was used for hypnosis maintenance in 65% and sevoflurane in 35%. The products used for spinal anesthesia were 8 mg hyperbaric bupivacaine combined with 25mcg fentanyl. Perioperative incidents were noted in 39.6% of patients. Almost half of them had hypotension. A case of cardiorespiratory arrest was noted. Amines were used in 33.3% of patients. Ephedrine was used in 30% of patients, noradrenaline in 3.3% of patients and adrenaline in 3.3%. All our patients benefited from a vascular filling. Crystalloids were mainly used to stabilize the hemodynamic state with an average of 1300 ml. Colloids were used in 13.2% of patients with an average amount of 500 ml. Blood transfusion was performed in 33.3% of patients. Tranexamic acid was used in 73.3% of patients. Antibiotic prophylaxis with cefazolin 2g was done in all patients. Oxytocin was administered in 93.3% of patients. The gestures performed intraoperatively were fetal extraction alone in 86.7% of patients and in 13.3% the extraction was followed by a hysterectomy. We had 13 live births. The Apgar score and the notion of resuscitation were only specified in 7 files. The following (Table 1) shows the distribution of children based on the Apgar score at one minute and five minutes. No patient died on the operating table. After the surgery, half of the patients were transferred to the gynecologic-obstetric department and the other half was admitted to intensive care unit. The suites were simple for all the parturients.

Discussion
The limitations and difficulties encountered in our study concerned the non-performance of certain biological examinations due to a lack of reagents and the incomplete nature of the medical records, making it difficult to use them. However, beyond all these obstacles, we have collected 30 patients in accordance with the inclusion criteria of our series. During our study period, 39 cases of placental abruption were identified and the 30 or 76.9% underwent a cesarean section. The noted placental abruption cases represented 3.1% of births, which is close to the figures for Sene [5], which had a prevalence of 2.98%, and for Niass [6] and Diarra [7], which had 2.2% and 1.96% respectively. But these data are well above the figures for Aaboudech T [8] which was 0.56% in Morocco. However, the prevalence was lower than that found in a Kanta study [9] in Mali by 5.1%. Indeed, it is in fact very difficult to have an accurate assessment of the frequency of placental abruption because the definition varies according to the mode of diagnosis [10]. The average age of our patients was 27.9 years and the 25-29 age group was the most affected. This average age is close to that found in the series of Sene [5] and Thiam [10] which was 28.8 years and 29 years respectively. Indeed, in several series the incidence of placental abruption increases with maternal age [11].
The average gestational age of occurrence was 34.17 WG in our series, which is consistent with the figures from the literature. Indeed, placental abruption is a paroxysmal pathology of the third trimester of pregnancy [12,13]. The sounds of the fetal heart were not perceived in 55.2% of cases and the indication of a maternal rescue was raised. The indication rate for maternal rescue is lower in our study compared to the rates found in the Sene [5] studies of 60.97%, Guisse [14] of 64.9% and Diarra [7] in Mali of 67.4%. This in utero death rate could be explained by the fact that the diagnosis of placental abruption is delayed, but also by the transfer delays which can be long in the absence of an ambulance in certain areas. Pauciparous patients were most affected by the placental abruption with a frequency of 43%, followed by multiparous and large multiparous who accounted for 30% cumulatively. These results are contradictory with most of the results of studies conducted in Senegal. Indeed, in the studies of Thiam [10] and Sene [5], a higher frequency was noted in multiparous and large multiparous with 63.4% and 68% respectively. Placental abruption is an unpredictable pathology that can affect all women of childbearing age regardless of parity. Nearly one third, or 33.3%, of patients had clinical anemia. However, Diarra [7] found 75.4% of her patients who presented with clinical anemia. This can be explained by the delay in diagnosis but also in the management of placental abruption cases. We had found 46.7% of patients with hypertension with a systolic blood pressure (SBP) greater than or equal to 140 mmHg. This hypertension is also found in the work of Diarra [7] in 28.9% of patients and Diallo [13] in 68.5%.
