- Research Article
- Abstract
- Introduction
- Materials and Methods
- Variables of the Study
- Operational Definitions
- Data Collection Tool and Procedures
- Data Quality Assurance
- Data Analysis and Management
- Ethics Approval and Consent to Participate
- Results
- Discussion
- Strength of the Study
- Limitations of the Study
- Conclusions
- Acknowledgements
- References
Incidence and Risk Factors of Post-Dural Puncture Headache Among Adult Non-Obstetric Patients after Spinal Anesthesia at Comprehensive Hospitals of South Nations Nationalities and Peoples Region of Ethiopia: A Modified Poisson Regression
Selman Reshad Amino*1, Amene Abebe2, Nefsu Awoke3, Wogayehu Abera4, Abdulkadir Kedir4, Nesredin Shemsu4, Temesgen Mamo1 and Sintayehu Samuel1
1Department of anesthesia, College of Medicine and Health Science, Wachemo University Hosaena, Ethiopia
2School of Public Health, College of Health Science and Medicine, Wolaita Sodo University, Ethiopia
3School of Adult Health Nursing, College of Health Science and Medicine, Wolaita Sodo University, Ethiopia
4School of anesthesia, College of Health Science and Medicine, Wolaita Sodo University, Wolaita Sodo, Ethiopia
Submission: March 27, 2024; Published: May 23, 2024
*Corresponding author: Selman Reshad, Department of anesthesia, College of Medicine and Health Science, Wachemo University Hosaena Ethiopia
How to cite this article: Selman Reshad A, Amene A, Nefsu A, Wogayehu A, Abdulkadir K, et al. Incidence and Risk Factors of Post-Dural Puncture Headache Among Adult Non-Obstetric Patients after Spinal Anesthesia at Comprehensive Hospitals of South Nations Nationalities and Peoples Region of Ethiopia: A Modified Poisson Regression. J Anest & Inten care med. 2024; 13(4): 555869.DOI 10.19080/JAICM.2024.13.555869
- Research Article
- Abstract
- Introduction
- Materials and Methods
- Variables of the Study
- Operational Definitions
- Data Collection Tool and Procedures
- Data Quality Assurance
- Data Analysis and Management
- Ethics Approval and Consent to Participate
- Results
- Discussion
- Strength of the Study
- Limitations of the Study
- Conclusions
- Acknowledgements
- References
Abstract
Introduction: Post-dural puncture headache is one of the incapacitating problems which may delay recovery, and timely discharge of patients, increase patient suffer and healthcare expense. In Ethiopia most of the earlier research are cantered on obstetric patients. Hence, this study aimed to assess the incidence as well as risk factors of post-dural puncture headaches among adult non-obstetric patients.
Methods: A prospective observational study was carried out on 340 adult non-obstetric patients using a consecutive sampling method. Data was collected using an observation checklist and a structured questionnaire. Epidata version 4.6 was used to enter the data and then exported to SPSS 26.0 for analysis. Tables, graphics, and textual narrations were used to present the study’s findings. Model fitness was checked by finite sample corrected Akaike Information Criterion (AICC). The relative risk and 95% confidence intervals were computed. A bi-variable and multivariable modified Poisson regression analysis was computed, and the level of statistical significance was declared at p-value<0.05.
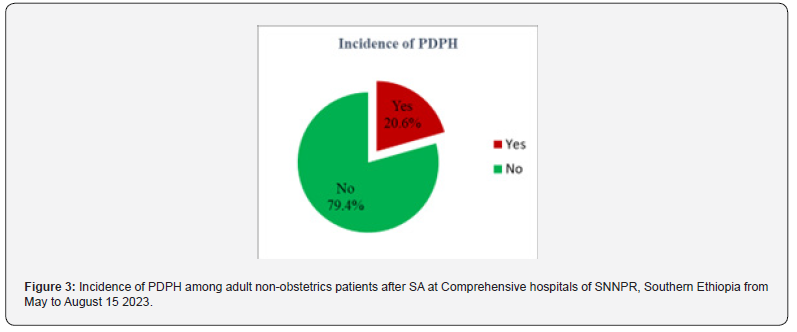
Results: The incidence of post-dural puncture headache in this study was found to be 20.6% (95%CI: 16, 25%). Young age ARR=3.78; (95%CI: 1.199, 11.897), female sex, ARR = 1.66; (95%CI: 1.114, 2.488), spinal anesthesia administered by students under supervision of professionals ARR=1.536(95%CI: 1.030,2.288), large needle ARR = 1.623 (95% CI: 1.107,2.381), perpendicular needle bevel orientation ARR =2.43, (95% CI: 1.551,3.818), and multiple attempts ARR=2.08, (95% CI: 1.256,3.448) were found to be significant risk factors of PDPH.
Conclusions: In this study, the incidence of PDPH among adult non-obstetric patients comparable the results of similar studies. Post-dural puncture headache was significantly higher in young patients, perpendicular needle bevel orientation, and multiple dural puncture attempts.
