The Incidence and Predictors of Intraoperative Hemodynamic Change Following Thoracic Surgery in Ethiopia, 2023. Multi-Centre Approach
Yisehak Wolde1*, Mitiku Desalegn2, Adugna Arigawi3
1Department of Anesthesia, Lecturer. Wachemo University, college of Medicine and health science, Hosanna, Ethiopia
2Department of anaesthesia, lecturer, Tikur Anbessa Specialized Hospital, Addis Ababa University, Ethiopia
3Department of anaesthesia, Assistant professor in Anaesthesia, Tikur Anbessa Specialized hospital, Addis Ababa University, Ethiopia
Submission: February 20, 2024; Published: March 18, 2024
*Corresponding author: Yisehak Wolde, Department of Anaesthesia, Lecturer. Wachemo University, college of Medicine and health science, Hosanna, Ethiopia
How to cite this article: Yisehak W, Mitiku D, Adugna A. The Incidence and Predictors of Intraoperative Hemodynamic Change Following Thoracic Surgery in Ethiopia, 2023. Multi-Centre Approach. J Anest & Inten care med. 2024; 13(3): 555866. DOI 10.19080/JAICM.2024.13.555866
Abstract
Background: Hemodynamic instability, which is an independent predictor of long-term patient morbidity and duration of stay in the hospital. Multiple factors contribute to the development of intraoperative hemodynamic instability. Prevention and treatment of these factors may reduce patients’ hemodynamic change and its associated morbidity and mortality. This study aims to assess the incidence and associate factors of intra-operative hemodynamic change in patients undergoing elective thoracic surgery in TASH, Menilik II referral hospital, and SPSH 2023.
Methods: The institutions-based cross-sectional study was conducted among 181 adult patients who underwent elective thoracic surgery at Tikur Anbessa, Menilik II Referral Hospital, and Saint Peter Specialized Hospital from January 1, 2023, to April 30/2023. A systematic random sampling technique was used, and quantitative data were collected through interviews and data retrieval from charts using a pre-tested questionnaire. Both bi-variable and multi-variable logistic regression analyses were done to evaluate the association between independent and dependent variables. The level of statistical significance was declared at a p-value less than 0.05. The data was entered into Info 7.2.1 and analyzed by SPSS version 26 software performed descriptive statistics and bivariate and multivariate logistic regression.
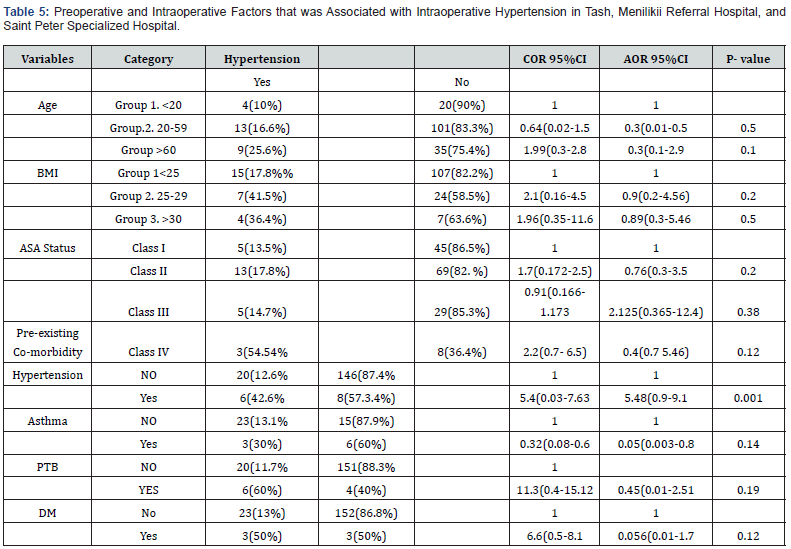
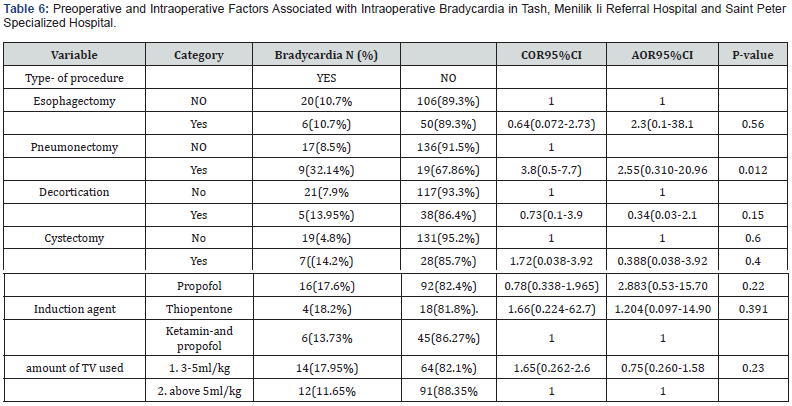
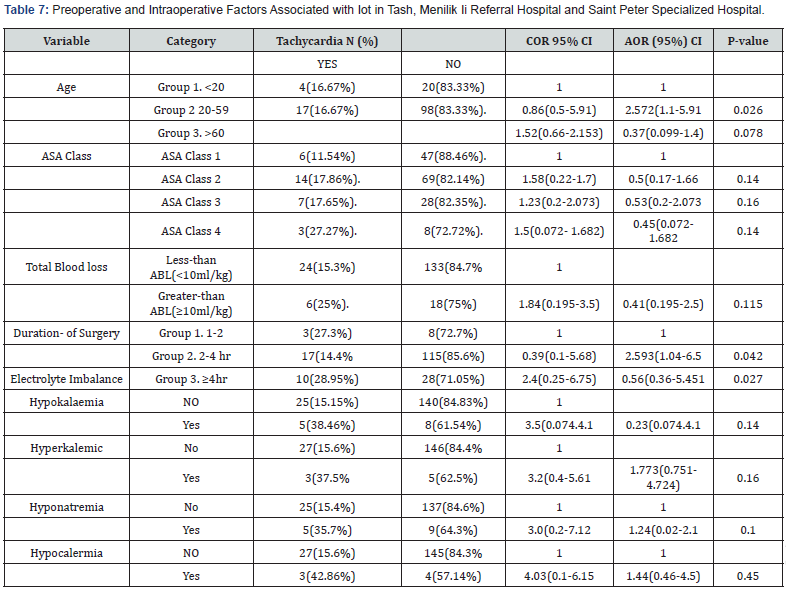
Result: A general of 181 patients’ information has been gathered during the observed period. The result of the study found that 74 (40.8%) patients, had intraoperative hypotension with 95%CI:(33.6%-48%),26(14.4%), hypertension,95% CI (9.6%-20%),30(16.6%), tachycardia, with 95%CI:(11.2%-23%) and,26(14.4%), patients-developed-intra-operative-bradycardia respectively. Intraoperative blood loss was statistically associated with intraoperative hypotension, [AOR = 9.58, 95% CI (2.57-35.8)], (p=0.001). The pre-existing co-morbidity associated with intra-operative hypertension, [AOR = 5.48, 95% CI:(0.91-9.1)] (P=0.001). The age and the duration of surgery were significantly associated with intra-operative tachycardia (AOR=2.6;95%CI (1s.04-6.5)(P=0.042). The type of procedure-pneumonectomy was strongly associated with intra-operative bradycardia (AOR=2.55,95%CI (0.310-20.96), (P=0.012).
Conclusion: The prevalence of hemodynamic change is higher during the intra-operative period. Blood loss, Age, type of procedure, pre-existing co-morbidity, and duration of surgery were identified as predictive factors.
