Abstract
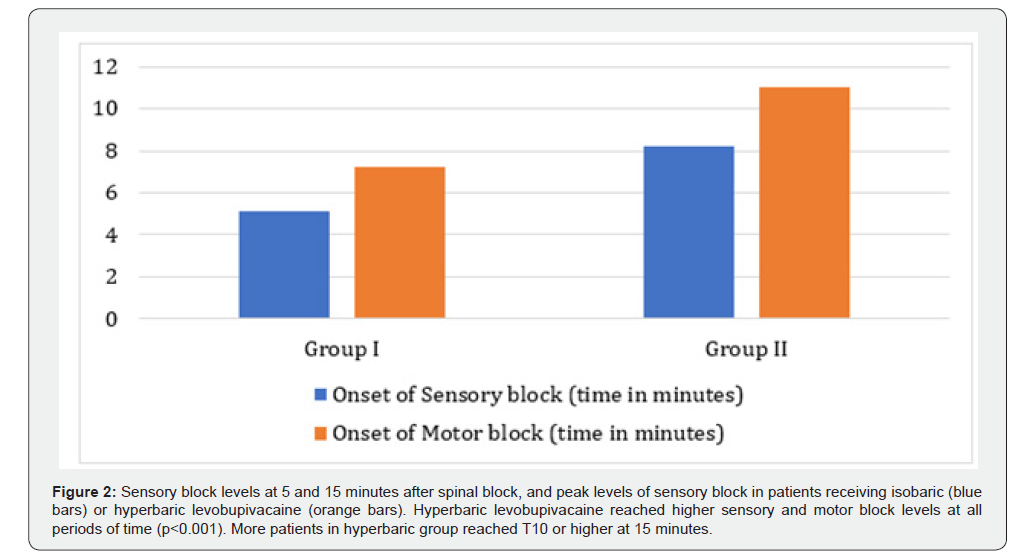
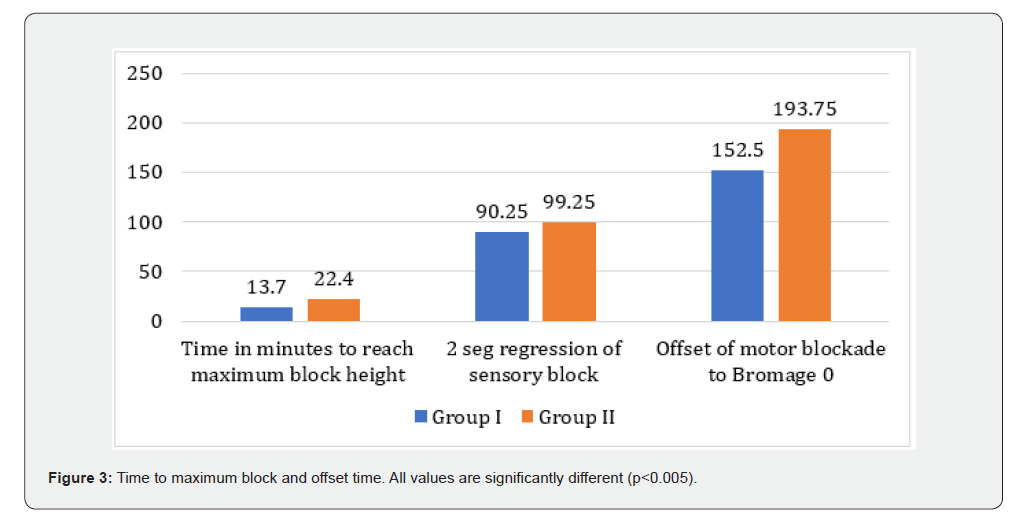
Spinal anesthesia is a common anesthetic technique for infraumbilical surgeries The small dose of local anesthetics required, and intense sensory, motor and sympathetic blockade make it an attractive option. Bupivacaine, conventionally used for spinal anesthesia has a long duration of action. However, it is limited by toxicity especially of the cardiovascular and central nervous system. Levobupivacaine, the S(-) enantiomer of bupivacaine, has the advantage of less cardiotoxicity and a more predictable spread of sensory block. Few studies have been done comparing effects of hyperbaric levobupivacaine with its isobaric form in infraumbilical surgeries. The present study compared intrathecal hyperbaric levobupivacaine and plain levobupivacaine in patients undergoing infraumbilical surgeries. We randomly assigned patients into two groups. Group I received 2.52 ml 0.5% levobupivacaine + 0.48 ml 50% dextrose (hyperbaric 0.42% levobupivacaine) and Group II who received 2.52 ml 0.5% levobupivacaine + 0.48 ml 0.9% normal saline (isobaric 0.42% levobupivacaine). We found that in hyperbaric levobupivacaine group, both sensory and motor block occurred earlier (7.25 ± 1.68 min vs 11.00 ± 1.747 min, <0.001). The level of T8 or higher was reached in 90% of cases in the hyperbaric group compared with 70% in the isobaric group (P = 0.007). The time to reach maximum height of block was faster in hyperbaric levobupivacaine group (13.70 min vs 22.40 min, p< 0.001). Two segment regression of sensory block (90.25 min vs 99.25 min, <0.001), offset of motor block (152.50 min vs 193.75 min) was faster in hyperbaric levobupivacaine group
Our results suggest that hyperbaric levobupivacaine was more predictable for sensory block level and had shorter duration of action making it more suitable for day care surgery.
Conclusion: Delirium in ICU patients is common and associated with increased morbidity and mortality. Early identification and targeted interventions may help mitigate adverse outcomes.
Keywords:Levobupivacaine; Hyperbaric; Infraumbilical Surgeries; Sensory and Motor Blocks