Key words: Incidence; Non-Obstetric Patients; Post-Dural Puncture Headache; Spinal Anesthesia; Risk Factors
Abbreviations: ARR: Adjusted Relative Risk; ASA: American Society of Anaesthesiologists; BMI: Body Mass Index; CI: Confidence Interval; CSF: Cerebrospinal Fluid; NEMMCSH: Nigist Eleni Mohammed Memorial Comprehensive Specialized Hospital; PDPH: Post Dural Puncture Headache; SA: Spinal Anesthesia; SNNPR: South Nations Nationalities and Peoples’ Region; WCSH: Worabe Comprehensive Specialized Hospital; WSUCSH: Wolaita Sodo University Comprehensive Specialized Hospital
- Research Article
- Abstract
- Introduction
- Materials and Methods
- Variables of the Study
- Operational Definitions
- Data Collection Tool and Procedures
- Data Quality Assurance
- Data Analysis and Management
- Ethics Approval and Consent to Participate
- Results
- Discussion
- Strength of the Study
- Limitations of the Study
- Conclusions
- Acknowledgements
- References
Introduction
The International Classification of Headache Disorders (ICHD-III) defined Post Dural Puncture Headache (PDPH) as a bifrontal and/or occipital headache that develops within five days after Lumber Puncture, gets better or disappears while lying down, and gets worse or arises when an upright position is adopted. Together with the positional headache, PDPH may be accompanied by nausea, vomiting, neck stiffness, dizziness, photophobia, tinnitus, and diplopia [1]. Spinal Anesthesia (SA) or unintentional dural puncture while administering epidural anesthesia, which results in a loss of Cerebrospinal Fluid (CSF) to the epidural space through the dural hole and a drop in CSF pressure, low intracranial CSF volume or intracranial hypotension may ensue which deemed to play a pivotal role for the pathophysiology of PDPH [2].
There is a wide variation on the incidence of PDPH. A review of literatures by Jabbari A., et al., reported the incidence of PDPH within the range of 0.1-36% in the general population, including both obstetric and non-obstetric patients, after SA [3]. The variation on the incidence of PDPH is due to non-modifiable and modifiable factors. Feminine gender, youth, gestation, past headaches, low CSF opening pressure, and low Body Mass Index (BMI) are characteristics that put patients at risk for developing PDPH [4]. Given that evidence from studies shows that PDPH incidence is also affected by needle size, needle type, and needle bevel orientation [5]. In addition, from review of different literature PDPH incidence is also affected by; patient position during SA administration, approach to SA, experience of anesthesia provider, and number of dural puncture attempts [6,7]. However, there are inconsistencies between findings of studies for some of mentioned risk factors of PDPH [8-10]. The presence of PDPH can be extremely uncomfortable to the patient, making it difficult to move around, and potentially lengthening hospital stays and raising medical expenses in addition diminishing the capacity patient to carry out daily tasks. Therefore, it’s critical to prioritise PDPH prevention and the best possible care due to its serious implications [11].
There is a wealth of information available regarding the occurrence, treatment, and prevention of PDPH in pregnant patients after SA and unintentional dural puncture during epidural analgesia. Little information is available regarding dural puncture in patients who are not obstetrics [12,13]. Even though PDPH incidence is common among non-obstetric patients under SA secondary to different risk factors, there is no adequate study regarding the PDPH incidence among non-obstetric patients in Ethiopia. There are also inconsistencies on the factors of PDPH among studies. In addition, most of the previous studies used odds ratio which is obtained from logistic regression model to show the effect of risk factors on PDPH, however; odds ratio is overestimates the effect of risk factors as risk ratio when the outcome is common (>10%). Therefore, this study used a modified Poisson regression model to directly estimate risk ratio both reliably and effectively [14-16]. Thus, the purpose of the current study to evaluate the incidence as well as risk factors of PDPH among adult nonobstetric patients.
- Research Article
- Abstract
- Introduction
- Materials and Methods
- Variables of the Study
- Operational Definitions
- Data Collection Tool and Procedures
- Data Quality Assurance
- Data Analysis and Management
- Ethics Approval and Consent to Participate
- Results
- Discussion
- Strength of the Study
- Limitations of the Study
- Conclusions
- Acknowledgements
- References
Materials and Methods
Study Design, Period and Setting
Prospective cohort study design employed at comprehensive hospitals of South Nations Nationalities and Peoples Region of Ethiopia from May 15 to August 15. There are a total of three comprehensive hospitals in the South Nations, Nationalities and Region of Ethiopia. Namely, Wolaita Sodo University Comprehensive Specialized Hospital, Worabe Comprehensive Specialized Hospital, and Nigist Eleni Mohammed Memorial Comprehensive Specialized Hospital were included in this study. All the three hospitals were included in the study.
Population
All adult non-obstetric patients undergoing surgery at the three comprehensive hospitals were the source population of the study. All adult non-obstetric patients undergoing surgery under SA and fulfil inclusion criteria were included in this study. Patients with chronic headache, history of PDPH, SA converted to general anesthesia, and once the patient is selected and comes for the next operation under SA.
Sample Size Determination and Sampling Procedure
The sample size was determined by taking the following assumption: the prevalence of PDPH is 33% (17), the confidence interval is 95%, and the margin of error is 0.05. The sample size was determined using the following single population proportion formula by the assumption of homogeneity of the population to study variables in the selected hospitals.
To get the sample size with a confidence interval of 95% and a margin of error of 5%

Where n=sample size, Z=Z statistics for 95% level of confidence (1.96), P= incidence of outcome (0.33), and d=margin of sampling error to be tolerated (0.05).