Abbreviations: ASA: American Society of Anaesthesiology; ABL: Allowable Blood Lose; IOH: Intra-Operative Hypo/Hypertension, IOB: Intra-operative Bradycardia; MAP: Mean Air Way Pressure; PEEPs: Positive End Expiratory Pressure; SPSS: Statistical Package for Social Science; SBP: Systolic Blood Pressure; TASH: Tikur Anbessa Specialized Hospital; TEA: Thoracic Epidural Anaesthesia and TV Tidal volume.
Introduction
Thoracic surgery is a field of medicine that deals with the diagnosis and surgical treatment of inside the chest [1]. Thoracic surgery is an independent risk factor for perioperative complications, especially in patients with common- morbidities before surgery [2,3]. A thorough careful preoperative evaluation, smoking cessation, selection of the appropriate surgical procedure, and routine pre- and postoperative physiotherapy, can reduce mortality and major morbidity after lung resection [4-6]. The type of lung resection, either a lobectomy or a pneumonectomy influences resultant hemodynamic changes. Compared to preoperative values, both surgical approaches influence hemodynamics by increasing heart rate, mean pulmonary artery pressure, pulmonary capillary wedge pressure, and pulmonary vascular resistance as well as decreasing right ventricular ejection fraction [7,8].
The term hemodynamic refers to a physiological system concerned with the motion of blood inside the body. Hemodynamic balance calls for sufficient blood or fluid inside the body for the coronary heart to acquire and pump, ok strain from the heart to work in opposition to the systemic vascular resistance to transport the blood around the frame, and an efficaciously running pump to transport the obtained blood [9,10]. Several risk factors predict intra-operative hemodynamic instability. Risks can be patient, anaesthesia or surgery related. Age, history of medication, ASA physical status, and chronic disease are common patient related factors. Aesthetics, and other drugs, are anaesthesia-related factors. Intraoperative blood loss, surgeon expertise, operation type, and urgency may all influence the occurrence of intra-operative hemodynamic instability. Cardio-respiratory adverse events, and intra-operative pain may all play a role in the development of hemodynamic instability [11,12].
High prevalence of thoracic- surgical patients hemodynamic change even in developed countries, 58.3%,76.76. %, and 43.5%hypotension, hypertension, both hypotension and hypertension and 65% experienced changes in heart rate from the normal range [13]. respectively [14]. The intraoperative blood loss Age, smoking history, preoperative co-morbidity, coronary heart disease, anaesthetic agents use, and ASA status of a patients were identified as predictive factors [15]. There are different definitions given to intraoperative hypotension and hypertension during surgery with incidences and complications varying accordingly [16,17]. Evidence shows that: the definition of intraoperative hyper−/hypotension varied widely in the literature. In generally accepted that SBP > 160 mm-Hg during surgery is defined as intra-operative hypertension, and SBP < 80 mm-Hg as hypotension. Applying an absolute mean arterial pressure threshold of 65 mm Hg yielded an incidence of hypotension,65% for a greater than or equal to 1-min exposure, 49% for a greater than or equal to 5-min exposure, and 31% for a greater than or equal to 10-min exposure Respectively [18].
