Abstract
Background & Aim: Delirium is common but unrecognized in critically ill patients. The study attempted to identify the incidence, risk factors and outcomes of delirium in mechanically ventilated patients, admitted in the intensive care unit (ICU).
Methods: The Confusion Assessment Method-ICU (CAM-ICU) scale was used to identify patients having delirium. Patients who are diagnosed to have delirium and risk factors associated with it were identified. Data regarding age, co morbidities, usage of drugs. Other variables recorded included 28-day hospital mortality, days on mechanical ventilation, length of stay in the ICU, hospital length of stay and need for home care services.
Results: A total of 151 patients were enrolled in the study. The median age of the cohort was 58 years (IQR 46.0-68), and majority 128 (84.8%) were males and 87 (57.6%) were more than 60 years of age. The crude mortality in the cohort was 35.76%. Delirium was identified in 75 patients (49.7%). The mortality was significantly higher in the delirium group. The multivariate analysis showed CNS involvement, and Chronic lung disease to be the strongest predictor besides both severity scoring systems after adjustment. Several factors significant in univariate analysis including age, opioid use, and physical restraints lost their significance in the multivariate model.
Conclusion: Delirium in ICU patients is common and associated with increased morbidity and mortality. Early identification and targeted interventions may help mitigate adverse outcomes.
Keywords:CAM-ICU; Delirium; Diagnosis; Intensive Care Unit; Mortality; Risk factors
Abbreviations:APACHE II: Acute Physiology And Chronic Health Evaluation II; CAM-ICU: Confusion Assessment Method - Intensive Care Unit; CVC: Central Venous Catheter; CKD: Chronic Kidney Disease; COPD: Chronic Obstructive Pulmonary Disease; CI: Confidence Interval; DM: Diabetes Mellitus; HTN: Hypertension; ICU: Intensive Care Unit; ICDSC: Intensive Care Delirium Screening Checklist; IQR: Interquartile Range; MV: Mechanical Ventilation; OR : Odds Ratio; RASS: Richmond Agitation Sedation Scale; SD: Standard Deviation; SOFA : Sequential Organ Failure Assessment
Introduction
Delirium is common in hospitalized patients but may go unrecognized. The reported prevalence of delirium in mechanically ventilated patients is 50-80% [1]. The consequences of delirium in the intensive care unit (ICU) patients besides increased mortality include prolonged stay in the hospital thereby increasing the hospital cost. It is also associated with increased rates of self-harm including self-extubation, removal of feeding tubes and intravascular devices [2]. The patient related risk factors for delirium include old age, severity of illness, excessive alcohol intake and smoking, past history of hypertension and neurological condition such as Parkinsonism and seizure disorder. Iatrogenic factors such as use of physical restraint, infusions of sedatives, and anti-psychotic drugs have also been implicated for the development of delirium. Strategies to decrease exposure to sedative drugs such as protocol-based sedation or daily interruption of sedation have been tried to lower the risk of delirium [3]. The confusion assessment method for the intensive care unit (CAM-ICU) and intensive care delirium screening checklist (ICDSC) is most commonly used for the diagnosis of delirium [4]. Very few studies have been carried out in India to measure the prevalence and outcomes of patients experiencing delirium during their ICU stay [5]. The information about possible long-term outcomes in these patients is lacking. This prospective observational study aims to study the risk factors, and outcomes of delirium in mechanically ventilated adults admitted to the ICU
Study Design and Methods
The study was carried out in a 62 bed ICU in a tertiary care hospital of North India. The primary objective was to identify the risk factors for delirium. The secondary objectives were to assess the outcomes in terms of incidence, length of stay in ICU and hospital, and hospital mortality. The duration of mechanical ventilation (MV) and the need for Home Care Services after hospital discharge were also included as secondary outcomes. Level of arousal was measured by using the Richmond Agitation Sedation Scale (RASS),6which is a 10-point scale ranging from + 4 to −5, with a RASS score of 0 denoting a calm and alert patient. The patients who were ventilated >48 hours, in the age group 18-80 years, Richmond Agitation Sedation Scale (RAAS) score -3 and above, and potential candidates for weaning were enrolled. Post cardiac arrest, traumatic brain injury, and patients who received neuromuscular blockers, propofol, ketamine, and dexmedetomidine were excluded.