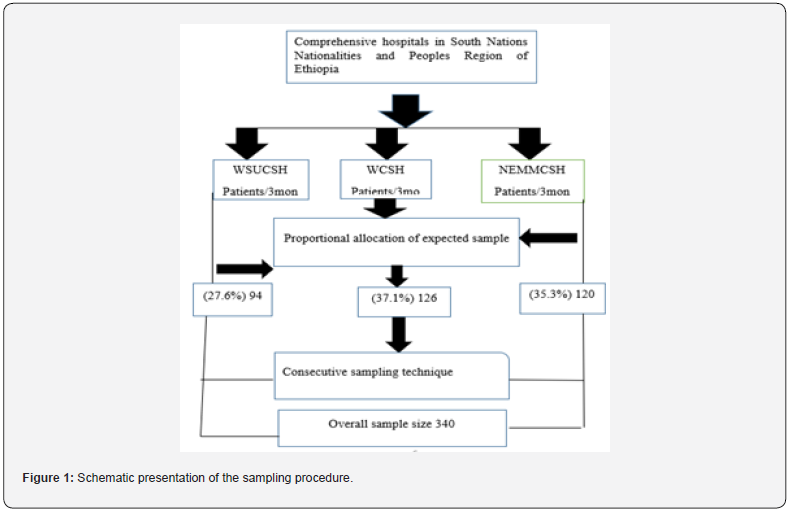
All three hospitals namely, WSUCSH, WCSH, and NEMMCSH were included in this study. From the situational analysis of postoperative surgical patient logbook of these hospitals, 700 patients were operated under SA within 3 months (May 1, 2022-August 1, 2022). Then patients who underwent operation under SA were proportionally allocated for each Comprehensive Hospital in SNNPR. From the logbook record in 3 months, operations done under SA in each hospital were WSUCSH=193, WCSH=260, and NEMMCSH=247. Then study participants were selected using consecutive sampling technique with the assumption that each study participant was randomly admitted to hospital and scheduled for surgical operation (Figure 1).
- Research Article
- Abstract
- Introduction
- Materials and Methods
- Variables of the Study
- Operational Definitions
- Data Collection Tool and Procedures
- Data Quality Assurance
- Data Analysis and Management
- Ethics Approval and Consent to Participate
- Results
- Discussion
- Strength of the Study
- Limitations of the Study
- Conclusions
- Acknowledgements
- References
Variables of the Study
Dependent Variable
Post-Dural Puncture Headache (Yes/No).
Independent Variables
Patient-Related Variables: Age, sex, Body Mass Index (BMI), American Society of Anesthesiologist (ASA) physical status of the patient.
Anesthesia Provider and Spinal Needle Related Factors: Position of the patient while administering SA, type of spinal needle, size of the spinal needle, orientation of the needle bevel to the long axis of the spine, approach of spinal anaesthesia, number of attempts during puncture, type of operator of the anaesthesia, and work experience of an operator.
- Research Article
- Abstract
- Introduction
- Materials and Methods
- Variables of the Study
- Operational Definitions
- Data Collection Tool and Procedures
- Data Quality Assurance
- Data Analysis and Management
- Ethics Approval and Consent to Participate
- Results
- Discussion
- Strength of the Study
- Limitations of the Study
- Conclusions
- Acknowledgements
- References
Operational Definitions
PDPH: PDPH is characterized by a headache that gets worse in an upright position and becomes better in the supine position. To diagnose the headache as PDPH, a postural component had to be present [17,18]. The severity of PDPH pain was evaluated by using a Visual Analog Scale (VAS) score. PDPH can be mild if VAS evaluations of 6 to 44 mm, VAS ratings of 45 to 69 mm are diagnosed as Moderate PDPH, and VAS ratings ≥70 mm as suggestive of severe PDPH pain [19].
Approach of spinal aesthesia: It is a needle insertion technique relative to the spinous process, which can be a median or paramedian [20].
Needle size: large needle 18-22Gauge, and small needle 23-25Guage.
Neck stiffness: refers to restriction neck’s range of motion or function.
Photophobia: discomfort in the eyes experienced because of being subjected to bright light [21].
Tinnitus: a feeling that either or both ears are sounding, hissing, or yelling.
Vomiting: food particles that have not yet been digested move through the mouth [22].
- Research Article
- Abstract
- Introduction
- Materials and Methods
- Variables of the Study
- Operational Definitions
- Data Collection Tool and Procedures
- Data Quality Assurance
- Data Analysis and Management
- Ethics Approval and Consent to Participate
- Results
- Discussion
- Strength of the Study
- Limitations of the Study
- Conclusions
- Acknowledgements
- References
Data Collection Tool and Procedures
An observation checklist and questionnaire adopted from previous studies was used, which is prepared in the English language [23,24]. Data was collected by three-degree holder anaesthetists and supervised by three MSc holder anaesthetists. The patient-related information was obtained from secondary data using medical documents or primary data from history by the data collector. Intraoperatively using checklist data about the patient’s position during SA, approach, number of attempts, the operator, needle type, and size direction of needle bevel were documented by data collectors. Postoperatively all patients were followed until they reported PDPH within 3 days. Those who reported PDPH before 3 days were not followed the report. And those who did not report PDPH until 3 days were declared free of PDPH. The first visit was done between the first 12 and 24 hours of the postoperative period; the next visit was in the 48th hour, and the last visit was in the 72nd hour. In patients who develop headaches within 3 days of post-operation, they were assessed for their positional influence. The severity of PDPH pain was assessed using visual analogue scale.