The main causes of vasovagal syncope, which is loss of consciousness because of inadequate blood flow to the brain and a mortality rate of 5–10%, are due to bradycardia and hypotension [19]. Evidence currently available suggests that MAP below 60 mm Hg sustained for 5 Min or more may be related to organ dysfunction and higher mortality [20]. Hemodynamic change is one of the peris- operative complications during t surgery the reviewer agree that: Surgical massive haemorrhage (22%,) was a significant cause of mortality another possible risk factor developed was preoperative Heart rate (<60 beats/ Min), preoperative hypotension, Elderly, preoperative renin- Angiotensin blockade Revised cardiac risk index (>3points), and Type of surgery. Although other research discovered that exact mechanisms of how intraoperative hemodynamic change affects long-term survival are yet unknown. Intraoperative hemodynamic change occurs despite frequent or even continuous intraoperative hemodynamic monitoring, Avoiding is a physiologic complex challenge for anesthesiologists.
Evidence currently available suggests that MAP below 60 mm Hg sustained for 5 Min or more may be related with organ dysfunction and higher mortality. Interestingly, a recent study showed that individualized intraoperative hemodynamic instability intervention reduced systemic- inflammatory response syndrome and organ dysfunction after surgery, although its long-term impact on surgical outcome has not been reported yet.
Methods and Materials
Study Design and Setting
The institutional-based cross-sectional study was conducted in three public specialized hospitals from January1 to April 30, 2023. The three hospitals were chosen for this study because they are the only government hospitals in Addis Ababa in which thoracic surgery is performed. Tikur Anbessa specialized Hospital (TASH), located in Addis Ababa which is the capital city of Ethiopia and the largest referral hospital. It offers diagnosis and treatment for approximately 370,000- 400,000 patients yearly, with nearly 8000 surgeries performed annually with 14 operation rooms. from these two operation tables in which thoracic procedure was performed and around 350 thoracic cases operated annually. Menilik II Referral Hospital is Established in 1909 after which Russia ties to Ethiopia after the Italian invasion in 1896. Today Menilik Hospital is operated by Addis Ababa Health bureau and has 6 major operating theatres. Approximately 230 thoracic surgeries are performed annually. Saint peter specialized hospital, one of the government hospitals in Addis Ababa, has five operation tables, from this one operation table in which the thoracic surgery is performed. Approximately 210 thoracic procedures were performed annually.
Population
All adult patients who underwent elective surgery were the source population and all eligible adult patients who fulfilled the inclusion criteria during the data collection period were the study population. During preoperative period, Patients with ASA Status >IV, those Patient who refused to give consent and patients with history of dementia were excluded from the study.
Sample Size Determination and Sampling Technique
The sample size was determined using the single population proportion method for the first objective, which is the magnitude of intraoperative hemodynamic change during elective thoracic surgery. Since no related study was found in Ethiopia or Africa, P = 0.5 was used for calculation to get the maximum sample size, 95% level of significance, 5% margin of error, and 10% for incomplete or as contingency data was used as parameters. Population correction used since the source population is<10,000. Situational analysis of thoracic surgeries was done 3 months before the start of the study and an average of 60 procedures is done per month.
The sample size is calculated as follows:
Since the size of the population is less than 10,000 this study uses a correction formula as follows
N = the total number of surgical patients who are undergoing surgery by general Anaesthesia which is 300.
The sample size was 168 and, adding 10% for non-response rate, the final sample was 185.
A systematic random sampling method was used. Potential study subjects were all eligible patients scheduled for elective thoracic surgery and their names were selected and included in the surgery list. A list of all adult patients scheduled for thoracic surgery was collected from the theatre lists and submitted to the operating theatre a day prior to the scheduled surgical procedures. After Situational analysis was done for 3 months before the start of the study, an average of 330 elective surgery cases (200 in TASH and 75 in Menilik referral hospital 55 saint peters specialized hospital) are found to be done in three months in three hospitals. After proportional allocation, 112 study subjects from TASH and 42 Study subject from Menilik referral and 31 cases from SPSH were taken.
K was determined using the formula: K=N/n, where n = total sample size and N = population. Therefore, the sampling interval was two and the first study participant (random start) was selected using a lottery method from each daily surgical schedule. Each day before elective surgery begins, patients are selected by a systematic random sampling technique from each group of surgical schedule. Then, every second case from the daily surgical procedures was included in the study during the study period. The intention of including them in the study, the aim and benefits of the study, and the data collection procedures were explained. A preliminary assessment of whether the patient fulfills the inclusion criteria was made, and those who met the inclusion criteria were included. This procedure was repeated on each day of data collection until the required sample size was attained.
Operational Definitions
American Society of Anaesthesiologists (ASA) physical status classification: developed by the ASA task force which classifies patients according to their physical status (systemic well-being [21].
ASA class I: normal healthy patient except for the surgical complaint he had.
ASA class II: a patient with a mild systemic disease without substantive functional limitation.
ASA class III: a patient with a severe systemic disease with substantive functional limitations.
ASA class IV: a patient with severe systemic disease that constantly threatens life. life. ASA class V: the moribund patient who is not expected to survive without the operation.
Baseline value: is the value taken before induction.
Hemodynamic Change: patient has experience at least one of the physiologic parameters including, systemic hypertension, hypotension, tachycardia, bradycardia, or combination [22].
o Hypotension: a decrease in ≥30% from baseline value or for adult SBP<80mmhg [23].
o Hypertension: adult patients an increase in ≥30% from base line or SBP>160mmhg [24].
o Tachycardia: an increase in heart rate, >=20% from base line value.
o Bradycardia: a decrease in heart rate, ≥30% from the baseline value.