This hypertension, although it is a cause of placental abruption, must be approached with caution because it is very often, a hypertension that ‘hides misery’ because patients most often arrive in a state of compensated shock. This is all the truer as 33.3% of patients had a shock index greater than or equal to 0.9, which suggests the existence of a compensated shock with need for transfusion. In our series, 53.3% of patients had a hemoglobin level below 10g/dL. More than a quarter, or 26.7%, had thrombocytopenia, half of which with a rate less than 100 000/ mm3. However, Kilani [12] found 72.22% of patients with anemia and 22.22% of patients who presented with thrombocytopenia. This anemia and thrombopenia are explained by the presence of the hematoma and its increase over time as well as the DIC (disseminated intravascular coagulation) that results from the process. The assessment of coagulation by measuring the TP was only available in 36.67% of the patients and only one, namely 9.1%, had a TP below 50%. This low rate of patients with a clotting procedure could be explained by the lack of reagents at the laboratory level but also by the slowness in delivering the results. General anesthesia with orotracheal intubation was the most used anesthetic technique in 73.3% of cases. Spinal anaesthesia was performed in the other patients (26.7%). In the series of Sene [5], the caesarean section was performed in 100% of cases under general anesthesia. On the other hand, in the study of Dia [15] only 15.8% of patients were caesarized under general anesthesia.
Spinal anaesthesia, although not totally contraindicated, presents a major anesthetic risk because it is an anaesthetic in a hypovolemic patient, probably in a state of shock and who presents a significant risk of coagulopathy. It is moreover this risk of coagulopathy that makes epidural anesthesia formally contraindicated [16]. For the induction of our patients, ketamine was the most used hypnotic alone or in combination for coinduction. Ketamine, inducing few hemodynamic changes is interesting when maternal hemodynamics is unstable. It decreases the incidence of maternal memorizations. Its adverse effects are the delusional manifestations with hallucinations upon waking [15]. It is to reduce these adverse effects that it was associated with midazolam in 32% of cases. Propofol, although it is the reference hypnotic in general anesthesia for a cesarean section, is not the best choice in a context of placental abruption with regard to hemodynamically precarious patients [17]. They often present a hypertension that should be cautioned, because it often hides hypovolemia or a state of shock in the compensation phase. However, propofol was the only hypnotic drug available, which means that it was used for induction in titration in 24% alone and in 28% of cases in combination with ketamine.
The interview was done with halogens in 95.2% of cases, including isoflurane in 65% and sevoflurane in 35%. Sevoflurane 1% was compared to isoflurane 0.5% in maintenance and found no significant difference between the two groups with regard to hemodynamic changes, blood loss, uterine tone and postoperative complications. At these doses, the halogens have almost no effect on hemodynamics [15,18]. Among the perioperative incidents, we noted 40% of cases of hemodynamic instability. A cardiorespiratory arrest, a patient’s fall from the top of the operating table and an episode of convulsions were noted in 3.33% each. Sene [5] noted in its series a hemodynamic instability in 100% of the patients undergoing intraoperative surgery. The instabilities were jugulated by a vascular filling with crystalloids (average 1300 mlen) and/or colloids (average 500 mlen). Apart from vascular filling, vasopressor amines were also used, notably ephedrine by bolus of 6 to 12 mg. Norepinephrine was administered in 3.33% of patients. Adrenaline was only used in the patient, which is 3.33% for the management of an intraoperative cardiac arrest. It is currently recommended to start the transfusion early. The target being around 9 to 10 g of hemoglobin as long as the hemorrhage is active. The transfusion of fresh frozen plasma (FFP) must also be started quickly with an RBC/FFP ratio close to 1 without waiting for the result of the hemostasis assessment [15]. A third of the patients, 33.33%, were transfused with whole blood and 30% received a single bag. In the study of Sene [5], a blood transfusion was performed in 94.59% of the patients.
This state of affairs is due to several factors. First, there are regular shortages of blood components at the blood bank of the Ziguinchor Peace Hospital, then the use of whole blood is justified by the lack of centrifugal apparatus to prepare bags of RBC (red blood cells), FFP or platelet concentrates. Tranexamic acid was used in 73.3% of the workforce. It is a drug used for its anti-fibrinolytic properties. The evidence for its effectiveness is growing. Several studies and publications have been made on its effectiveness in the treatment of postpartum hemorrhages and in the prevention of bleeding [19]. All patients received antibiotic prophylaxis based on cefazolin as recommended by the French Society of Anaesthesia, Critical Care and perioperative Medecine (SFAR) [20]. Oxytocin was administered in 93.3% of patients. The two patients in whom oxytocin were not administered are those in whom an indication of hysterectomy or hemostasis was immediately established. Apart from fetal extraction, a hemostasis hysterectomy was performed in 13.3% of patients. This radical gesture performed in our series was well above that of Sene [5] which noted 2.4% hysterectomy. Unlike in the study of Sene [5] where admission to intensive care following surgery was done in 100% of the patients, in our series 50% were admitted to intensive care. No deaths were noted. The results were favorable.