- Research Article
- Abstract
- Introduction
- Materials and Methods
- Variables of the Study
- Operational Definitions
- Data Collection Tool and Procedures
- Data Quality Assurance
- Data Analysis and Management
- Ethics Approval and Consent to Participate
- Results
- Discussion
- Strength of the Study
- Limitations of the Study
- Conclusions
- Acknowledgements
- References
Data Quality Assurance
An observation checklist and questionnaire were adopted from previous studies which were prepared in the English language. Before the actual data collection two-day training was given to data collectors and supervisors regarding the objective of the study, obtaining informed consent and how to approach the patient. During data collection regular supervision was conducted to check the completeness and consistency of data. Before data analysis data cleaning and crosschecking for missing data was done.
- Research Article
- Abstract
- Introduction
- Materials and Methods
- Variables of the Study
- Operational Definitions
- Data Collection Tool and Procedures
- Data Quality Assurance
- Data Analysis and Management
- Ethics Approval and Consent to Participate
- Results
- Discussion
- Strength of the Study
- Limitations of the Study
- Conclusions
- Acknowledgements
- References
Data Analysis and Management
Data was entered into Epi data 4.6 and then exported to SPSS version 26.0 for analysis. Summary measures such as mean, frequency distribution, percent, and standard deviations were computed. The multi-collinearity of the independent variables was checked by a variance inflation factor (VIF) <10 for all independent variables. Bi-variable and multivariable modified Poisson regression analysis was done at P-value < 0.25 and P-value < 0.05 respectively to identify independent predictors of PDPH. The model fitness was checked by finite sample corrected Akaike Information Criterion (AICc). The incidence of PDPH and risk factors strength of associations was presented using an adjusted relative risk (ARR) with its 95% CI. Finally, variables with p-value < 0.05 in the multivariable modified Poisson regression model were declared as statistically significant association with the dependant variable. Tables, graphics, and textual narrations were used to present the study’s findings.
- Research Article
- Abstract
- Introduction
- Materials and Methods
- Variables of the Study
- Operational Definitions
- Data Collection Tool and Procedures
- Data Quality Assurance
- Data Analysis and Management
- Ethics Approval and Consent to Participate
- Results
- Discussion
- Strength of the Study
- Limitations of the Study
- Conclusions
- Acknowledgements
- References
Ethics Approval and Consent to Participate
Ethical approval for this study was obtained from the ethical review board of Wolaita Sodo University, College of Health Sciences and Medicine. Permission was obtained from the hospitals to conduct the study. The purpose and objective of the study were explained to the patients and informed consent was taken from every study participant before the start of data collection. The obtained data was used only for study purposes. Confidentiality and anonymity were ensured.
- Research Article
- Abstract
- Introduction
- Materials and Methods
- Variables of the Study
- Operational Definitions
- Data Collection Tool and Procedures
- Data Quality Assurance
- Data Analysis and Management
- Ethics Approval and Consent to Participate
- Results
- Discussion
- Strength of the Study
- Limitations of the Study
- Conclusions
- Acknowledgements
- References
Results
Socio-Demographic and Preoperative Characteristics of Patients
A total of 340 non-obstetric patients who fulfilled inclusion criteria and had volunteered by giving consent participated in the study making a response rate of 100%. The majority 220 (64.7%) of the study participants were males. The mean age of the study participants was 45.64, with a standard deviation of 16.48, and 135 (39.7%) of the participants were in the age range of (41-60 years). A higher proportion 229 (67.4%) of them were ASA I. Regarding BMI, the mean BMI of the study participants was 21.22, with a standard deviation of 2.17, and a very high proportion of 304(89.4%) of the participants were with normal BMI (18/.5- 24.9) range. (Table 1).

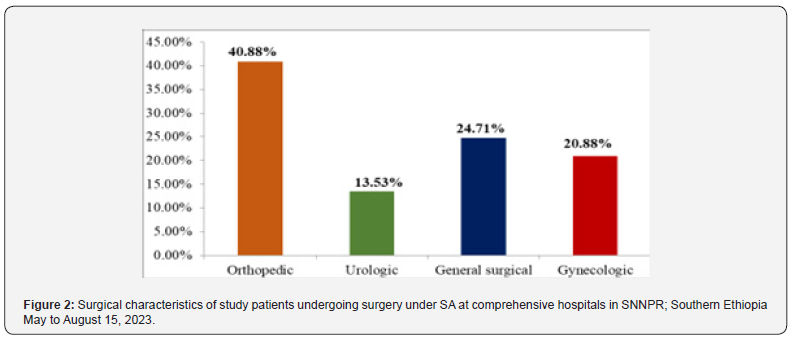
Type of surgery
It was observed from the data that among all non-obstetric surgical patient’s majority 139(40.88%) were orthopaedic patients, followed by general surgical 84(24.71%), gynaecologic 71(20.88%), and urologic 46(13.53%) (Figure 2).
Spinal Anesthesia-Related Parameters of Study Subjects
Out of three hundred and forty patients who received SA, 326 (95.9%) were in a sitting position while only 14 (4.1%) were in a lateral position. Most SA was given by anesthesia professionals 221(65%). The mean experience year for anesthesia professionals was 2.63±1.39 experience, with a minimum of one year and a maximum of nine years. The majority 269(79.1%) of the anesthetists preferred the midline approach for administering SA. The cutting type of needle is the only spinal needle type used to administer SA to study subjects. The 23G spinal needle was the most used 137 (40.29%) and the 21G was the least used spinal needle size 12(3.53%) for administering SA to these patients. The parallel needle orientation to the long axis of the dural fiber was more preferred 184(54.1%) than the perpendicular one. Most of the successful dural puncture was achieved by the second attempt 147(43.2%) (Table 2).