Abbreviations:BMI: Body Mass Index; CTRI: Clinical Trials Registry; PACU: Post-Anesthesia Care Unit; CSF: Cerebrospinal Fluid
Introduction
Spinal anesthesia is an established technique for providing anesthesia for infraumbilical surgeries, as it is safe, effective and easy to perform technique. It requires small doses of local anesthetics and produces intense sensory, motor and sympathetic blockade. Bupivacaine, used for spinal anesthesia is known to have central nervous system toxicity (light headedness, visual and auditory disturbances, drowsiness, convulsions), and adverse cardiovascular effects (arrhythmias, myocardial depression) [1] Bupivacaine exists in two isomeric forms, S (-) and R (+). The S (-) enantiomer of bupivacaine, levobupivacaine has the advantage of less cardiotoxicity in the event of accidental intravascular injection [2] The commercial preparation of levobupivacaine is isobaric with CSF (1.0003+/-0.0003) while bupivacaine is available in both isobaric and hyperbaric form. For the purpose of this study levobupivacaine was made hyperbaric by the addition of dextrose. Few studies have compared the isobaric to the hyperbaric form of levobupivacaine. There is very little evidence regarding its efficacy, especially in infra umbilical surgeries [2]. This study aimed to observe the level of sensory and motor blockade and offset of block achieved with hyperbaric levobupivacaine as compared to plain levobupivacaine in infra umbilical surgery. Adverse effects if any of was considered as secondary outcome.
Methods
This prospective double blind randomised control study was conducted in a 750-bed tertiary care centre, after approval by the Institutional Ethics Committee (Number). It has been registered with the Clinical Trials registry (CTRI/2022/03/040877). All consecutive adult patients of either gender aged 18-60 years, ASA I - III patients undergoing infraumbilical surgeries were enrolled after informed consent. Patients with a past history of spine surgery, local infection, coagulopathy, hypersensitivity to local anesthetics, obesity (defined as Body Mass Index (BMI) >30), and pregnancy were excluded.
