Comparison of EMS and Non-EMS Transportation Outcomes Among ST-Segment Elevation Myocardial Infarction (STEMI) Patients: A Systematic Review and Meta-Analysis
Ayman Elsayed Sleim Mohamed*
Riyadh University Hospital, Dar Al Uloom University, Riyadh, Saudi Arabia
Submission: January 03, 2024; Published: January 23, 2024
*Corresponding author: Ayman Elsayed Sleim Mohamed, Riyadh University Hospital, Dar Al Uloom University, Riyadh, Saudi Arabia
How to cite this article: Ayman Elsayed Sleim Mohamed. Comparison of EMS and Non-EMS Transportation Outcomes Among ST-Segment Elevation Myocardial Infarction (STEMI) Patients: A Systematic Review and Meta-Analysis. J Anest & Inten care med. 2024; 13(3): 555861. DOI 10.19080/JAICM.2024.13.555861
Abstract
Background: Emergency Medical Services (EMSs) are essential for diagnosing and treating myocardial infarction with ST-segment elevation (STEMI).
Aim: The current meta-analysis aimed to compare the outcomes, survival rates and incidence of complications between STEMI patients transported by EMS vs. non-EMS transportations.
Method: The literature on prehospital care for STEMI sufferers was filtered out by examining the published research in online libraries from 2008 to 2023. The article at hand covered eight indicators of outcomes in total: (1) Symptom-to-balloon time (SBT), (2) Door-to-balloon time (DBT), (3) mortality rate, (4) symptom-to-door time (STDT), (5) heart rate (HR), (6) systolic blood pressure (SBP), (7) door to-needle time (DNT) and (8) symptom-to-door time (SNT). 7 papers reported patients’ complications. To assess bias risk, Egger’s test and a funnel plot were employed.
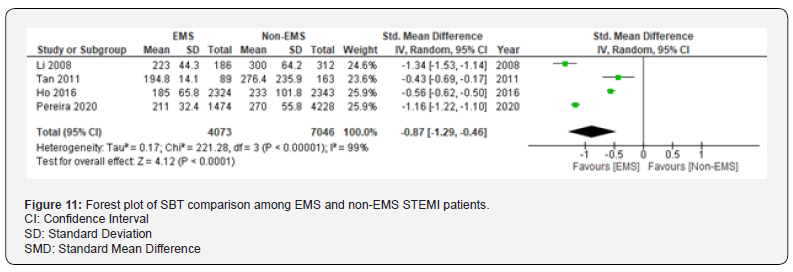
Results: 11 published papers were included with a total of 56579 STEMI patients (29607 patients in the EMS group and 26972 patients in the non-EMS group). The in-hospital mortality risk ratio among EMS and non-EMS STEMI patients did not significantly differ (p=0.17) (RR =1.09, 95% CI: 0.96 to 1.24). DBT of the STEMI patients transferred by EMS was significantly lower than STEMI patients transported by other means of transportation (SMD =−0.52, 95% CI: −0.97 to −0.08, P=0.02). SBP of the STEMI patients was lower among EMS patients than patients transported by non-EMS means (SMD =−0.27, 95% CI: −0.58 to −0.03, P=0.08). HR of the where EMI patients was significantly reduced among EMS transported patients than non-EMS transported patients (SMD =−0.08, 95% CI: −0.16 to −0.01, P=0.03). SBT was significantly lower among STEMI EMS transported patients than non-EMS patients (SMD =−0.87, 95% CI: −1.29 to −0.46, P<0.001). STDT of the STEMI EMS transported patient significantly reduced than non-EMS patients (SMD =-0.94, 95% CI: -1.41 to -0.46, P< 0.001). DNT of the STEMI EMS transported patient was significantly lower than non-EMS patients (SMD =-0.46, 95% CI: -0.65 to -0.27, P< 0.001). The complications rate after treatment among non-EMS STEMI patients was significantly higher than those patients transported by EMS means (RR =1.24, 95% CI: 1.01 to 1.52, P=0.04).
Conclusions: The current meta-analysis provided evidence that STEMI sufferers who used EMS transport had a reduced mortality rate than patients who used other means of transportation. It is advised that healthcare administrators and legislators take the required steps to raise public health consciousness and education regarding the usage of emergency medical services (EMS), which will lower the death rate and problems associated with acute myocardial infarction (AMI).