Incidence of PDPH
The overall incidence of PDPH in this study was 20.6% (95% CI= 16, 25) (Figure 3).
From the study participants who developed PDPH; 48.6% was detected in the 1st 24 hours (Table 3).
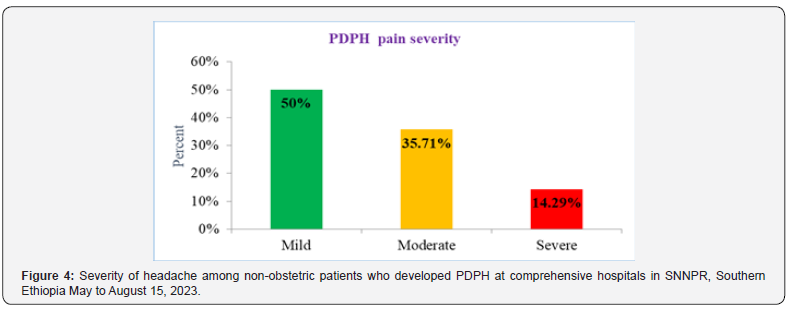
Among seventy patients who developed PDPH, most of them developed mild PDP pain 35 (50.00%) (Figure 4).
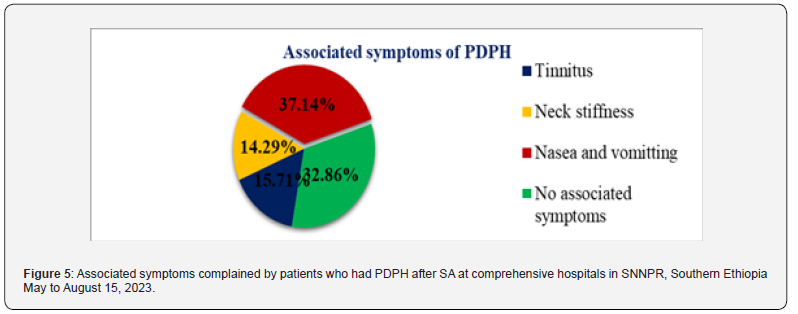
On 67.94% of patients with PDPH nausea and vomiting, neck stiffness, or tinnitus was observed (Figure 5).

Risk factors of PDPH
In the multivariable modified Poisson regression model, controlling for the possible confounder; variables namely age, sex, the anesthesia provider, needle size, needle bevel orientation, and the number of dural puncture attempts become significantly independent predictors of PDPH with a p-value <0.05. According to the result of our study, the occurrence of PDPH was 3.8 times higher in age groups of 20-40 years than those with the age of ≥ 60 years ARR=3.78; (95%CI: 1.199, 11.897). The patient’s sex was also strongly related to the development of PDP. Patients who were females had a 66% greater risk of developing PDPH than patients who were males ARR = 1.66; (95%CI: 1.114, 2.488). This study’s findings showed that SA performed using a large needle size (small gauge) increased the likelihood of PDPH by 62% ARR = 1.62 (95% CI: 1.107-2.381). Similarly, SA done with a cephalic needle direction increased the risk of PDPH by 2.4 times ARR = 2.43, (95% CI: 1.551-3.818). When SA was carried out by BSc students under supervision, the incidence of PDPH was increased by 54% than patients who underwent SA by anesthesia professionals ARR=1.54(95%CI: 1.030, 2.288). The risk of developing PDPH was higher 2.0 folds for those who received SA on subsequent try compared to individuals who underwent a single attempt ARR=2.08, (95% CI: 1.256, 3.448) (Table 4).

- Research Article
- Abstract
- Introduction
- Materials and Methods
- Variables of the Study
- Operational Definitions
- Data Collection Tool and Procedures
- Data Quality Assurance
- Data Analysis and Management
- Ethics Approval and Consent to Participate
- Results
- Discussion
- Strength of the Study
- Limitations of the Study
- Conclusions
- Acknowledgements
- References
Discussion
In this study, out of 340 study participants, 70(20.6%; 95% CI: 16, 25) of them developed PDPH. Out of those who developed PDPH, slightly lower than half 34 (48.6%) of them reported PDPH within the first 24 hours after SA, and half 35 (50%) of them complained of mild levels of PDPH. Post-dural puncture headache risk was higher among patients; between the ages of 20 and 40, females, who received SA by BSc anesthesia students under supervision, who received SA by a large needle size and in perpendicular needle bevel direction, and SA succeeded after multiple attempts, according to the secondary outcomes of this study. The occurrence of such a problem has been assessed to be highly varied, according to various literatures. According to review papers by Jabbari A., et al., the incidence of PDPH following an intentional dural puncture ranges from 0.1% to 36%, which includes the findings of the present study. Comparable findings were reported; a study investigated by M D. Schmittner et al. in Germany found 18% of PDPH cases among anorectal surgery patients and a study conducted by Roheena Wadood and Abbas Tariq in Pakistan revealed 22% PDPH incidence among urologic patients [25].