Data Collection Tool, Method, and Procedure
Data was collected using a structured pretested questionnaire by data collectors from January 01 to April 30, 2023. Questions in the questioner include socio-demographic data, clinical patient characteristics, and different surgical and anesthetic variables. Socio-demographic and preoperative clinical data were extracted from the patient’s records on the morning of surgery. Intraoperative anaesthetic and surgical data were collected from the intraoperative anaesthesia charts. Data was collected by three trained anesthetists; this was done on the morning of surgery, in the intraoperative period and this continued until the desired number of patients is achieved. Medication, Co-morbidity, and medical history were extracted from patients’ medical records. Immediately, after the patient entered the operation room, the data collector records baseline blood pressure and heart rate before induction and records blood pressure and heart rate post-induction.
The air way pressure value record was taken immediately after securing the air way. The intra-operative blood loss, type of drug used, amount fluid or blood took and urine out-put, were obtained from an anesthesia record sheet. Airway pressure (PAP, MAP) and PEEP were monitored by integrated airway pressure monitors on the anaesthesia machines. Blood pressure was monitored using an automatic non-invasive blood pressure monitor and an invasive Arterial Blood pressure monitoring system. A pulse oximeter and electrocardiograph were used to measure the pulse rate.
Data Quality Assurance
To assure the quality of the data, training on the objectives and relevance of the study and brief orientations on the assessment tools were provided for the data collectors. The questionnaires were prepared in English and pretested on 5% of the study population. The results of the pretest weren’t included in the final analysis. During data collection, each question was revised by the investigator to be complete and appropriate. In the event of missed measurements during the intraoperative period, the electronic data stores of the monitoring equipment were recalled and back traced, and the data was filled.
Data Analysis
Data were coded, edited, entered, and cleaned in Epi Info version 7.2 before being exported to the Statistical Package for Social Sciences (SPSS) software version 26.0. Using SPSS basic descriptive statistics like frequency of preoperative and intraoperative factors, socio-demographic variables and prevalence of Hemodynamic change was done. Bivariate and multivariate logistic regression analyses were done to determine the presence of associations between dependent and independent variables, and the odds ratio with 95% confidence intervals was used to determine the degree of association between dependent and independent variables. The prevalence was calculated as the proportion of patients with intraoperative hemodynamic change with a 95% confidence interval. Variables with a p-value less than equal to 0.25 in the bivariate logistic regression analysis were considered for multi-variable analysis. After checking for multicollinearity, Ulti variable analysis was performed to adjust for possible con founders and come up with significant predictors. The statistical tests were performed at a 5% significance level. The results were presented by using text, tables, charts, and graphs.
Results
Socio, Democratic characteristics of patients
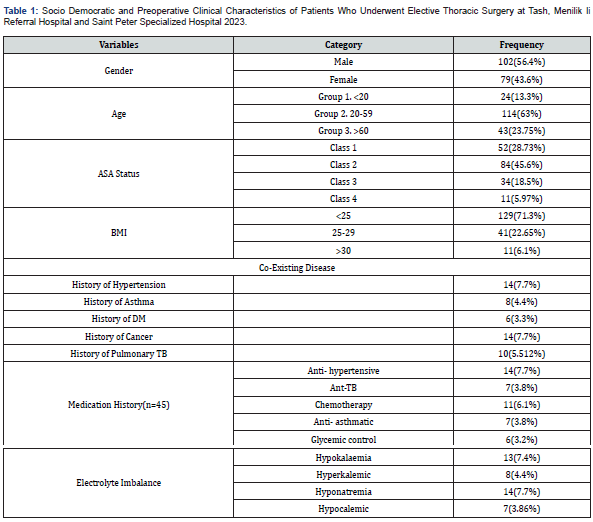
One hundred and eight-five patients were enrolled in the study. From this study subjects’ four patients’ documents with incomplete records were also excluded. The results presented were for the remaining 181 patients. The total number of male and female respondents was 102(56.4%),79(43.6%) respectively. The median age of patients was 39±12. Regarding American Society of Anesthesiology, most of the patients were ASA II 84(46.4%), ASAI was 52(28.75%), ASA III 34(18.5%) and ASA IV 11(5.97%). Concerning Co-morbidities, 14(7.7%) patients had hypertension, 10 (5.5%) patients had pulmonary infection, 9(5%) had asthma and 14 (7.7%) had Malignancy or Cancer and 6(3.3%) had a history of DM (Table 1).
Anaesthetic and Surgical Characteristics of Patients
All the (181) patients underwent their surgeries under General Anaesthesia with Endotracheal intubation. Intra-operative anaesthesia was maintained with volatile anaesthesia with halothane and Isoflurane, and with long-acting muscle relaxant. The Intermittent boluses of fentanyl and Epidural anaesthesia technique was used for intraoperative pain for 98(54.1%) and paravertebral or erector spinae block was used in 31(17.13%) patients, 82(45%) patients were given both Fentanyl and morphine. Most of the Procedure took more than two-hour duration 132(72.9%), (Table 2).