Keywords: Emergency Department; Myocardial Infarction with ST-Segment Elevation (STEMI); Survival Rate; Pre-Hospital Transport
Abbreviations: EMS: Emergency Medical Services; STEMI: ST Segment Elevation; SBT: Symptom-To-Balloon Time; DBT: Door-To-Balloon Time; STDT: Symptom-To-Door Time; HR: Heart Rate; MA: Mortality Rate; SBP: Systolic Blood Pressure; DNT: Door To-Needle Time; SNT: Symptom-To-Door Time; AMI: Acute Myocardial Infarction; CVD: Cardiovascular Diseases; WHO: World Health Organization; NOS: Newcastle Ottawa Scale; SMD: Standard Mean Differences; CI: Interval; RR: Risk Ratio; PPCI: Primary Percutaneous Coronary Intervention; CPR: Cardiopulmonary Resuscitations; VF: Ventricular Fibrillation
Introduction
Being the main reason of death, the incidence of cardiovascular diseases (CVD) has emerged as one of the biggest threats to the medical sector in most cultures [1]. among the most significant cardiovascular conditions is acute myocardial infarction (AMI) with ST elevation (STEMI), which has the greatest rates of hospitalization and deaths. STEMI patients and the healthcare system bear a substantial financial burden from the expenses of medical care, treatment, and re-admission [2,3]. The World Health Organization (WHO) states that AMI accounts for 30% of mortality in developing nations and 50% of deaths in advanced economic nations [4,5]. Numerous studies have demonstrated that, despite AMI’s potentially fatal outcomes-such as heart attack, stroke, and death-its suitable management, prompt and efficient clinical procedures, and the timely transfer of patients to medical facilities all significantly lower the disease’s complications and mortality rate [6].
Because early identification and treatment-such as initial angioplasty and the administration of thrombolytic medications, which restore blood flow to a blocked artery-have been effective in reducing the degree of associated risks and complications, half of AMI patients die if they do not receive treatment in the initial stages of the illness [7]. When it comes to management and treatment of AMI, timing is crucial. For example, the European Society of Cardiology suggested that the initial angioplasty be carried out no later than 120 minutes following the onset of symptoms [8]. There is a clear relationship between the onset of therapy and the patient’s transportation to medical facilities. Researchers found that the effectiveness of treatment therapies would improve with a shorter transit time for individuals suffering from AMI. As a result, myocardial ischemia-related death and serious complications will be decreased [9]. According to scientists, patients with AMI-especially those who exhibit hemodynamic instability-who delay receiving emergency medical services (EMS) experience longer times before reperfusion and experience a higher 30-day mortality rate. Nonetheless, in certain cases, the delay results from providing emergency medical care prior to the patient’s hospital transfer, which improves the patient’s prognosis [10].
Apart from the duration of patient transfer, the emergency medical services provided by the ambulance can help lessen the effects of myocardial infarction [11]. Patients frequently travel to medical facilities in a variety of ways, which might impact how quickly they can receive emergency care and treatment while being transported. The research conducted by Pathan et al. evaluated the use of air and ground ambulances for the transportation of patients suffering from AMI in the United States and Qatar between 2012 and 2014. They discovered that while both ambulances offer emergency medical services (EMS) with paramedics who have received training, air ambulances-that is, a specially outfitted helicopter-are better able to adhere to the guidelines for intervention times, which clear blocked arteries and lower the death rate [12]. According to research by individuals with AMI who were transported by EMS to medical centers experienced shorter hospital stays and more successful therapeutic interventions than patients who were not transported by EMS.
To achieve the intended therapeutic goals, emergency medical technicians’ and paramedics’ appropriate patient transportation and primary care are therefore effective. Patients employ a variety of transport options to go to the medical facilities; for instance, some might choose EMS transport, while others may use private or public transportation. However, how individuals with AMI are transported may have an impact on the disease’s outcomes, mortality rate and the disease complications. Therefore, the main objective of the current meta-analysis was to compare the outcomes, survival rates and incidence of complications between STEMI patients transported by EMS vs. non-EMS transportations.