However, the incidence in this study was much higher when compared to the findings of studies conducted in different countries. In the USA the report indicates 2-3.4%, in Brazil (7.5%), in India (9.5%), and in Turkey (6%) [26-29]. The possible reason for the above discrepancies could be patients in earlier studies underwent SA utilizing cutting and pencil-pointed spinal needles, as well as small-size spinal needles exclusively; however, in this study, patients only received SA by cutting kind of spinal needles, as well as either small spinal needles or large spinal needles. Because it is thought that pencil point needles cause a tiny incision and then pull fibres apart to let the shaft pass through [30]. Assuming the tissues are elastic and do not tear while being stretched, they should return when the needle is removed, creating a smaller hole than a needle of the same size with a cutting bevel [31]. Another study done by Tafesse D in Black Lion Comprehensive Specialized Hospital, Addis Ababa Ethiopia reported 33% PDPH incidence which is higher than the result of this study.
The probable cause for this difference could be the use of a large needle size of 100% (22G) in their study since a large needle size increases the risk of PDPH [32]. However, in this study, 76.75% of the needles used ranged from 23 to 25G. According to this study’s finding, the age group of 20 to 40-year-olds has a PDPH development rate that is approximately 3.8 times higher than those over 60 years old ARR=3.78; (95%CI: 1.199, 11.897). The risk of developing a PDPH was nearly three times higher in the 40 to 60-year-old age group than it was in the > 60-year-old age group. The decreased dura mater elasticity, it more difficult for CSF to leak through the puncture opening, a smaller response of the cerebral vessels to CSF hypotension, and a smaller vertebral extradural space, allow just a little CSF collection, thereby stopping the flow of CSF from the subarachnoid space as its protective mechanism in elders [33]. This is in line with a study conducted in the USA [34]. Similarly, other studies in India and Turkey reported a higher incidence of PDPH in younger patients compared to their counterparts.
This study revealed that being female increases one’s risk of developing PDPH. Patients who were female had a 72% greater risk of developing PDPH than patients who were males ARR = 1.72; (95%CI: 1.164, 2.534). This is because women exhibit more responsiveness to painful stimuli than males do, which appears to indicate a difference in how they interpret nociceptive information, perhaps facilitating the central sensitization process [35]. Different investigations came to the same conclusion about this like studies conducted in Brazil, India, Pakistan, and in Northern Ethiopia (Gondar) [36]. Unlike this, a study conducted by Dagmar Oberhofer et al. in Croatia revealed that the incidence of PDPH has no relationship to the female gender, in younger orthopaedic patients. The possible discrepancy may be due to the age difference between groups. It was observed from the result of the present study that PDPH was increased by 54%, when SA was administered by BSc students under supervision, then patients who underwent SA by professional anesthetists ARR=1.54(95%CI: 1.030, 2.288).
This agrees with the findings of a study conducted by Y.A. Ferede, Y.A. Nigatu, and A.F. Age nehu et al. in Northern Ethiopia (Gondar), and in line with another study conducted in Turkey. However, it contradicts the findings of research demonstrated by W.I. Chaudhry et al. in Pakistan reported the absence of a significant association between clinician experience and PDPH incidence [37]. The potential cause of the discrepancies could be related to the varying levels of training. This study tried to compare BSc anesthesia students under the supervision of anesthesia professionals, but their study compared postgraduate anesthesiologist residents at different levels with senior consultants.
In this study, the use of large spinal needles has been shown to increase the chance of developing PDPH by 62% compared to smaller counterparts ARR = 1.62 (95% CI: 1.107, 2.381). The possible explanation for this discrepancy is due to larger openings on the Dura created by the larger needles, which results in increased CSF leakage than smaller openings brought on by smaller needles. Studies from the past conducted by Kassa et al., in Gondar (Northern Ethiopia), and by J. Salzer et al., in Sweden provided evidence for this finding. The uniformity may be explained by the fact that larger needles with wider holes in the dura caused more CSF leaking than smaller needles with smaller holes did, and a longer time required to repair. However, a study demonstrated by M D. Schmittner et al. in Germany found an absence of statistically meaningful difference between 25 G and 29 G needles. The logic behind this difference is more likely due to the difference age of patients.
The present study also demonstrated that PDPH incidence was increased approximately 2.4 times, ARR = 2.43, (95% CI: 1.551, 3.818) when a spinal needle was inserted in a cephalic needle bevel direction as compared to the parallel needle bevel direction. This result agrees with the findings of a study conducted by Amorim et al. in Brazil and the metanalysis conducted by. The possible explanation for this could be a tiny, slit-like hole is created when the arachnoid mater is punctured with a spinal needle that has been beveled. Therefore, it is hypothesized that parallel insertion of a beveled needle will disrupt/kill much fewer arachnoid cells than perpendicular insertion [38]. The occurrence of PDPH was also significantly correlated with the number of attempts in this study. The risk of developing PDPH was higher approximately by twofold for those who received SA on subsequent try compared to individuals who underwent a single attempt ARR=2.08, (95% CI: 1.253, 3.448). The result is like those of other studies [39]. As opposed to our findings, Dagmar Oberhofer et al.’s investigation revealed no connection between the number of attempts and the prevalence of PDPH [40].
