Summary
Introduction: Acute pulmonary edema is a common condition for which the management is an emergency. It is classic to distinguish two types of pulmonary edema: cardiogenic and lesional.
Objectives: To evaluate the management of acute pulmonary edema in the intensive care unit.
Methodology: We conducted a retrospective, descriptive and analytical study. It took place over a 12-month period from January 1st to December 31st, 2023.
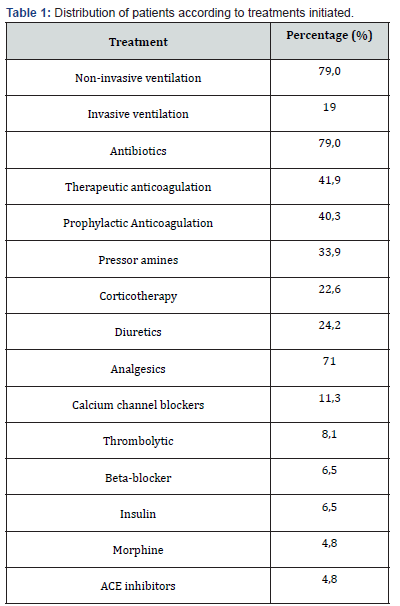
Results: We collected 62 patients during the study period, a frequency of 16%. The average age was 59.1 years with extremes of 20 and 99 years. The sex ratio was 1. Pulmonary edema was lesional in 74.4% and cardiogenic in 25.6% of patients. Pulmonary embolism found in 30.6% and pneumonia in 32.3% were the main etiologies of lesional pulmonary edema. Hypokinetic dilated cardiomyopathy found in 14.5% was the main etiology of cardiogenic pulmonary edema. Antibiotic therapy was administered in 79% of patients and corticosteroid therapy in 22% in the treatment of pulmonary oedema. More than half of the patients, 69%, received painkillers. Diuretics were administered in 24% of patients. Noradrenaline was administered in 16.13% and dobutamine in 11.3%. Non-invasive ventilation (NIV) was used in 73% of patients, high-flow oxygenation in 6% and invasive ventilation in 19%. We reported 69.4% of deaths secondary to pulmonary edema with injury.
Conclusion: The distinction between these two types of edemas is important, as it guides the treatment and can have an impact on the prognosis of patients.
Keywords:Acute Pulmonary Edema; Cardiogenic; Lesional; Resuscitation; Ziguinchor
Abbreviations: NIV: Non-Invasive Ventilation; CPE: Cardiogenic Pulmonary Edema; ARDS: Acute Respiratory Distress Syndrome
Introduction
Pulmonary oedema is defined as the pathological accumulation of fluid in the extravascular spaces and tissues of the lung. It is a frequent pathology whose management is an emergency. Severity can range from simple exertional dyspnea to major respiratory failure. It is classic to distinguish two types of pulmonary edema: cardiogenic and lesional. Although they lead in both cases to an alteration of amitosis, their therapeutic management differs due to different pathophysiological mechanisms. Cardiogenic pulmonary edema (CPE) is more common and secondary to an increase in hydrostatic pressure in the pulmonary capillaries often related to left heart failure. The lesional pulmonary oedema, of which acute respiratory distress syndrome (ARDS) is the most severe form, is in turn the consequence of a process combining direct aggression and inflammation leading to alveolo-capillary whose etiologies are numerous intra or extra-thoracic. The prognosis of cardiogenic edema is better than that of lesional edema despite the improvement in its management, particularly ventilatory [1-3].