Methods
Literature Search
We looked through online libraries of PUBMED, Google scholar, Web of Science, Science direct and Embase to find publications about pre-hospital STEMI patients EMS transport care. Topic terms in combination with free words were used in the design of the research extraction method. Emergency department; myocardial infarction with ST-segment elevation (STEMI); survival rate; mortality rate; EMS; non-EMS meta-analysis were among the keywords searched. The searchable database has been modified to include papers published between 2008 and 2023, and English papers could be selected throughout the search.
Inclusion Criteria
(1) Cohort study literature available through several sources: (2) An essay about the effectiveness and outlook of prehospital care for STEMI sufferers makes up the investigation’s contents: (3) The EMS group acquired first aid and then transportation under the intervention procedures described in the literature, while the non-EMS were admitted to healthcare centers by other means of transportation.
Exclusion Criteria
(1) Papers with just the title and abstract of the relevant literature or incomplete content; (2) non-cohort research, including news articles, reviews, and case studies; (3) The literature lacks some data, or the primary data-like main outcomes-cannot be included; (4) duplicated papers; (5) Papers written in a language other than English.
Outcome Markers
The article at hand covered eight indicators of outcomes in total: The following outcomes are measured:
Symptom-to-Balloon Time (SBT); (2) Door-To-Balloon Time (DBT); (3) Mortality Rate (MA); (4) Symptom-To-Door Time (STDT); (5) Heart Rate (HR); (6) Systolic Blood Pressure (SBP); (7) Door To-Needle Time (DNT); (8) Symptom-To-Door Time (SNT). 7 papers reported patients’ complications.
Assessment of Literature Quality and Extraction of Data
Two investigators independently examine the abstracts and titles for initial assessment, studied the full text for rescreening, included papers that matched our standards, and gathered the necessary data from the included papers in accordance with the predetermined search formula and exclusion and inclusion criteria. Basic characteristics and outcome indicators were among the data that needed to be gathered; the former mostly contained the patient’s age, the year the research publishing, the sample size, females to males’ ratio, and other details. The latter included the eight outcome indicators’ values. Following the gathering of data and literature, two researchers cross-checked their findings, and a third researcher was asked to mediate any disagreements. The Newcastle-Ottawa scale (NOS) was used to assess the retrospective papers’ quality. The scale consists of eight items, which are pertaining to the choice of study population, comparability, assessment of exposure, or assessment of outcome. Nine points total is the score; low, moderate, and high quality. For prospective studies, the Cochrane collaboration tool was applied.
Statistical Analysis
The data was analysed using Revman Version 5.4 software. The measurement results were described using the standard mean differences (SMD) and 95% CI, and the count results were described using 95% Confidence Interval (CI) and the Risk Ratio (RR) coefficient. For evaluation of data, either random effects models or fixed effects models were employed. I2 represented the test for heterogeneity across many trials. If I2 was greater than 50%, it was deemed that there was heterogeneity among the papers; if I2 was less than 50%, heterogeneity is low and a fixed effect model was applied [13,14]. The literature works’ publication bias was measured using a funnel plot and Egger’s test, and the meta-analysis outcomes’ significance level was assessed using two-sided P<0.05 [15].
Results
Outcomes of A Literature Query
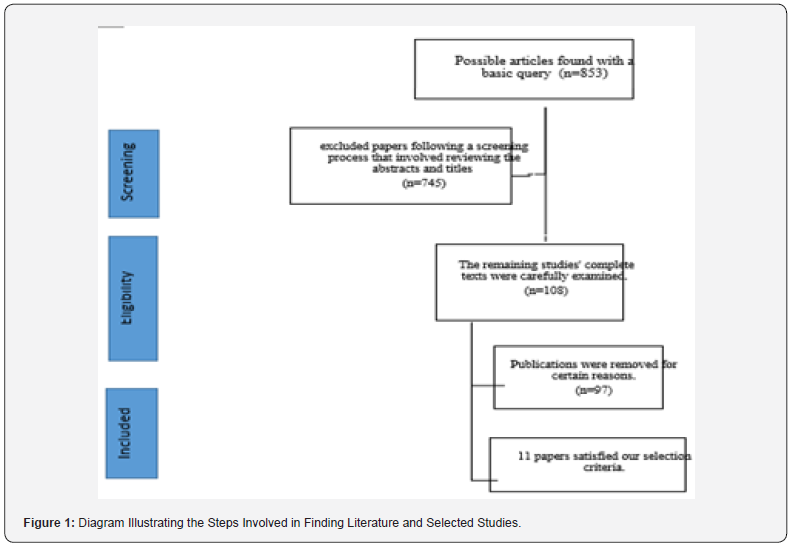
853 publications in all were acquired for the preliminary review; after duplicated papers were eliminated by the software, 108 articles were left. Following a review of the abstract and title, 613 papers that were blatantly at odds with the article’s topic were eliminated, leaving 97 materials that could fit the inclusion criteria. A total of eleven articles were eventually included for full-text viewing after being included in the present article (Figure 1).