- Research Article
- Abstract
- Introduction
- Materials and Methods
- Variables of the Study
- Operational Definitions
- Data Collection Tool and Procedures
- Data Quality Assurance
- Data Analysis and Management
- Ethics Approval and Consent to Participate
- Results
- Discussion
- Strength of the Study
- Limitations of the Study
- Conclusions
- Acknowledgements
- References
Strength of the Study
This study is a multicenteric and included patients with ranges of different operations performed under SA. So, the result can be generalized. The current study used a modified Poisson model for analysis, which enables to directly estimate of the effect of risk factors on outcome variables by risk ratio.
- Research Article
- Abstract
- Introduction
- Materials and Methods
- Variables of the Study
- Operational Definitions
- Data Collection Tool and Procedures
- Data Quality Assurance
- Data Analysis and Management
- Ethics Approval and Consent to Participate
- Results
- Discussion
- Strength of the Study
- Limitations of the Study
- Conclusions
- Acknowledgements
- References
Limitations of the Study
This study has limitations. First, the treatment strategies and long-term complications or effects of PDPH were not studied in this study. Secondly, in this study follow-up was for three days, PDPH may rarely occur up to seven days. Thirdly, this study couldn’t assess the effect of needle type on the occurrence rate of PDPH because all the lumber punctures in this study were performed using cutting-type needles.
- Research Article
- Abstract
- Introduction
- Materials and Methods
- Variables of the Study
- Operational Definitions
- Data Collection Tool and Procedures
- Data Quality Assurance
- Data Analysis and Management
- Ethics Approval and Consent to Participate
- Results
- Discussion
- Strength of the Study
- Limitations of the Study
- Conclusions
- Acknowledgements
- References
Conclusions
In this study, the incidence of PDPH among adult non-obstetric patients is comparable with findings of the other studies. However, PDPH was significantly higher in young patients, female sex, SA given by anesthesia students under supervision, large needle size, perpendicular needle bevel orientation, and multiple dural puncture attempts.
- Research Article
- Abstract
- Introduction
- Materials and Methods
- Variables of the Study
- Operational Definitions
- Data Collection Tool and Procedures
- Data Quality Assurance
- Data Analysis and Management
- Ethics Approval and Consent to Participate
- Results
- Discussion
- Strength of the Study
- Limitations of the Study
- Conclusions
- Acknowledgements
- References
Acknowledgements
Our gratitude goes to supervisors, data collectors, study respondents, Staffs, and managers in Wolaita Sodo University Compressive specialized, Worabe Comprehensive specialized, and Nigist Eleni Mohammed memorial Compressive specialized hospitals.
- Research Article
- Abstract
- Introduction
- Materials and Methods
- Variables of the Study
- Operational Definitions
- Data Collection Tool and Procedures
- Data Quality Assurance
- Data Analysis and Management
- Ethics Approval and Consent to Participate
- Results
- Discussion
- Strength of the Study
- Limitations of the Study
- Conclusions
- Acknowledgements
- References
References
- Society HCCotIH (2013) The international classification of headache disorders, 3rd edition (beta version). Cephalalgia 33(9): 629-808.
- Moore AR, Wieczorek PM, Carvalho JCJJN (2020) Association between post–dural puncture headache after neuraxial anesthesia in childbirth and intracranial subdural hematoma 77(1): 65-72.
- Jabbari A, Alijanpour E, Mir M, Rabiea SM, Rupani Mohammad A (2013) Post spinal puncture headache, an old problem, and new concepts: review of articles about predisposing factors. Caspian J Intern Med 4(1): 595-602.
- Kwak K-HJKjoa (2017) Postdural Puncture Headache 70(2):136-143.
- Amorim JA, Gomes de Barros MV, Valença MMJC (2012) Post-dural (post-lumbar) puncture headache: risk factors and clinical features 32(12): 916-923.
- Zorrilla Vaca A, Makkar JKJPP (2017) Effectiveness of lateral decubitus position for preventing post-dural puncture headache: a meta-analysis 20(4): E521-E529.
- Ferede YA, Nigatu YA, Agegnehu AF, Mustofa SYJIJoSO (2021) Incidence and associated factors of post dural puncture headache after cesarean section delivery under spinal anesthesia in University of Gondar Comprehensive Specialized Hospital, 2019, cross sectional study. 33: 100348.
- Schmittner MD, Terboven T, Dluzak M, Janke A, Limmer ME, et al. (2010) High incidence of post-dural puncture headache in patients with spinal saddle block induced with Quincke needles for anorectal surgery: a randomised clinical trial. Int J Colorectal Dis 25(6): 775-781.
- Oberhofer D, Jokić A, Skurić J, Vukelić M, Šklebar I (2013) Incidence and clinical significance of post-dural puncture headache in young orthopaedic patients and parturients. 115(2): 203-208.
- Salik F, Kiliç ET, Akelma H, Güzel AJA (2018) The effects of the quincke spinal needle bevel insertion on postdural puncture headache and hemodynamics in obstetric patients 12(3): 705-710.
- Bezov D, Lipton RB, Ashina Sait (2010) Post‐dural puncture headache: part I diagnosis, epidemiology, etiology, and pathophysiology 50(7): 1144-1152.
- Tien JC, Lim MJ, Leong WL, Lew E (2016) Nine-year audit of post-dural puncture headache in a tertiary obstetric hospital in Singapore 28: 34-38.
- Meyer Bender A, Kern A, Pollwein B, Crispin A, Lang M Philip (2012) Incidence and predictors of immediate complications following perioperative non-obstetric epidural punctures 12: 31.