Data Collection and Outcome Measurements
Data was collected in a predefined case-record form developed for the study. The following information was extracted from the patient records: [1] demographic characteristics [2] risk factors for development of delirium - (age and gender, co-morbidities such as coronary artery disease, prior neurological conditions, dementia, chronic renal and liver disease, addiction to alcohol and smoking, cumulative doses of midazolam, fentanyl, antipsychotic and anti-cholinergic medications and others) [3]. Days to the diagnosis of delirium after admission, primary specialty (surgical/ medical) [4] severity scores (APACHE, SOFA) on admission, [5] outcome parameters (hospital mortality, days on MV, length of stay in the ICU, hospital and need for home Care services after hospital discharge) [6]. The incidence of tracheostomy, physical restraint use, accidental device removal (endotracheal or gastric tube, vascular catheters) was recorded. For the purpose of the study home care services was defined as 24 hours professional nurse in attendance to take care of essential needs such as bed bath, oral care, medication, enteral feed and care of tracheostomy. Readiness to wean was assessed daily using standardized criteria, and a T-piece trial was initiated when the criteria were met . If the RAAS score -3 and above, the first screening for delirium was done. Duration of delirium was defined as the number of days in the study period during which patients were CAM-ICU positive and were not comatose . The patients were followed up till hospital discharge or death whichever occurred earlier. The ICU and hospital length of stay, days on MV and tracheostomy if done was recorded. The need for professional home care was also recorded at the time of discharge.
Sample size and Statistics
With estimated prevalence of delirium in mechanically ventilated patients as 53.8% 5 and 8 risk factors in the equation, the calculated sample size was 148 . We recruited 151 patients for the study Statistical analysis was done using statistical package for the social science (SPSS) system version SPSS 28.0. Continuous variables were described as mean (±SD) or medians and interquartile ranges [IQR] depending on data distribution. Frequencies and percentages (%) were used to describe categorical variables . Continuous variables with normal distribution were compared by Students’ T test, those with skewed distribution were compared using Mann Whitney U test . Categorical data between the groups were compared using Chi-squared test or Fisher’s exact test as appropriate. To assess the risk factors for delirium, univariate analysis and multivariate analysis was conducted and the factors which were found significant were subjected to logistic regression, to assess the factors independently associated with delirium. A p value < 0.05 was considered significant .
Results
A total of 151 patients were enrolled in the study after an informed consent obtained from the next of kin of the patients, and approval from the Institutional Ethics Committee (vide EC/07/22/2110). The study is registered with the Clinical Trials Registry (CTRI/2022/10/046323). The demographic characteristics of the patients is depicted in (Table 1). The Median age of the cohort was 58 years (IQR 46.0-68), and majority of the patients 128 (84.8%) were males and 87 (57.6%) were more than 60 years of age. Among the major risk factors, CNS involvement was found in 34 (22.5%) and chronic kidney disease in 40 (26.5%) patients. Chronic Liver Disease in 29 (19.2%) and history of alcohol intake in 22 (14.6%). 131 (86.8%) of patients received opioids. Only 5 (3.3%) of the patients received benzodiazepines. The median dose of opioid given was 3.05 mg (IQR 1.5 – 6.03). The opioids were given for a mean duration of 4.35 ± 2.92 days. the median dose was 99.00 mg (IQR 39.00-300.00) for a mean duration of 6.00 ± 6.32 days. On day 1 CAM was positive in 66 (43.7%) of patients and on day 8 it was positive in 68 (45.0%) of cases. 54 (35.76%) patients died while 97 (64.2%) survived to discharge resulting in a crude mortality of 35.76%. The duration of MV days median (IQR) was 4 (3-10) days. The median (IQR) LOS in ICU (days) was 08 (5.0-15), and the median LOS in hospital (days) was 11 (7.25.- 23.0) in the entire cohort.