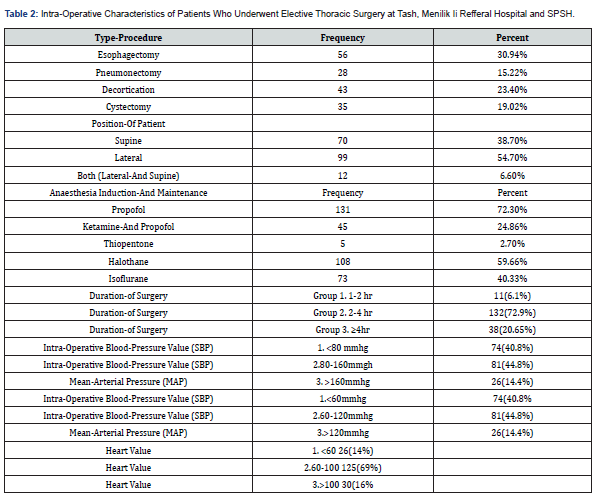
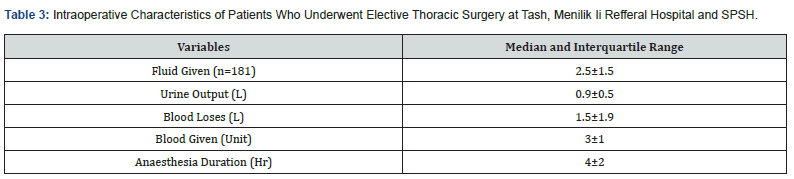
Invasive monitoring with the arterial catheter was used on 69(38.1%) patients for blood pressure monitoring. The intra-operative median systolic blood pressure of patients was 109±11. The lowest intraoperative median systolic blood pressure value was 70±9. The intraoperative median mean arterial blood pressure was 68±13.the lowest intraoperative median mean arterial blood pressure 49±7. The intra-operative median heart rate value was 73±18.the lowest intraoperative median heart rate value was 50±7. Treatment of intraoperative hemodynamic change is according to the attending anesthetist or anesthesiologist. Noradrenaline was used on 29(16%) and Adrenaline was used on 10(5.5%) patients for treatment-of intraoperative-hypotension inhalational agent and beta blocker used to treat intraoperative hypertension for 15(8.3%) and atropine was given to 17(9.4%) patients to treat intraoperative bradycardia and lidocaine used to treat tachycardia for 11(6.1%) patients (Table 3).
Blood pressure and heart rate variable during preoperative and intraoperative period
The baseline median systolic blood pressure of patients was 119±6 and post-induction median systolic blood pressure value of patients were 105±40.From this value 74(40.8%) patients had developed intra-operative hypotension which were ≥30% decrease from baseline, and lowest intra-operative median systolic blood pressure value of patients were 70±9. From this post induction systolic blood pressure value 16(8.8%) patients decrease <30% from base line value of patients which were not considered as hypotension according to our operational tool.
From post-induction systolic blood pressure 26(14.4%) patients had developed intra-operative hypertension which was increased ≥30% from baseline, and highest intra-operative median systolic blood pressure value were 159±10.From this post-induction systolic blood pressure value 8(4.4%) patients increase <30% from base line systolic blood pressure which was relative threshold value to detect intra-operative hypertension. The baseline median heart value of patients were 74±13 and post-induction median heart rate value of patients were 80±30.From this heart rate value 30(16.6%) patients had developed intra-operative tachycardia which increased ≥20% from base line, and highest intra-operative median heart value was 130±25.from this post-induction heart rate 5(2.8%) patients increased <20% from baseline heart rate value, which was not fulfil our operational definition.
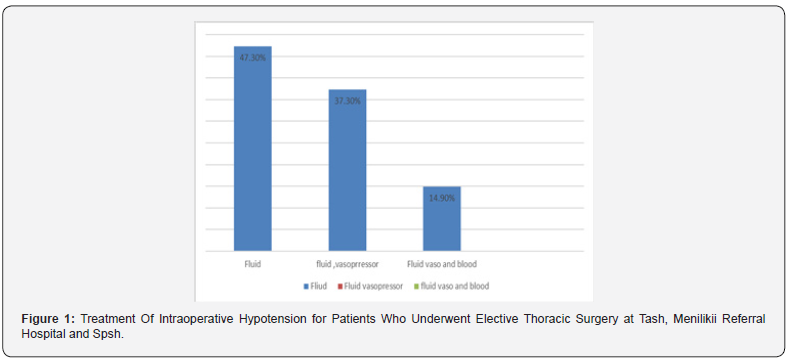
From post-induction heart rate value 26(14.4%) had developed intra-operative bradycardia which was increased ≥30% from baseline, and the lowest intra-operative median heart rate value was 50±7.from post-induction heart rate 11(6.1%) patients decreased <30% from baseline heart value, which was relative threshold criteria to detect intra-operative bradycardia. Of, total 181 patients, 74(40.8%) had developed intra-operative hypotension,26(14.4%), hypertension, 30(16.6%), tachycardia and 26(14.4%) intraoperative bradycardias respectively. The lowest intraoperative median mean arterial blood pressure was 49±7. The lowest intraoperative median heart rate value was 50±7. The highest intra-operative median heart rate value was 140±25, (Figure 1).
Associated Factors of Intra Operative Hemodynamic Change
Binary logistic regression analysis was conducted to see the association between independent variables and intraoperative hemodynamic change. According to bivariate analysis, presence of intraoperative blood loss with greater than allowable loss, Increasing ASA class, pre-existing co-morbidity like asthma was associated with an increase in the likelihood of exhibiting intraoperative hypotension. Patients having preexisting-co-morbidity, like hypertension, are susceptible to hypertension. Duration of surgery, and age of patients was significantly associated with intra-operative tachycardia. Patients having pre-existing co-morbidity like hypertension, susceptible to intra-operative hypertension [COR=0.093; 95% CI: 0.03-0.32], compared with patients who don’t have co-morbidity.