The etiologies of ARDS are dominated in 59.4% of cases by pneumonia, especially with the Covid-19 pandemic. They are followed by extra-pulmonary sepsis in 16% of cases. ARD) represents 10 to 15% of the causes of admission to resuscitation [4]. It is responsible for 20 to 45% mortality [4]. At the same time, acute CPE corresponds to the occurrence of signs of life-threatening congestive heart failure. Acute heart failure can occur due to a de novo cardiac pathology or then decompensate for chronic heart failure requiring the search for precipitating factors [5]. CPE represents 5% of emergency room hospitalizations and mainly affects elderly patients with chronic heart disease. The hospital mortality related to pulmonary edema is estimated at 1% and amounts to 40% at 1 year [6,7]. In Senegal, few studies have been conducted on acute cardiogenic and lesional pulmonary edema. The deficiency of resuscitation data on these pathologies, whose recurrence is not evident in the Ziguinchor region, led us to initiate this study whose general objective is to review the management of pulmonary edema in the intensive care unit of the Ziguinchor Peace Hospital and the specific objectives are to specify the clinical and paraclinical epidemiological profile, to determine their impact, to evaluate their management and to give their evolutionary aspect.
Patients and Methodology
We conducted a retrospective, descriptive and analytical study on the management of pulmonary edema at the Peace Hospital Center in Ziguinchor. It took place over a 12-month period from January 1st to December 31st, 2023. We included all patients who presented with pulmonary edema at resuscitation confirmed by clinical and paraclinical elements. We were interested in the study of frequency, sociodemographic, clinical and paraclinical parameters, therapeutic management, and evolutionary parameters.
Results
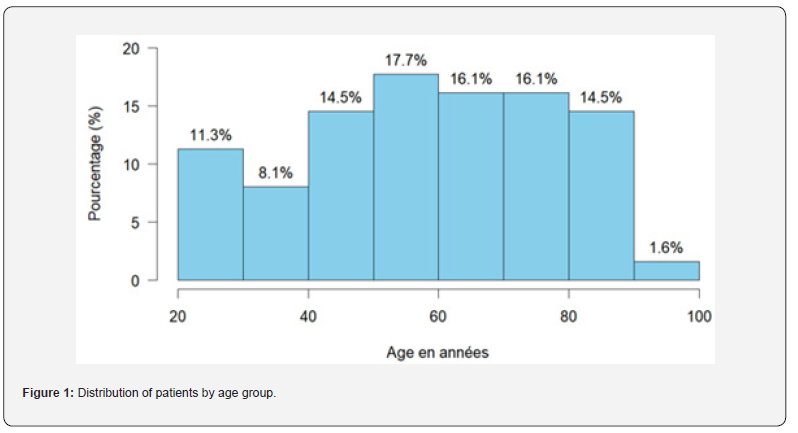
During our study period, we collected 62 patients out of 380 admitted to the resuscitation department of the Peace Hospital, which represents a frequency of 16%. The lesional pulmonary oedema was present in more than half of the patients, 74.4%, and 25.6% of the patients presented a CPE. The sex ratio was 1. The average age of patients was 59.1 years with a standard deviation of 19.1. The median age was 60 years with extremes of 20 and 99 years (Figure 1). More than half of the patients, or 58%, resided in Ziguinchor. A peak in admission was recorded in the month of October with 16.4%. Among the 62 patients in our study, 41.9% had a medical history. Hypertension was the main medical history followed by diabetes in respectively 31.1% and 12.9% as illustrated. Among hypertensive patients, 43.5% had no follow-up. Patients had an altered general condition in 46.8% of WHO stage III. The average oxygen saturation was 84 ± 9.3 with extremes of 45 and 95%. The majority of patients, 96.8%, had a desaturation at admission. The mean systolic blood pressure was 123 ± 34.4 with extremes of 63- and 210-mm Hg. More than half of the patients, 52.5%, had high blood pressure and 44.1% had low blood pressure. Most of the patients, or 83.1%, had tachypnea. More than half or 57.4% of the patients had tachycardia. Hyperthermia was found in 23.3% of patients. We found anemia in 30.5% of cases.