Univariate Analysis
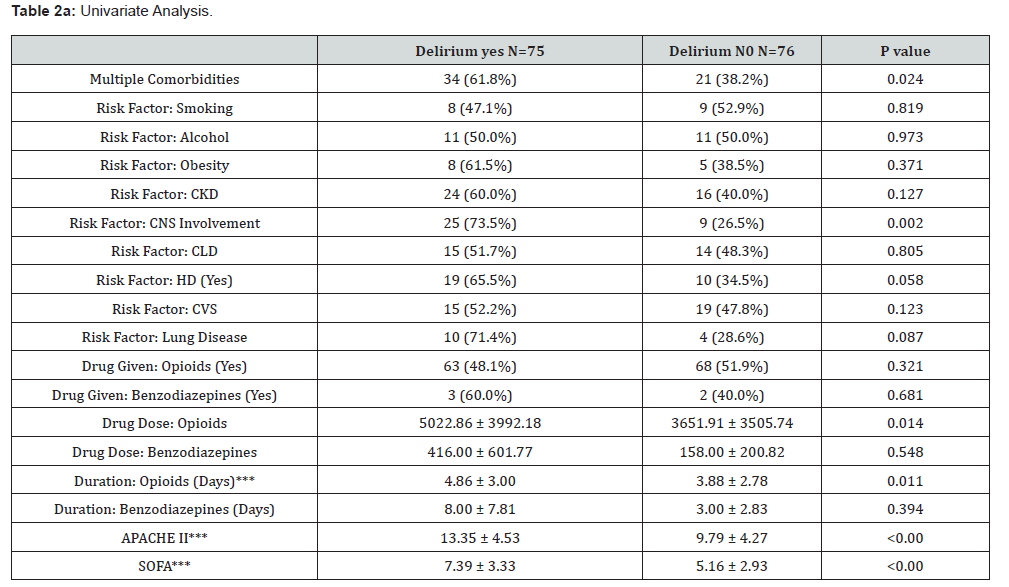
To identify potential risk factors for delirium, we performed univariate analysis comparing 75 patients who developed delirium with 76 who remained delirium-free during their ICU stay (Tables 2a, 2b). Patients developing delirium were significantly older (59.93 ± 14.23 vs 52.97 ± 15.99 years, p=0.005), with 61.8% of the delirium group having three or more comorbidities compared to 38.2% in the non-delirium group (χ2 = 5.108, p=0.024). Among specific risk factors evaluated, CNS involvement showed the strongest association with delirium, being present in 73.5% of delirious patients versus 26.5% of non-delirious patients (χ2 = 9.993, p=0.002). Chronic lung disease was also more prevalent in the delirium group (71.4% vs 28.6%, p=0.087), though this did not reach statistical significance. The severity scores APACHE II and SOFA Scores were significantly higher in the patients who had delirium. Among the 75 patients who had delirium, majority 66 had delirium on day 1 of the study (when weaning was initiated) and this continued till day 8, when 68 of 75 patients continued to experience delirium. The relative risk of developing delirium on day 8 was 11.86 (CI 6.1-24.12).
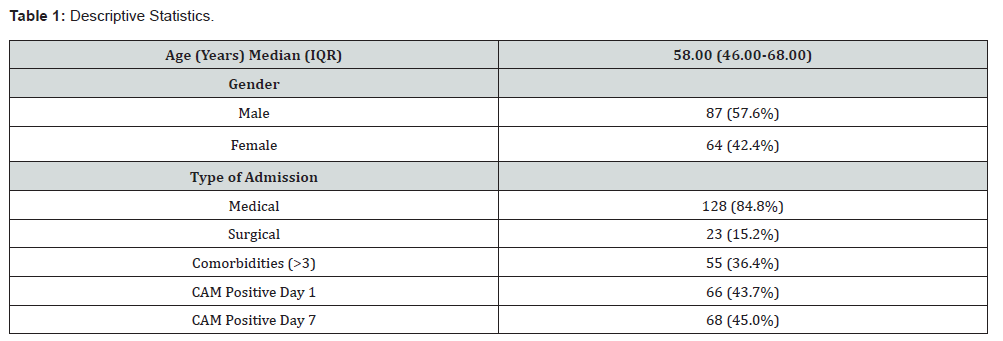
N=151
CAM: Confusion Assessment Method
Summary of Outcomes
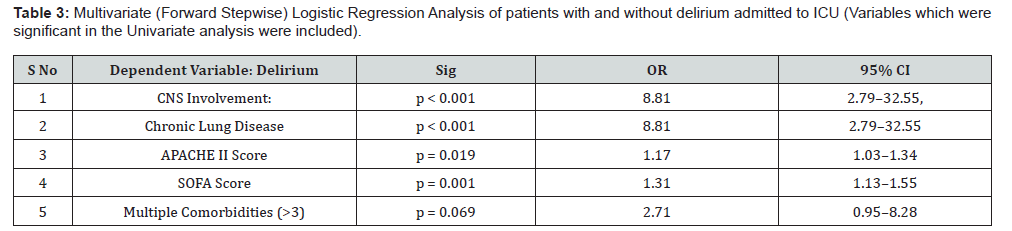
Model Fit: Chi-Square (χ²): 63.74, p < 0.001, Pseudo-R²: 0.30, AIC: 183.6
Discrimination Ability: C-statistic: 0.85, Calibration: Hosmer- Lemeshow test: χ² (8) = 3.04, p = 0.932 OR odds ratio, CI confidence interval, SOFA sequential organ failure Score, APACHE Acute Physiology and chronic health evaluation score, CNS Central Nervous System ICU: Intensive Care Unit.