Basic Attributes and an Assessment of the Included Literature’s Quality
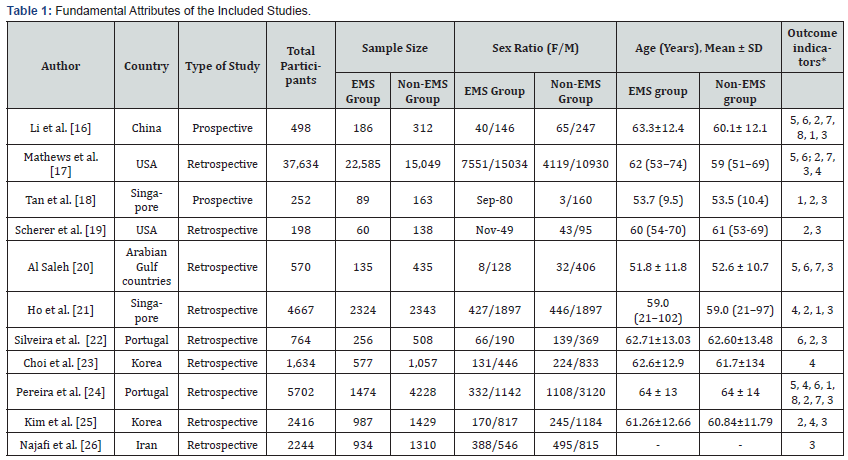
This analysis comprised 11 trials with n=56579 participants (29607 patients in the EMS group and 26972 patients in the non- EMS group). There were 9 retrospective and 2 prospective studies. Among the included articles, 9 papers reported mortality rate, 7 papers reported door to balloon time (DBT), 5 papers reported systolic blood pressure (SBP), 4 papers reported heart rate (HR), 4 papers reported symptoms to balloon time (SBT), 5 papers reported symptoms to door time (STDT), 4 papers reported door to needle time (DNT) and 7 papers reported the incidence of complications among EMS and non-EMS STEMI patients (Table 1), [16-26].
SBT: Symptom-To-Balloon Time
DBT: Door-To-Balloon Time
HR: Heart Rate
SBP: Systolic Blood Pressure
DBP: Diastolic Blood Pressure
DNT: Door To-Needle Time
STDT: Symptom-to-Door Time
SD: Standard Deviation
*Outcome Indicators: SBT [1], DBT [2], Mortality Rate [3], STDT [4], HR [5], SBP [6], DNT [7], SNT [8].
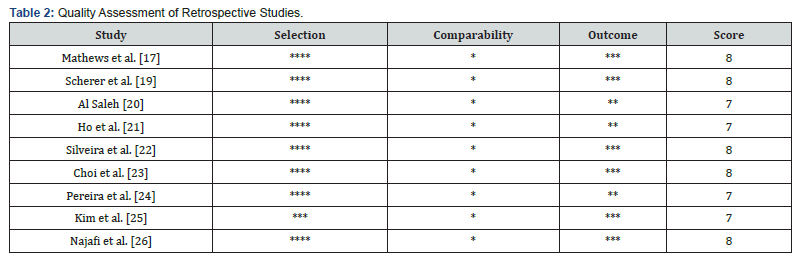
Quality Assessment
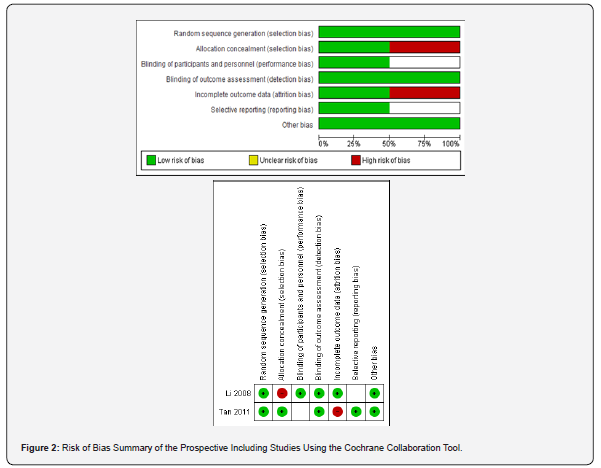
The quality of the prospective studies was assessed according to the risk of bias using the Cochrane collaboration tool. For the retrospective studies, the Newcastle-Ottawa Scale (NOS) was applied, and the assessments are shown respectively (Figure 2) and (Table 2).