We found neutropenia in 5.1% of cases and hyperleukocytosis in 54.2% of cases. Thrombopenia was found in 15.3% of cases. CRP was positive (> 6) in 73.6% of patients. We found hyponatremia in 18.2% of patients and hypernatremia in 14.5%. The mean serum potassium level was 4.1 ± 0.9 with extremes of 2.4 and 6.6. Renal function was impaired in 39.3% of patients. The chest X-ray was performed in 37.1% of patients. Bilateral alveolar opacities with aerial bronchogram were found in 22.6% of patients. An opacity giving the butterfly wing pattern had been found in 17.7%. Pulmonary embolism in 30.6% and pneumonia in 32.3% were the main etiologies of lesional pulmonary edema. Among patients with pulmonary lesional edema, the mechanism was direct in 98%. Hypokinetic dilated cardiomyopathy in 14.5% was the main etiology of CPE. The management is described in the table below (Table 1). Noradrenaline was used in 16.13% followed by dobutamine in 11.3% and synergistically in 6.45%. The mortality in our series was 69.4%. All deaths had lesional pulmonary edema. The factors associated with mortality were poor general condition and poorly followed hypertension.
Discussion
In our study, the prevalence was 16%. This figure is relatively high, underscoring the importance of closely monitoring for pulmonary edema especially in patients with cardiac and respiratory risk factors. This could also be a reflection of the high severity threshold of patients in intensive care where pulmonary complications are common, as reported in the literature [3-8]. The average age of patients was 59.1 years. The most represented bracket was 50 to 99 years. The study by Muller and Bobbia [9] had found a similar age group regarding cardiogenic edema. The Rubenfeld study [10] had found more pulmonary edema in the age group between 55 and 85 years. The predominance of this age group may be related to the aging of the heart and vessels, the underlying comorbidity and cardiac pathologies but also the vulnerability of people at these ages. Our study revealed an equal distribution of men and women among patients with pulmonary edema, which contrasts with some previous studies showing a predominance of pulmonary edema in males, particularly for cardiogenic causes. This equality may suggest that, in our cohort, the risk factors associated with pulmonary edema are more homogeneously distributed between the genders, or that there are other factors influencing the incidence of this complication during resuscitation.
Nearly half or 41.9% had a medical history and hypertension was the main antecedent. This is a risk factor for the development of heart failure and CPE. This comorbidity is a key element in the pathophysiology of CPE [11,12]. Hypoxemia was found in 96.8%. The majority of our hypoxemic patients had oxygen saturation between 45 and 95%. The median was 88%. This reflects the severity of heart and respiratory failure in our cohort. Severe hypoxia is a classic sign of CPE where fluid accumulation in the lungs hinders gas exchange and leads to insufficient tissue oxygenation. Our results are in line with the literature which shows that hypoxia is often present and of poor prognosis [6]. The majority of patients (83.1%) had tachypnea. This is a common physiological response to respiratory disorders, particularly in critical situations. She often signs a compensatory response to hypoxia. As explained in the pathophysiology of lesional edema, the alveoli are damaged, which disrupts gas exchange and leads to hypoxia [12]. In response, the respiratory system increases the respiratory rate to try to maintain a sufficient level of oxygenation. In cardiogenic edema, the heart’s inability to pump blood efficiently leads to pulmonary congestion reducing the lungs’ ability to supply oxygen to the body [6]. The average heart rate was 108 ± 24.4 with extremes of 54 and 200 bpm. The median was 105 bpm. Tachycardia is a common phenomenon in stressful contexts, such as in intensive care.
Here the patients face intense physiological stress, whether cardiac, respiratory or systemic. This stress induces an activation of the sympathetic nervous system, which increases the heart rate to try to maintain sufficient cardiac output in order to ensure the perfusion of vital organs, notably the heart, lungs and brain. The results revealed neutropenia in 5.1% of cases and leukocytosis in 54.2% of cases. In our study, hyperleukocytosis could be explained by a higher frequency of lesional pulmonary edema which are generally secondary to an infection. The CRP was positive (> 6) in 73.6% of cases. In the injured pulmonary edema, CRP is positive in relation to the inflammation occurring on the occasion of infectious or inflammatory etiologies. Jouanet’s work has demonstrated the involvement of inflammation in severe pneumonia [13]. The chest X-ray plays a crucial role in positive, etiological and differential diagnosis, as well as in the assessment of associated complications. The recent study by Simon [14] confirmed this assertion. In our study, 37.1% of patients underwent a chest X-ray. The lack of pulmonary imaging in most of our patients could be explained by the lack of a radiographic device in our structure throughout our study. Our study found more patients with edema (74.4%) than cardiogenic, unlike that of Goldstein [6] where they observed a lower incidence of ARDS compared to CPE. Similarly, there is a tendency to report a higher prevalence of CPE in hospitalized populations, particularly in intensive care.