- Talbot D, Mésidor M, Chiu Y, Simard M, Sirois CJE (2022) An alternative perspective on the robust Poisson method for estimating risk or prevalence ratios 34(1): 1-7.
- Guangyong Zou (2004) A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 159(7): 702-706.
- Zou GY, Donner Allan (2013) Extension of the modified Poisson regression model to prospective studies with correlated binary data. Stat Methods Med Res 22(6): 661-670.
- Tafesse D (2016) Assessments of the Magnitude of Post Dural Puncture Headache (PDPH) and Associated Risk Facrors with PDPH among Patients Undergoing Spinal Anesthesia for Orthopedics and Urologic Procedures in Black Lion Specialized Referral Hospital, Addis Abeba, Ethiopia.
- Bakshi SG, Gehdoo RS (2018) Incidence and management of post-dural puncture headache following spinal anaesthesia and accidental dural puncture from a non-obstetric hospital: A retrospective analysis 62(11): 881-886.
- Baamer RM, Iqbal A, Lobo DN, Knaggs RD, Levy NA (2022) Utility of unidimensional and functional pain assessment tools in adult postoperative patients: a systematic review 128(5): 874-888.
- Lee JH, Yoon DH, Heo Ha B (2020) Incidence of newly developed postoperative low back pain with median versus paramedian approach for spinal anesthesia 73(6): 518-524.
- Wu Y, Hallett M (2017) Photophobia in neurologic disorders 6: 26.
- Wang S, Borison Hljaon (1950) Psychiatry. The vomiting center: a critical experimental analysis 63(6): 928-941.
- Ferede YA, Nigatu YA, Agegnehu AF, Mustofa SY (2021) Incidence and associated factors of post dural puncture headache after cesarean section delivery under spinal anesthesia in University of Gondar Comprehensive Specialized Hospital, 2019, cross sectional study. Int J Surgery Open 33: 100348.
- Ferede YA, Nigatu YA, Agegnehu AF, Mustofa SY (2021) Incidence and associated factors of post dural puncture headache after cesarean section delivery under spinal anesthesia in University of Gondar Comprehensive Specialized Hospital, 2019, cross sectional study. Int J Surgery Open 33: 100348.
- Wadood R, Tariq AJK (2014) Post dural puncture headache; comparison of 25 and 27G spinal needles in urological patients. 7(1): 40-43.
- DelPizzo K, Cheng J, Dong N, Edmonds CR, Kahn RL, et al. (2017) post-dural puncture headache is uncommon in young ambulatory surgery patients. HSS J 13(2): 146-151.
- Parthasarthy S, Sivashanmugam TJAJPCR (2016) Incidence of post-dural puncture headache in Indian population: A need for a relook 9(2): 230-232.
- Pirbudak L, Özcan HI, Tümtürk PJAJotTSoA (2019) Postdural puncture headache: Incidence and predisposing factors in a university hospital. Agri 31(1): 1-8.
- DelPizzo K, Luu T, Fields KG, Sideris A, Dong N, et al. (2020) Risk of post-dural puncture headache in adolescents and adults. Ansh Analg 131(1): 273-279.
- Richman JM, Joe EM, Cohen SR, Rowlingson AJ, Michaels RK, et al. (2006) Bevel direction and postdural puncture headache: a meta-analysis. Neurologist 12(4): 224-228.
- Ready LB, Cuplin S, Haschke RH, Nessly MJA, Analgesia (1989) Spinal needle determinants of rate of transdural fluid leak. Anesth Analg 69(4): 457-460.
- Salzer J, Granåsen G, Sundström P, Vågberg M, Svenningsson AJEJoN. (2020) Prevention of post‐dural puncture headache: a randomized controlled trial. Eur J Neurol 27(5): 871-877.
- Gibson SJ, Helme RDJCigm (2001) Age-related differences in pain perception and report. Clin Geriatr Med 17(3): 433-456.
- Neuman SA, Eldrige JS, Qu W, Freeman ED, Hoelzer BCJPP (2013) Post dural puncture headache following intrathecal drug delivery system placement. Pain Physician 16(2): 101.
- Sarlani E, Greenspan JDJP (2002) Gender differences in temporal summation of mechanically evoked pain. Pain 97(1-2): 163-169.
- Doshi SM, Ramanuj R, Parmar RJIJCA (2019) Compare the incidence of post dural puncture headache of two different age groups and gender in elective lower limb surgeries: A prospective, observational study. Indian J Clin Anaesth 6(3): 415-419.
- Chaudry W, Saleem S, Naaman K, Waseen H, Javaid A, Waseem MBJPS (2009) Comparison of 22, 23 and 25 Gauge Quincke Needles for post dural puncture headache and identification of other significant factors for PDPH in a tertiary care hospital. 23(2): 55-60.
- Bernards CMJRA, Medicine P (2005) Sophistry in medicine: lessons from the epidural space. Reg Anesth Pain Med 30(1): 56-66.
- Weji BG, Obsa MS, Melese KG, Azeze GAJPM (2020) Incidence and risk factors of postdural puncture headache: prospective cohort study design. Perioper Med (London) 9(1): 32.
- Khraise WN, Allouh MZ, El-Radaideh KM, Said RS, Al-Rusan AMJL (2017) Assessment of risk factors for post-dural puncture headache in women undergoing cesarean delivery in Jordan: a retrospective analytical study. Local Reg Anesth 10: 9-13.






