Intra-operative Tachycardia was 2.4 times more likely to occur during the duration of surgery longer than 2hr, compared with duration [COR=2.4 95% CI: (1.-5.68)] of surgery that took less or equal to 2hr. In comparison to age group, patients with increasing age were associated with intraoperative Tachycardia. The likelihood of developing intra-operative tachycardia was 2.57 times [COR=2.57; 95% CI: (1.119-5.91)] higher among patients who were younger ages. The type of procedure such as pneumonectomy was strongly associated with Intra-operative Bradycardia [COR=0.234(0.051-1.074). After excluding variables which doesn’t fit for the model using P-value ≥0.25 in Likelihood ratio test, multi-variable analysis was performed, for those selected variables intraoperative blood loss, type of diagnosis like lung emphysema, and patients having hypertension and asthma as a co-existing disease were associated with intra-operative hypotension. Patients with intra-operative blood loss greater than allowable blood loss (s10ml/kg of total estimated blood volume) were 9 times (AOR=9.584.; 95%CI: (2.57-35.8), more likely of developing intra-operative hypotension compared to patients with less than allowable blood loss (<10ml/kg of estimated blood volume of patients (Table 4).
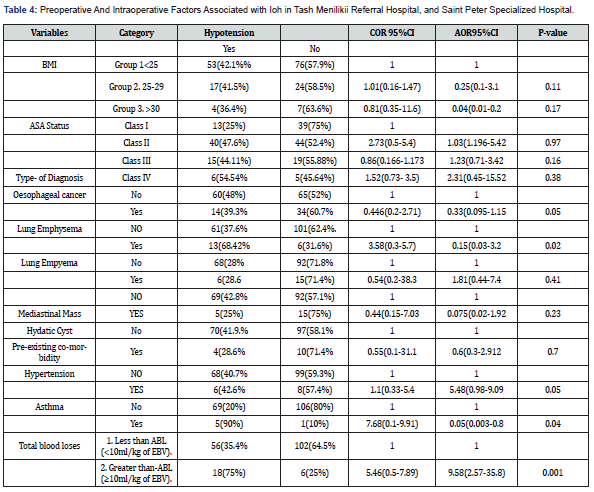
**Statistically Significant.
From this study result, patients having pre-operative- poorly controlled hypertension were likely to develop intra-operative hypertension (AOR=5.48:95%CI (0.9-9.1), in reference to patients who have no pre-operative hypertension (Table 5). According to this study finding, this type of procedure had a higher risk of developing intra-operative, bradycardia. The nature of the procedure, like pneumonectomy or lobectomy, was 2.55 times (AOR=2.55; 95%CI:(0.310-20.96) more likely of developing intra-operative bradycardia than patients with another type of procedure-cystectomy (AOR=0.388;95%CI: (0.038-3.92). (Table 6) According to this study result, the age patient and the duration of surgery increase, the higher chance of developing intra-operative tachycardia, so the duration of a procedure longer than two hours was 2.4 times (AOR=2.4;95%CI:(1.03-5.68) more risk of developing intra-operative tachycardia with the procedure, that took less than two hours (Table 7).
Discussion
Intraoperative Hypotension
According to this study, there is a higher magnitude of Intra-operative hypotension for those who have underwent elective thoracic surgery. The prevalence of intraoperative hypotension was obtained to be 40.8% (95% CI: 33.8%-48.2%). This magnitude is lower than a study done by D. Sharma et al in India where 65% (n=73) of the patients had at least one episode of hypotension [25,26]. But it is greater than the result of research conducted by G. Singh et.al in college of India which the magnitude of hypotension was reported as 16.6%, which was none cardio-thoracic surgery performed with endoscopic, therefore, magnitude of intra-operative hypotension is lower than our study result. This study finding, nearly in-line to the study done by Korkomaz et.al, who stated an IOH incidence of 37.6% in adults [27,28]. Our study result, like a cross-sectional study conducted by Dr Heshmat, in Iran, after surgery, 36% of patients experienced changes in systolic blood pressure 49% shows diastolic blood pressure changes [29].
The magnitude of the result of this study is lower than a prospective study done at the University of British Columbia, study was conducted on 193 Elective surgical patients. The prevalence of hypotension or bradycardia was 127(65.8%). A final five risk factors were developed such asper-operative rate (<60 Min), preoperative hypotension (<110/60mmhg), Elderly, pre-operative, ACE inhibitors or beta blocker, Revised cardiac risk index (>3 points), and type of surgery. Our Study finding is lower than a retrospective cohort study conducted by Zhang, Mu et al.in Shanghai Chest Hospital, in 676 patients were done lung cancer surgery. An overall magnitude, intraoperative hypotension,160(58.3%), A higher incidence of hypotension in this study may be attributed to the frequent use of intra-arterial invasive monitoring which has a better detection ability of intra-operative blood pressure change. They also used systolic blood pressure threshold value less than 100-mmhg for, ≥ 5-minute exposure, for hypotension.
The risk factors for a study conducted above were age, smoking history, preoperative co-morbidity, coronary heart disease, anaesthetic agents used and ASA status of the patient and intraoperative blood loss. Our study result, risk factors were nearly Similar to this finding. It was also observed, in the study conducted in, Germany in perioperative blood pressure management. For instance, in this study, the incidence of intraoperative hypotension varies substantially depending on the selected definition, taking a 20% drop in systolic blood pressure, into account led to incidences of intra-operative hypotension of 93% for exposure lasting more than or equal to one minute,88% for exposure lasting 5 minutes. Applying an absolute mean arterial pressure threshold of 65 mm Hg yielded an incidence of intra-operative hypotension of 65% for a greater than or equal to 1-min exposure, 49% for a greater than or equal to 5-min exposure, and 31% for a greater than or equal to 10-min exposure.