This difference can be explained by the increased incidence of pneumonia, which constitute the main etiologies of lesional pulmonary oedema. The predominance of direct causes of lesional edema observed in our study can be explained by several factors. First, the central role of care-associated infections in causing acute lung injury in current resuscitation units largely contributes to the increase in lesional edema. In addition, severe sepsis responsible for a systemic inflammatory cascade can also lead to direct degradation of the alveolo-capillary membrane, thereby increasing fluid accumulation in interstitial spaces. Finally, physical traumas especially thoracic often present in polytraumatized patients can also cause direct injury to the vascular wall and epithelium, promoting fluid leakage. The study by Ware and Lorraine [15] demonstrated that the majority of causes of ARDS were indirect and this was even correlated with mortality. Corticosteroid therapy was administered in 22% of our patients due to an exacerbated inflammatory component or underlying pulmonary comorbidity. Although corticosteroid therapy is less commonly used in CPE, its effectiveness in lesional pulmonary edema is more than proven [6,16]. Meduri showed that the level of procollagen peptide types 1 and 3 was increased in the bronchoalveolar lavage and in the plasma of patients with ARDS and that corticoids allowed reducing the level of these markers [17]. More than a third, or 69%, of our patients received analgesics, hence the importance of pain management in intensive care, especially in the context of respiratory distress, heart failure, or trauma.
In intensive care, analgesics are administered to improve the patient’s comfort and prevent pain from increasing intrathoracic pressure and further compromising respiratory function. The percentage of patients on diuretics (24%) might seem relatively low, given that diuretics are a first-line treatment for cardiogenic pulmonary edema, particularly in cases of heart failure. Many of our patients had pulmonary edema, which is why we note a low use of diuretics. Noradrenaline was used in 16.13% followed by dobutamine in 11.3% and synergistically in 6.45%. These results could be explained by the fact that dobutamine is used in the treatment of cardiogenic shock where there is often a myocardial dysfunction but also noradrenaline in case of septic shock in injured pulmonary edema. The percentage of patients who received both simultaneously suggests cases where patients had complex heart failure requiring both hemodynamic and inotropic support. The more frequent use of non-invasive ventilation (NIV) (73%) could indicate that the practitioners of our study institution prefer this approach as a first line, in the absence of contraindications such as impairment of consciousness. NIV, being less invasive, would allow better tolerance in some patients and would be associated with a lower risk of complication than invasive ventilation. Failure of NIV, manifested as worsening hypoxia or persistent hypercapnia, could explain the need for invasive ventilation in 19% of patients. A study by Cockral [18] showed that NIV reduces the use of intubation and mortality in patients with CPE. Fernando [19] demonstrated that mechanical ventilation combined with a pulmonary protection strategy is best advised in severe ARDS.
Non-invasive ventilation may be considered in patients with mild ARDS, but will likely be of limited use in more severe cases. Non-invasive assistance strategies can be proposed to avoid intubation, but subject to the absence of excessive inspiratory effort, the high-flow oxygen therapy technique is increasingly used in resuscitation because it offers comfort, rapid relief of shortness of breath and improved oxygenation during hypoxemic acute respiratory failure. Studies currently underway continue to prove its effectiveness in reducing the use of intubation and mechanical ventilation [20]. In our study, 69.4% of patients succumbed to their pathology, while 29% were transferred to other services for further management. The totality of mortality due to the lesional pulmonary edema. A study conducted in the United States by Bernard [21] found a percentage of deaths around 90%. Unlike in Belgium, Tilman [22] found mortality among 30% of patients. These data highlight the severity of the pathology and the generally unfavorable clinical outcome of patients with pulmonary edema, especially lesion. Pulmonary edema, particularly in al, can be rapidly fatal, especially if early management is not optimal or if there are numerous comorbidities. CPE, although often reversible if properly managed, can also lead to fatal outcome in cases of severe cardiac decompensation, especially in elderly patients or those with comorbidities such as high blood pressure, atherosclerosis or rhythm disorders.