Meta Analysis Results
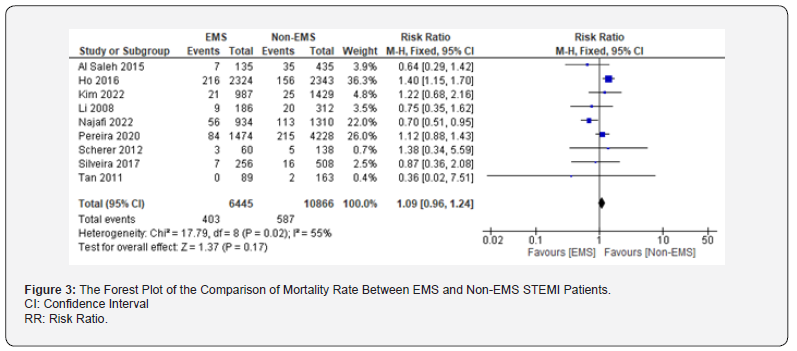
Mortality Rate
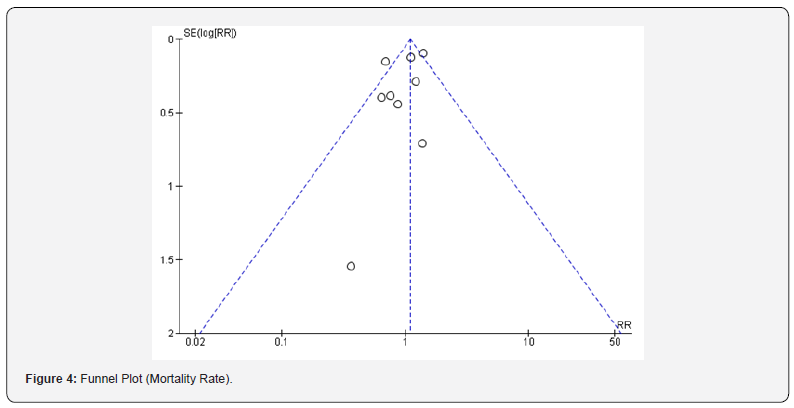
The death rate was reported in nine different articles. The fixed effect model was used to conduct the meta-analysis because there was minimal heterogeneity amongst the studies (I2 = 55%). The results showed that the in-hospital mortality risk ratio among EMS and non-EMS STEMI patients did not significantly differ (p=0.17) (RR =1.09, 95% CI: 0.96 to 1.24; (Figure 3). The overall symmetry was still evident, according to the death rate indicator’s funnel plot analysis (Figure 4). There was no publication bias among the incorporated studies, according to the outcomes of Egger’s test (P>0.05), (Figure 4).