Conclusion
Despite much progress in improving maternal and child health, many challenges remain, especially in developing countries. The anesthetic management of obstetric hemorrhagic pathologies involves the availability of anesthetic products such as etomidate, ketamine and better access to blood products in all health facilities. General anesthesia should be performed in these patients according to the Lucas classification.
References
- Boisramé T, Sananès N, Fritz G (2014) Abruption placentae. Diagnosis, management and maternal-fetal prognosis: a retrospective study of 100 cases. Gynecol Obstet Fertil (4292): 78-83.
- (2025) Maternal mortality.
- (2023) Continuous Demographic and Health Survey (DHS-Continuous) Report.
- (2016) National College of French Gynecologists and Obstetricians. Updates in Obstetrics.
- Sène A (2022) Management of PMH in intensive care at the regional hospital of Diourbel: about 41 cases. Med Thesis, Dakar, Senegal.
- Niass A (2019) The retroplacental hematoma in Dakar: a multicenter case-control study. Med Thesis, Dakar, Senegal.
- Diarra S (2007) Retroplacental hematoma in the gynecology-obstetrics department of the reference center of commune V of the district of Bamako. Thesis Med Bamako Mali.
- Aaboudech T (2018) Retroplacental hematoma fetus living at the maternity hospital of SOUISSI in Rabat. Thesis Med. Rabat, Morocco.
- Kanta SI (2021) Retroplacental hematoma (RPH) in the gynecological-obstetrics department of the Somine Dolo Hospital in Mopti. Med. Thesis Bamako, Mali.
- Thiam O, Mbaye M, Diouf AA, Touré FB, Gueye M, et al. (2014) Epidemiological, prognostic and therapeutic aspects of HRP in a reference maternity hospital in a rural area. Pan Afr Med J 17: 11.
- Thiéba B (2003) Retroplacental hematoma: epidemioclinical and prognostic aspects of a series of 177 cases in Gynecology, Obstetrics & Fertility 31(5): 429-33.
- Kilani K (2012) Retroplacental hematoma: Retrospective study in the department of gynecology and obstetrics "B" over 5 years at the Mohamed VI University Hospital of Marrakech. Thesis Med Marrakech, Morocco.
- Diallo AB (2019) In utero fetal deaths at the Pikine National Hospital: analysis and etiological approach from January 1, 2018 to December 31, 2019. Thesis Med Dakar, Senegal.
- Guissé E (2022) Epidemiological, diagnostic, therapeutic and prognostic aspects of retroplacental hematoma at the Fatick Regional Hospital Center. Med Thesis, Dakar, Senegal.
- Dia CA (2021) Emergency caesarean section anesthesia at the Saint-Louis Regional Hospital Center: about 195 cases. Med Thesis 2021, Dakar, Senegal.
- Mian DD, Angoi V, Nguessan KLP, Abauleth YR, Kouakou F, et al. (2014) Retroplacental hematoma (RPH) and fetal death in utero (MFIU): about 70 cases and literature review. Rev Afr anesth Med Emergency 19: 37-42.
- Meniolle F, Dadure C, Morau E (2018) Caesarean section under general anesthesia: what's new? Prat En Anesth Resuscitation 22(6): 342‐345.
- Vial F, Herbain D (2020) Prevention and management of intraoperative memorization during caesarean sections under general anesthesia. Prat En Anesth Resuscitation 24(3): 151-161.
- Dakar, Senegal (2024) Evaluation of the effects of tranexamic acid on bleeding during caesarean section: a comparative study of 60 cases at the Peace Hospital of Ziguinchor (Senegal). Mémoire Med 330.
- (2024) Antibiotic prophylaxis in surgery and interventional medicine.






