Study Design
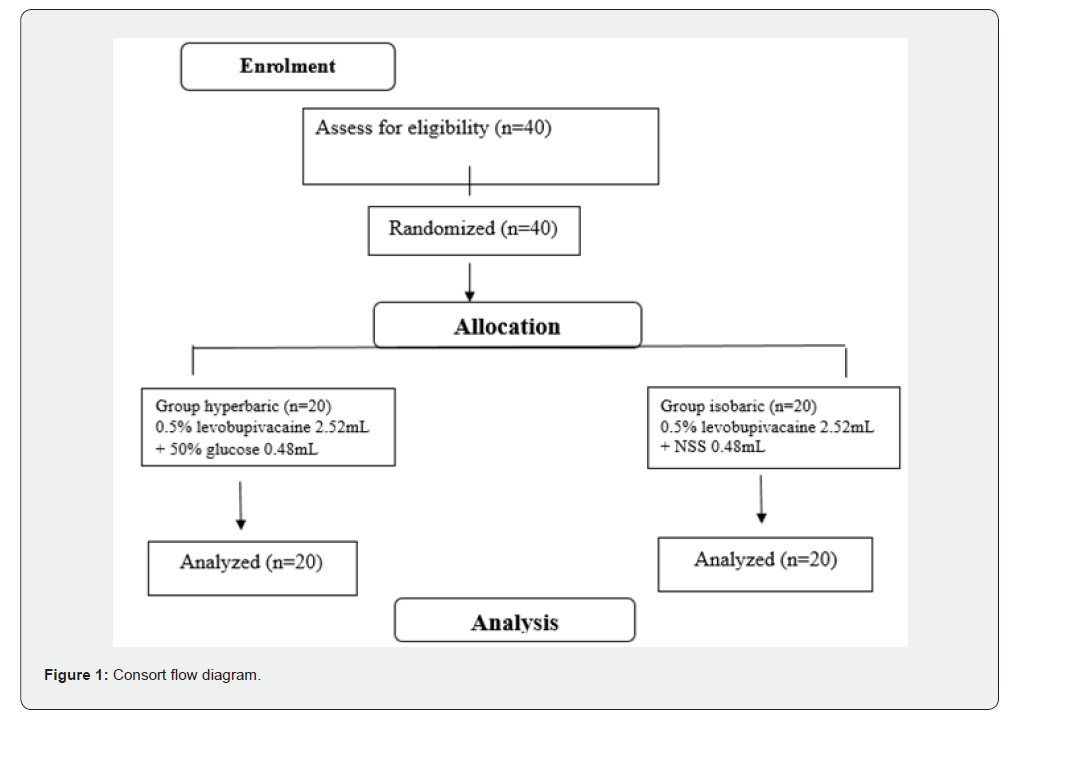
The patients were randomly allocated into two groups, to receive either isobaric or hyperbaric levobupivacaine ((Neon Laboratories Ltd). Both solutions were prepared immediately prior to surgery by an anesthesiologist, who was not involved in the study. A total volume of 3 ml was prepared in both the groups.
Group I (n= 20) : 2.52 ml 0.5% levobupivacaine + 0.48 ml 50% dextrose
Group II (n= 20) : 2.52 ml 0.5% levobupivacaine + 0.48 ml 0.9% normal saline
A thorough preanesthetic examination, relevant investigations as indicated was done for all the patients. All patients were kept fasting for 6 hours prior to surgery. Premedication included oral alprazolam 0.25 mg and ranitidine 150 mg, given the night before and on the morning of surgery. After securing venous access with a 20 G intravenous cannula on the non-dominant hand of the patient, pre loading was done with Ringer lactate infused at the rate of 5-6ml/kg body weight. Baseline heart rate, systolic and diastolic blood pressure, and oxygen saturation (SpO2) was recorded. The patient was placed in left lateral position. Under sterile condition, lumbar puncture was performed at the L3- L4 level through mid-line approach using a 25-gauge Quincke needle. After the study drug was injected, the patient was turned supine immediately. Oxygen was delivered through a venturi mask with fractional inspired oxygen (FiO2) of 0.4. In the event of traumatic or failed lumbar puncture, the patient was excluded from the study. Standard monitoring included ECG, SpO2 and NIBP (systolic, diastolic and mean blood pressure). Recording was done every minute for the first 10 minutes, every 5 minutes till 60 minutes then every 10 minutes for 120 minutes or the end of surgery whichever was earlier. The parameters were recorded every half hourly in the post-anesthesia care unit (PACU).