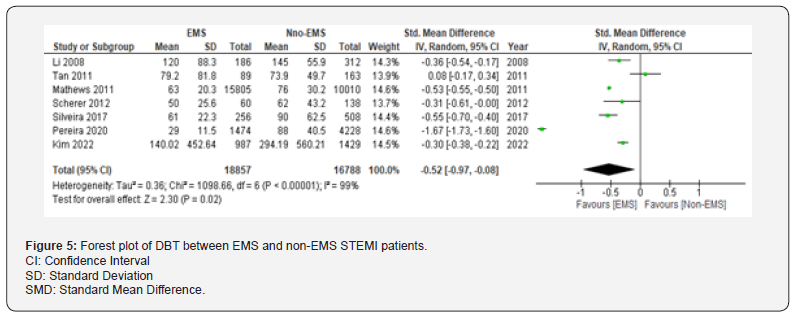
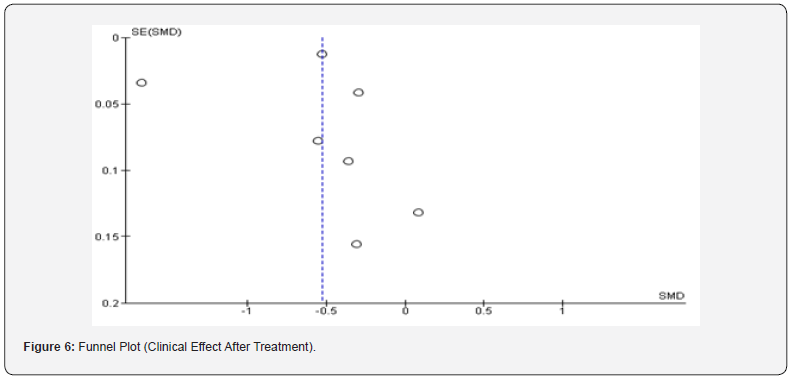
Comparison of Door to Balloon Time (DBT)
Data on participants’ DBT was provided in a total of 7 publications. Because of the high level of heterogeneity (I2 = 99%) among the research studies, a random effect model was used to conduct the meta-analysis. The results showed that the DBT of the patients transferred by EMS was significantly lower than patients transported by other means of transportation (SMD =−0.52, 95% CI: −0.97 to −0.08, P=0.02; (Figure 5). The overall symmetry was still evident, according to the funnel plot evaluation of DBT (Figure 6). The included articles did not exhibit publication bias, according to the outcomes of Egger’s test (P>0.05) (Figure 6).
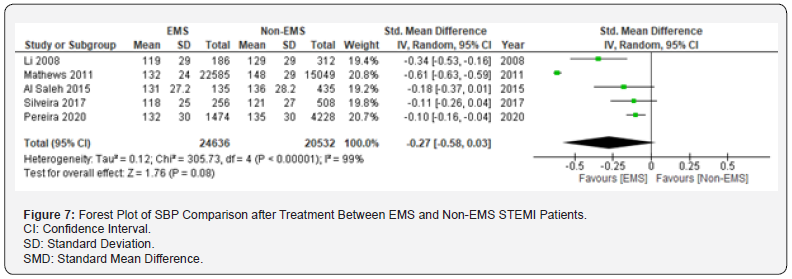
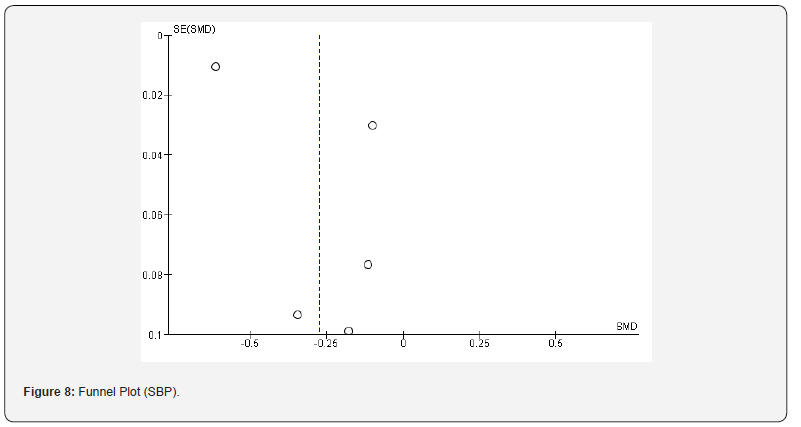
Comparison of SBP After Treatment
A total of 5 papers reported data on patients’ SBP after treatment. There was high heterogeneity among the studies (I2 =99%), so the meta-analysis was carried out using the random effect model. The results showed that the SBP of the patients was lower among EMS patients than patients transported by non-EMS means (SMD =−0.27, 95% CI: −0.58 to −0.03, P=0.08; (Figure 7). The overall symmetry was still evident, according to the funnel plot evaluation of the SBP (Figure 8). The included articles did not exhibit publication bias, according to the outcomes of Egger’s test (P>0.05), (Figure 8).