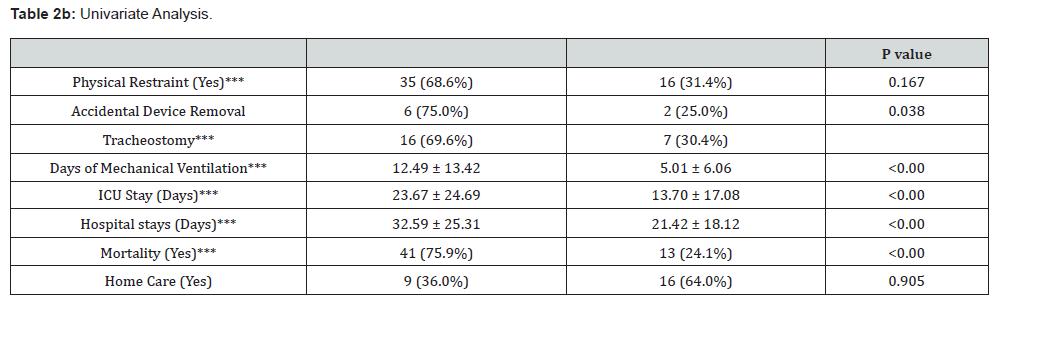
Regarding medication exposure, while the majority of patients in both groups received opioids (86.8%), those developing delirium received higher cumulative doses (5022.86 ± 3992.18 vs 3651.91 ± 3505.74 mg, p=0.014), for longer durations (4.86 ± 3.00 vs 3.88 ± 2.78 days, p=0.011). Use of physical restraint was higher in patients who developed delirium (68.6% vs 31.4%, χ2 = 11.072, p<0.001). Interestingly, gender, type of admission (medical vs surgical), and other comorbidities showed no significant association. During the study period, from among a total of 75 patients who experienced delirium 41 (75.9%) died, and the mortality in the delirium absent group was 24.1%. The relative risk of mortality in patients experiencing delirium was 2.17 (1.59- 2.97). Among the 97 (64.2%) survivors, only 9 of 37 delirium positive patients (36.0%)s discharged needed home care, while 16 (64.0%) out of a total of 63 discharged patients who did not experience delirium needed home care, (χ2 = 0.014, p = 0.905). (Table 2b).
Multivariate Analysis
To determine independent predictors of delirium while controlling for confounding factors, all variables with p<0.05 in univariate analysis were entered into a forward stepwise logistic regression model. The final model demonstrated robust performance with excellent discriminative ability (C-statistic: 0.85), good calibration (Hosmer-Lemeshow test: χ² (8) = 3.04, p=0.932), and explained 30% of the variance in delirium occurrence (Pseudo-R² = 0.30). In the multivariate analysis CNS involvement proved to be the strongest predictor, increasing the odds of delirium nearly nine-fold (adjusted OR: 8.81, 95% CI: 2.79-32.55, p<0.001). This finding underscores the vulnerability of patients with pre-existing neurological conditions. Chronic lung disease, which showed only a trend in univariate analysis, emerged as a significant independent predictor in the multivariate model, increasing delirium risk over six-fold (adjusted OR: 6.73, 95% CI: 1.35-41.96, p=0.027), likely reflecting the impact of hypoxemia and respiratory failure on cognitive function. Both severity scoring systems retained their predictive value after adjustment. The presence of multiple comorbidities (≥3) showed a trend towards significance (adjusted OR: 2.71, 95% CI: 0.95-8.28, p=0.069), suggesting cumulative health burden may contribute to delirium risk. Notably, several factors significant in univariate analysis-including age, opioid use, and physical restraints-lost their significance in the multivariate model, indicating these associations were likely mediated through illness severity and organ dysfunction. (Table 3).