Data Collection
From the time of intrathecal injection (taken as zero minute), the sensory and motor block was recorded by an investigator blinded to the type of solution, every minute for first 15 minutes, and then every 15 minutes for 120 minutes. Sensory level was checked by swab dipped in ether, bilaterally along the midclavicular line. The motor block was graded according to the modified Bromage score 0-3 (where score zero indicated no motor block, and score 3 complete motor block). Bromage score of score ≥2 and no response to pain as tested by the surgeon was the criteria to allow surgical incision. The time of onset of the block was taken as time to loss of sensation at T8 level. The maximum height of block was also recorded. Duration of the block was be taken as the duration from time zero to the time taken for two segment regression. For the purpose of the study hypotension was defined as a decrease in systolic blood pressure to <90mmHg and was treated with a rapid IV fluid bolus or ephedrine (6-12mg). Bradycardia was defined as heart rate <50/min and treated with IV atropine. Patients were monitored for two hours in PACU. Adverse events were recorded.
Randomisation
Allocation of the patients to the two groups was done by computer-generated random numbers kept in serially numbered opaque-sealed envelopes with alphabetic codes. Once the patient reached the operation theatre, the envelopes (containing the random number) was opened, and the patient’s data and the code was sent to the control analyst for uploading on the excel spread sheet.
Statistics & Sample Size Estimation
With the reference of previous study [2] a difference of 3.8 min in time to T10 sensory block was considered as clinically significant. A sample size of 20 per group was required to detect a significant difference for a α error of 0.05, power of 80% and pooled SD of 3.7. Continuous variables were presented as mean ± SD or median (IQR) depending on data distribution. Categorical variables are expressed as frequencies and percentages. Student’s t test and Mann Whitney U test was used for continuous variables. Chi-square test or Fisher’s exact test was used for categorical data. Statistical testing was done with the statistical package for the social science system version SPSS 27.0. A p value< 0.05 was considered significant.
Results
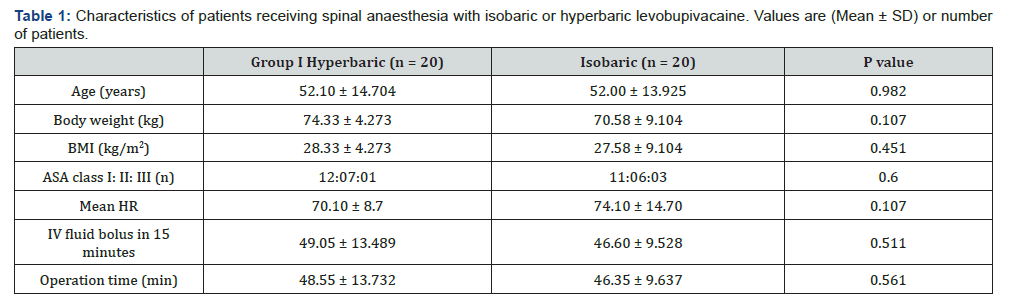
A total of 40 patients were included in the study out of which 20 patients (Group I) received hyperbaric levobupivacaine and 20 received isobaric levobupivacaine (Group II) (Figure 1). The two groups were similar with respect to age, height, weight, BMI, ASA status, amount of IV fluid given, and duration of operation (Table 1). Types of operation were similar. The mean onset of sensory block, mean onset of motor block, height of maximum block and time to reach height of maximum block was earlier in Group I and were statistically significant (Figure 2). Two segment regression of sensory block (90.25 vs 99.25 min) and motor blockade offset to Bromage 0 (152.50 vs 193.75 min) was faster in Group I and was statistically significant (Figure 3).