Our study also applied an absolute mean arterial pressure threshold of 60 mm Hg for a greater than or equal to 5 -min exposure, to detect the incidences of intra-operative hypotension, so the finding is nearly close to our study result. According to our research findings, the prevalence of intra-operative hemodynamic change was 74(40.8%), hypotension 26(14.4%), hypertension,30(16.6%) tachycardia, and 26(14.4%) intra-operative bradycardias, respectively. this study result was nearly in line with the study done by, Gyaninder P, Singh in India Medical College, on 298 patients, Ganjoo P. et.al found the incidence of tachycardia as (20.1%) bradycardia (12.4%) and hypertension (8.3%). In this study result, intra-operative blood loss is strongly associated with intra-operative hypotension. Patients with intra-operative blood loss greater than allowable blood loss were 9 times (AOR=9.584.; 95%CI:( 2.57-35.8), more likely of developing intra-operative hypotension compared to patients with less than allowable blood loss. This study result is consistent with the study conducted in England, on 676 patients who underwent lung cancer surgery.
Intraoperative Hypertension
The magnitude of the intraoperative hypertension (14.4%) in this study, lower than study conducted by Zhang, Mu et al.in Shanghai Chest Hospital, the magnitude of hypertension was (76.9%), A higher incidence of hypertension in this study may be attributed to the frequent use of intra-arterial invasive monitoring which has a better detection ability of intra-operative blood pressure change. They also used systolic blood pressure threshold greater than 140-mmhg for ≥ 5-minute exposure, and systolic blood pressure less than 100-mmhg for hypertension and hypotension respectively.
The pre-operative co-morbidity like hypertension was strongly associated with intra-operative hypertension. The study of our result shows, patients having pre-hypertension were prone to develop intra-operative hypertension compared with patients without pre-hypertension. This finding is in line with the study done in Canada Toronto hospital, to identify the common ethologies of hypertension during the perioperative period. From this research finding (22.7%) intra-operative hypertension was poorly controlled pre-hypertension [30]. In another research done by G. Singh et.al on 223 patients were analysed, and reported incidences of hypertension, at 16.1%, this finding closes our study result.
Intraoperative Bradycardia
In another research done by G. Singh et.al on 223 patients were analysed, and reported incidences intra-operative bradycardia at 11.3%, (27,28). This study was nearly in line with our study finding which was 14.4%. It was also observed in our study, the type of procedure of was higher risk of developingis nearly operative bradycardia. The nature of the procedure, pneumonectomy, or lobectomy was 2.55 times (AOR=2.55;95%CI:(0.310-20.96) more likely of developing intra-operative bradycardia than patients with other types of procedure, like Cystectomy (AOR=0.388;95%CI: (0.038-3.92). This finding is also nearly close to, the study was done by Brodsky JB. Review anaesthesia in thoracic surgery, and Etienne J Coulture Current challenge in thoracic surgery [31].
Intraoperative Tachycardia
According to our research findings, the prevalence of intra-operative tachycardia was (16.6%) which was nearly in line with study conducted by G singh et al. incidence of tachycardia was (18%). According to this study result, the duration of surgery was associated with intra-operative tachycardia. So, the duration of the procedure longer than two hours was 2.4 times more risk of developing intra-operative tachycardia with the procedure, which took less than two hours. This finding is similar with the study conducted by Dr Heshmat educational-therapeutic hospital in Rasht in the province of Iran. The study aimed to determine the level of hemodynamic changes after coronary artery bypass grafting and its related factors [32].
Limitation of the Study
Pre-operative screening of coexisting medical disease was missed in some patients because of lack standard investigation tool. The only way to identify this group of patients is variable screening test for each diagnosis. These tests are expensive and are not done routinely in our set-up. Some patients may be undiagnosed for some specific medical disease. Because these factors may influence the outcome variable, the findings of this study interpreted with these limitations in mind.
Conclusion
The finding of this study had high intra-operative hypotension episodes which was found to be 40.8%, in patients who underwent elective thoracic at TASH, Menilik II referral Hospital and Saint Peter Specialized Hospital. Hypertension, Tachycardia and Bradycardia had a magnitude 14.4%,16.6% and 14.4% respectively. Age, ASA class, type of diagnosis, intra-operative blood loss, type of procedure-existing co-morbidity and duration of surgery were predictors of intra-operative hemodynamic change of patients who underwent elective thoracic surgery at Tikor Anbessa specialized hospital, Menilik II referral hospital, and Saint Peter specialized hospital from February 1 /2023 to April 30 ,2023.
Acknowledgement
I would like to thank you Addis Ababa University Department of Anaesthesia for giving me the opportunity to conduct this study. My deepest heart-full gratitude and thanks to my advisor’s Mr Hirbo Samuel (MSc Lecturer in Anaesthesia Department) and -Mr. Adugna Argawi (Assistant Professor in Anaesthesia) for their continuous comments and valuable advice to develop this research. I would also like to thank you and the data collector for their support with data collection. Finally, I would like to extend my gratitude to those authors and researchers of articles for their valuable work I have read and cited.
References
- Joe B Putnam (2015) Lung, Chest Wall, Pleura, and Mediastinum. Thoracic Key 47-60.
- Halvorsen S, Mehilli J, Cassese S, Hall TS, Abdelhamid M, et al. (2022) 2022 ESC Guidelines on cardiovascular assessment and management of patients undergoing non-cardiac surgery. Eur Heart J 43(39): 826-3924.
- Li Q, Zhang X, Xu M, Wu J (2019) A retrospective analysis of 62,571 cases of perioperative adverse events in thoracic surgery at a tertiary care teaching hospital in a developing country. J Cardiothorac Surg 14(1): 98.
- R Peter Alston, Paul S Myles, Marco Ranucci (2015) Textbook O Cardiothoracic Anaesthesia 14(1): 415-422.
- Roy E, Rheault J, Pigeon MA, Ugalde PA, Racine C, et al. (2020) Lung cancer resection and postoperative outcomes in COPD: A single-center experience. Chron Respir Dis 1479973120925430.