Conclusion
The results of this study highlighted the importance of a rigorous clinical evaluation and rapid management adapted according to the etiologies. The distinction between these two types of edemas is important, as it guides treatment and can have an impact on the prognosis of patients. This work opens the way for future research, particularly to better understand the complex interactions between cardiac and pulmonary mechanisms.
References
- Perrot S, Sztrymf B, Ricard JD (2009) Pulmonary edema. EMC - Pneumology 6(4): 1‑
- Garnier M (2024) Acute respiratory distress syndrome. EMC - Anesthesia-Resuscitation 44(4): 1‑
- Bellani G, Laffey JG, Pham T, Fan E, Brochard L, et al. (2016) Epidemiology, Patterns of Care, and Mortality for Patients with Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries. JAMA 315(8): 788‑
- Fernando SM, Ferreyro BL, Urner M, Munshi L, Fan E, et al. (2021) Diagnosis and treatment of acute respiratory distress syndrome. CMAJ 193(21): E761-E768.
- (2021) College of Emergency Medicine and Resuscitation.
- Goldstein A, Antoine A, Ray P (2021) SAU and diagnosis of cardiogenic pulmonary edema. Care Gerontology 26(151): 24‑2
- Beuret P (2014) Management of the patient in acute respiratory failure. Arnette John Libbey Euro text, pp. 188.
- Wright JR (2005) Immunoregulatory functions of surfactant proteins. Nat Rev Immunol 5(1): 58‑
- Muller L, Bobbia X (2022) Modern management of acute cardiogenic pulmonary edema. Anesthesia & Resuscitation 8(2): 163‑1
- Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, et al. (2005) Incidence and Outcomes of Acute Lung Injury. New England Journal of Medicine 353(16): 1685‑16
- Netter F (2019) Thorax: surface anatomy. Atlas.
- Offenstadt G (2016) Resuscitation: the essentials in intensive care, resuscitation. Issy-les-Moulineaux: Elsevier-Masson.
- Jouan Y, Si-Tahar M, Paget C (2019) Severe pneumonia and acute respiratory distress syndrome: involvement of unconventional T cells. Rev Mal Respir 36(4): 451‑45
- Simon A, Redheuil A, Khafagy P, Boussouar S (2024) Imaging of pulmonary edema. EMC - Radiology and medical imaging - Cardiovascular-Thoracic-Cervical 42(4): 1‑
- Ware LB, Matthay MA (2000) The Acute Respiratory Distress Syndrome. New England Journal of Medicine 342(18): 1334-1349.
- Georges O (2016) Resuscitation the Reference Treaty in Intensive Medicine - Resuscitation.
- Umberto Meduri G, Tolley EA, Chinn A, Stentz F, Postlethwaite A, et al. (1998) Procollagen Types I and III Aminoterminal Propeptide Levels during Acute Respiratory Distress Syndrome and in Response to Methylprednisolone Treatment. Am J Respir Crit Care Med 158(5): 1432‑14
- Masip J, Roque M, Sánchez B, Fernández R, Subirana M, et al. (2005) Noninvasive Ventilation in Acute Cardiogenic Pulmonary Edema Systematic Review and Meta-analysis. JAMA 294(24): 3124-3130.
- Fernando SM, Ferreyro BL, Urner M, Munshi L, Fan E, et al. (2021) Diagnosis and treatment of acute respiratory distress syndrome. CMAJ 193(21): E761-E768.
- Iteke FR, Somwa ML, Rhulinamungu MF, Mulunda MB (2025) Oxygen therapy with Opti flow as a barrier to mechanical ventilation in the management of Covid-19: experience at the Diamond Medical Center in Lubumbashi. African Journal of Medicine and Public Health 4(2).
- Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, et al. (1994) The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 149(3 Pt 1): 818-824.
- Tilman S (2018) Severe heart failure and acute pulmonary edema. Rev Med Liege.






