Discussion
In this study we compared equal doses of hyperbaric and plain levobupivacaine with regard to sensory and motor block, height of maximum block and duration of block. Both the time of onset and offset of motor and sensory blockade were significantly faster with hyperbaric levobupivacaine. The side effects were similar between the groups. Similar findings have been reported in other studies [3]. A randomized, double blind study in healthy volunteers compared 0.25% hyperbaric levobupivacaine and racemic bupivacaine for spinal anesthesia. Sensory and motor block were found to be similar for the same doses of 4 mg levobupivacaine, 8mg bupivacaine, and 12mg hyperbaric levobupivacaine. They concluded that intrathecal levobupivacaine can be a substitute for bupivacaine, and secondly hyperbaric 0.25% levobupivacaine can be suitable for outpatient spinal anesthesia [4]. In another study in the context of outpatient anesthesia, intrathecal 40mg and 60 mg 2% hyperbaric prilocaine was compared with 60 mg 2% plain prilocaine.
The hyperbaric solutions had shorter duration of surgical block, and faster recovery, making it ideal for short procedures [5] The shorter duration of action may be due to the baricites or specific gravity of the solution in comparison to cerebrospinal fluid (CSF). In a study on patients undergoing lumbar discectomy recovery times was reported to be significantly shorter in the isobaric levobupivacaine group as compared to bupivacaine allowing early mobilization [6] Similar to other studies, the duration of motor and surgical block was significantly shorter with hyperbaric levobupivacaine [6,7] which can be explained by faster clearance of levobupivacaine as compared to racemic bupivacaine [8]. Our study is not without limitation, the foremost being a relatively small sample size which may not allow extrapolation of the result in other settings. In addition, the study was not powered to detect rare complications such as transient neurological complications associated with spinal levobupivacaine.
Conclusion
Our results have shown that the clinical efficacy of hyperbaric levobupivacaine was superior to the isobaric form for spinal anesthesia during infraumbilical surgeries. Compared with isobaric levobupivacaine, it had a shorter duration of sensory and motor block, allowing earlier recovery and mobilization. Hence, levobupivacaine can be a safer alternative for infraumbilical surgeries of short duration.
Study data availability
Anonymised data may be requested with reasonable justification from the corresponding author and will be shared as per the authors’ Institution policy.
References
- Gristwood RW (2002) Cardiac and CNS toxicity of levobupivacaine: strengths of evidence for advantage over bupivacaine. Drug Safety 25(3): 153-163.
- Sen H, Purtuloglu T, Sizlan A, Yanarates O, Ates F, et al. (2010) Comparison of intrathecal hyperbaric and isobaric levobupivacaine in urological surgery. Minerva Anestesiologica 76(1): 24-28.
- Sanansilp V, Trivate T, Chompubai P, Visalyaputra S, Suksopee P, et al. (2012) Clinical characteristics of spinal levobupivacaine: hyperbaric compared with isobaric solution. Scientific WorldJournal 2012: 169076.
- Alley EA, Kopacz DJ, McDonald SB, Liu SS (2002) Hyperbaric spinal levobupivacaine: a comparison to racemic bupivacaine in volunteers. Anesth Analg 94(1): 188-193.
- Camponovo C, Fanelli A, Ghisi D, Cristina D, Fanelli G, et al. (2010) A prospective, double-blinded, randomized, clinical trial comparing the efficacy of 40 mg and 60 mg hyperbaric 2% prilocaine versus 60 mg plain 2% prilocaine for intrathecal anaesthesia in ambulatory surgery. Anesth Analg 111(2): 568-572.
- Şahin AS, Türker G, Bekar A, Bilgin H, Korfalı G, et al. (2014) A comparison of spinal anesthesia characteristics following intrathecal bupivacaine or levobupivacaine in lumbar disc surgery. Eur Spine J 23(3): 695-700.
- Guler G, Cakir G, Ulgey A, Ugur F, Bicer C, et al. (2012) A Comparison of Spinal Anesthesia with Levobupivacaine and Hyperbaric Bupivacaine for Caesarean Sections: A Randomized Trial. Anesthesiology 2(3): 84-89.
- Burm AG, Van der Meer AD, Van Kleef JW, Zeijlmans PW, Groen K, et al. (1994) Pharmacokinetics of the enantiomers of bupivacaine following intravenous administration of the racemate. Br J Clin Pharmacol 38(2): 125-129.






