Discussion
In this observational study the incidence of delirium was found to be 66 (43.7%). The relative risk of developing delirium on day 8 was 11.86 (CI 6.1-24.12). The incidence of delirium is similar to that reported in other studies [7]. Few studies from Asia have reported lower incidence of delirium [8,9]. However, these studies excluded patients with cognitive and neurological disorders which suggests that patients with neurological disorders may be prone to delirium, a finding which has been shown in this study. An Indian study reported an incidence of 24.4%, which was much less than that in our study [10]. The possible reason for this difference is that our study was done in critically ill ventilated patients and our patients were older. The association of gender disparity to delirium has been reported earlier, with both males 10 and females 11 showing higher predisposition to develop delirium. We did not find any significant difference in the occurrence of delirium in either sex which suggests that gender alone might not be a risk factor contributing to delirium. Higher dose and duration of opioid use have been a major risk factor in our study. Similar findings have been reported in other studies [6]. Midazolam usage has been reported with higher incidence of delirium. In two studies the usage of midazolam was implicated, for but in our study, we have used midazolam in only 5 patients and antipsychotics were not used at all, in any of the patients [3,11]. In the multivariate analysis, the risk factors identified in this study were CNS involvement, Chronic lung disease, the severity Scores and the presence of >3 co morbidities. Other risk factors such as cardiovascular disease, chronic heart failure and presence of psychiatric illness did not show any association with delirium [12]. A previous study has found preexisting cognitive impairment as a major risk factor for delirium, besides diabetes, chronic kidney failure and male gender in multivariate analysis.
The risk factors identified in a systematic review by multivariate analysis respiratory disease, old age, alcohol abuse, and dementia (classified as predisposing factors), electrolyte abnormalities, fever, vasopressor requirement, high opioid dose, and metabolic acidosis (classified as precipitating factors), because they were related the patient’s underlying disease [13]. Medications commonly associated with delirium include anticholinergic agents, benzodiazepines, and opioids. There is moderate evidence that multiple organ failure is a risk factor for delirium. A recently published prospective observational study also reported similar findings in the Indian context [14]. Longer duration of mechanical ventilation in patients having delirium as shown in our study has also been reported by other studies [11,15]. Similar to other studies [15,16] our mortality in patients with delirium was higher (75.9% vs 24.1%). In a large retrospective analysis, acute delirium was associated with 32% increased odds of in‑hospital mortality. The limitations of the study include a small sample size, and observational design, which can only establish associations not causality. Other factors not included in the analysis may influence delirium risk. Ambient light and noise in the ICU contributed to delirium but this aspect was not included in the approved protocol. Future prospective studies may be done to establish causal relationships between identified risk factors and delirium. Further, this study was also not designed or powered to determine the role of delirium to adverse outcomes such as length of stay, cost, or mortality. Our study highlights the importance of prevention of modifiable risk factors like duration of mechanical ventilation and opioid use which could lessen the incidence of delirium. This in turn could further impact the stay in ICU/hospital and mortality. Usage of physical restraint should be limited in cases of severe agitation and self-harm. Approaches like the ABCDE bundle [17] and Clinical Practice Guidelines for the Management of Pain, Agitation, and Delirium (PAD) [18] must be followed in patients especially with those of non-modifiable risk factors like underlying co morbidities.
Summary & Conclusions
The study identifies CNS involvement, chronic lung disease, use of opiods and higher severity scores as independent predictors of delirium in ICU patients. Delirium is a significant complication in hospitalized patients, associated with increased morbidity and mortality. By identifying and addressing modifiable risk factors, healthcare professionals can play a crucial role in mitigating this condition and enhancing patient care.