- Lugg ST, Tikka T, Agostini PJ, Kerr A, Adams K, Kalkat MS, et al. (2017) Smoking and timing of cessation on postoperative pulmonary complications after curative-intent lung cancer surgery. J Cardiothorac Surg 12(1): 52.
- Brodsky JB (2017) Preoperative assessment Anesthesia for thoracic surgery. In: review anesthesia for thoracic surgery.
- Etienne J Couture (2022) Pulmonary hemodynamics and lung surgery: Narative Review. Curr Challenges Thorac Surg 5.
- Mulugeta M, Riskey N, Mollalign M, Adie B (2022) Incidence and predictive factors associated with hemodynamic instability among adult surgical patients in the post-anesthesia care unit, 2021: A prospective follow up study. Ann Med Surg 74: 103321.
- Abebe B, Kifle N, Gunta M, Tantu T, Wondwosen M, et al. (2022) Incidence and factors associated with post-anesthesia care unit complications in resource-limited settings: An observational study. Heal Sci Reports 5(3): e649.
- 00000542-199604000-00003HDI14FROM12.pdf.
- Abid Saleem, wahid Syed (2019) change in blood gases and hemodynamic parameters patients undergoing lung resection surgery and it implicationg go lung resection surgery. J Cardio Thorac Med 7: 406-412.
- Ahmadi N, Reza Masouleh S, Shekani Z, Kazem Nezhad Leili E (2012) Hemodynamic changes and related factors in patients undergoing coronary artery bypass grafting surgery. J Holist Nurs Midwifery 22(2): 1-10.
- Huang WW, Zhu WZ, Mu DL, Ji XQ, Li XY, et al. (2020) Intraoperative hypotension is associated with shortened overall survival after lung cancer surgery. BMC Anesthesiol 20(1): 1-160.
- Kouz K, Hoppe P, Briesenick L, Saugel B (2020) Intraoperative hypotension: Pathophysiology, clinical relevance, and therapeutic approaches 64(2): 90-96.
- Soto ruiz KM, Peacock WF, Varon J (2011) Perioperative hypertension: Diagnosis and Treatment. Journal Crit care 15(3): 143-148.
- Foe P (2004) Intraoperative Hypotension Is Associated with Adverse Clinical Outcomes After Noncardiac Surgery. Anesth Analg 4(5): 139-143.
- Lizano-Díez I, Poteet S, Burniol-Garcia A, Cerezales M (2022) The burden of perioperative hypertension /hypotension: A systematic review 17(2): e0263737.
- Hirsch J, DePalma G, Tsai TT, Sands LP, Leung JM (2015) Impact of intraoperative hypotension and blood pressure fluctuations on early postoperative delirium after non-cardiac surgery. Br J Anaesth 115(3): 418-426.
- Saugel B, Sessler DI (2021) Perioperative Blood Pressure Management. Anesthesiology 2: 250-261.
- De Cassai A, Boscolo A, Tonetti T, Ban I, Ori C (2019) Assignment of ASA-physical status relates to anesthesiologists’ experience: A survey-based national study. Korean J Anesthesiol 72(1): 53-59.
- Mulugeta M, Riskey N, Mollalign M, Adie B (2021) Incidence and predictive factors associated with hemodynamic instability among adult surgical patients in the post-anesthesia care unit: A prospective follow up study. Ann Med Surg 74: 103321.
- Cheung CC, Martyn A, Campbell N, Frost S, Gilbert K (2015) Predictors of Intraoperative Hypotension and Bradycardia. Am J Med 128(5): 532-538.
- Kurz A, Turan A, Rodseth RN, Cywinski J, Thabane L, et al. (2013) Perioperative hypertension: Diagnosis and Treatment. Perioper Med 3: 507-515.
- Sessler DI, Bloomstone JA, Aronson S, Berry C, Gan TJ, et al. (2019) Perioperative Quality Initiative consensus statement on intraoperative blood pressure, risk, and outcomes for elective surgery 122: 563-574.
- Medicine P (2013) Relationship between Intraoperative Mean 119(3): 507-515.
- Hirsch J, DePalma G SL (2015) Impact of intraoperative hypotension and blood pressure fluctuations on early postoperative delirium after non-cardiac surgery - PubMed impact of hypotension. 418-428.
- Singh GP, Prabhakar H, Bithal PK, Dash HH (2011) A retrospective analysis of perioperative complications during intracranial neuroendoscopic procedures: Our institutional experience Neurology India 59(6): 874-878.
- Koli PG, Shetty Y, Salgaonkar S, Dongre M, Arora S (2019) Cross-sectional study about perioperative management of Blood Pressure and effects of anaesthesia in hypertensive patients undergoing general & orthopaedic surgery. Egypt J Anaesth 34(3): 89-93.
- Mohseni S, Behnam-roudsari S, Tarbiat M, Shaker P (2022) Perioperative Hypertension Etiologies in Patients Undergoing Noncardiac Surgery in University Health Network Hospitals- Canada from 2015-2020. Integr Blood Press Control 23-32.
- Cabo D, Alarza FH, Rodriguez AMC, Delgado MCM (2020) Perioperative management in thoracic surgery 44(3): 185-191.
- Ahmadi N, Reza Masouleh S, Shekani Z, Kazem Nezhad Leili E (2012) Hemodynamic changes and related factors in patients undergoing coronary artery bypass grafting surgery. J Holist Nurs Midwifery 22(2): 1-10.






