References
- Salluh JI, Soares M, Teles JM, Ceraso D, Raimondi N, et al. (2010) Delirium Epidemiology in Critical Care Study Group. Delirium epidemiology in critical care (DECCA): an international study. Crit Care 14(6): R210.
- Zaal IJ, Devlin JW, Peelen LM, Slooter AJ (2015) A systematic review of risk factors for delirium in the ICU. Crit Care Med 43(1): 40-47.
- Mehta S, Cook D, Devlin JW, Skrobik Y, Meade M, et al. (2015) SLEAP Investigators; Canadian Critical Care Trials Group. Prevalence, risk factors, and outcomes of delirium in mechanically ventilated adults. Crit Care Med 43(3): 557-566.
- Gusmao-Flores D, Salluh JIF, Chalhub RA, Quarantini LC (2012) The confusion assessment method for the intensive care unit (CAM-ICU) and intensive care delirium screening checklist (ICDSC) for the diagnosis of delirium: a systematic review and meta-analysis of clinical studies. Crit Care 16(4): R115.
- Sharma A, Malhotra S, Grover S, Jindal SK (2012) Incidence, prevalence, risk factor and outcome of delirium in intensive care unit: a study from India. Gen Hosp psychiatry 34(6): 639-646.
- Ely EW, Truman B, Shintani A (2003) Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS). JAMA 289(22): 2983-2991.
- Martinez FE, Ho VW, Brogan G, Pickering C, Leung G, et al. (2021) Period-Prevalence and Risk Factors for Delirium in a Tertiary Referral ICU: A prospective cohort study. Acute Med 20(3): 168-173.
- Rahimi-Bashar F, Abolhasani G, Manouchehrian N, Jiryaee N, Vahedian-Azimi A, et al. (2021) Incidence and risk factors of delirium in the intensive care unit: A prospective cohort. Biomed Res Int 2021: 6219678.
- Abazid RM, Al-Harbi SA, Allihimy AS, Aldrewesh DA, Alkuraydis SA, et al. (2021) Incidence of delirium in the critical care unit and risk factors in the Central Region, Saudi Arabia. Saudi Med J 42(4): 445-448.
- Peng C, Wang M, Geng Y, Ke J, Dong P, et al. (2022) Risk factors for postoperative delirium in ICU patients with severe illness based on systematic review and meta-analysis. Annals of palliative medicine 11(1): 309-320.
- Ma W, Zheng J, Xu S, Huo Z (2020) Incidence and risk factors of delirium in ICU patients. Int J Clin Exp Med 13: 1928-1934.
- Pandharipande P, Cotton BA, Shintani A, Thompson J, Pun BT, et al. (2008) Prevalence and risk factors for development of delirium in surgical and trauma intensive care unit patients. J Trauma 65(1): 34-41.
- Fortini A, Morettini A, Tavernese G, Facchini S, Tofani L, et al. (2014) Delirium in elderly patients hospitalized in internal medicine wards. Intern Emerg Med 9(4): 435-441.
- Zaal IJ, Devlin JW, Peelen LM, Slooter AJ (2015) A systematic review of risk factors for delirium in the ICU. Crit Care Med 43(1): 40-47.
- Tiwari AM, Zirpe KG, Khan AZ, Gurav SK, Deshmukh AM, et al. (2023) Incidence, subtypes, risk factors, and outcome of delirium: A prospective observational study from Indian intensive care unit. Indian J Crit Care Med 27(2): 111-118.
- Lin SM, Liu CY, Wang CH, Lin HC, Huang CD, et al. (2004) The impact of delirium on the survival of mechanically ventilated patients. Crit Care Med 32(11): 2254-2259.
- Morandi A, Brummel NE, Ely EW (2011) Sedation, delirium and mechanical ventilation: the 'ABCDE' approach. Curr Opin Crit Care 17(1): 43-49.
- Barr J, Fraser GL, Puntillo K, Ely EW, Gélinas C, et al. (2013) American college of critical care medicine. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 41(1): 263-306.






