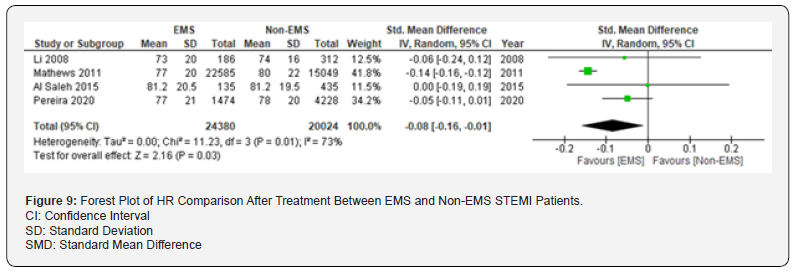
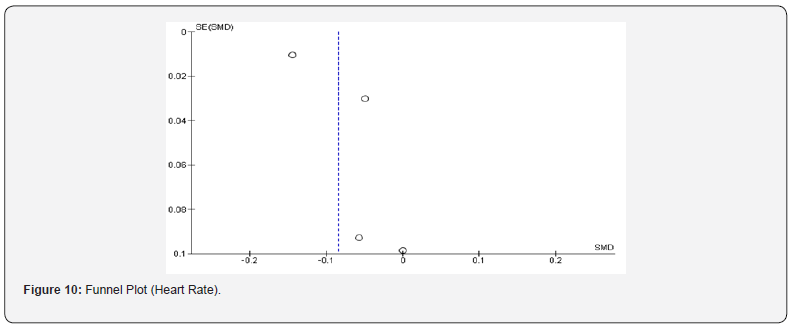
Comparison of Heart Rate After Treatment
A total of 4 papers reported data on heart rate of patients after treatment. There was a high heterogeneity among the studies (I2 =73%), so the meta-analysis was carried out by the random effect model. The results showed that the HR of the patients was significantly reduced among EMS transported patients than non-EMS transported patients (SMD =−0.08, 95% CI: −0.16 to −0.01, P=0.03; (Figure 9). The overall symmetry was still evident, according to the funnel plot evaluation of the HR (Figure 10). The included articles did not exhibit publication bias, according to the outcomes of Egger’s test (P>0.05), (Figure 10).
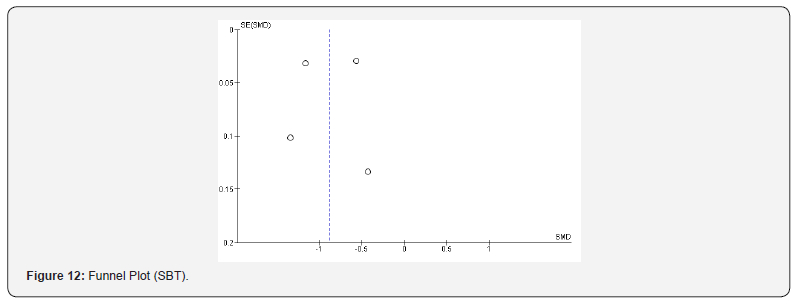
Comparison of Symptoms to Balloon Time (SBT)
A total of 4 papers reported data on symptoms to balloon time of EMS and non-EMS STEMI patients. There was high heterogeneity among the studies (I2 =99%), so the meta-analysis was carried out by the random effect model. The results showed that the SBT was significantly lower among EMS transported patients than non-EMS patients (SMD =−0.87, 95% CI: −1.29 to −0.46, P<0.001; (Figure 11). The overall symmetry was still evident, according to the funnel plot evaluation of SBT (Figure 12). The included articles did not exhibit publication bias, according to the outcomes of Egger’s test (P>0.05), (Figure 12).
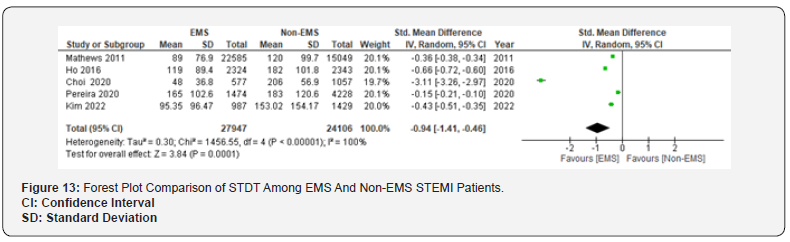
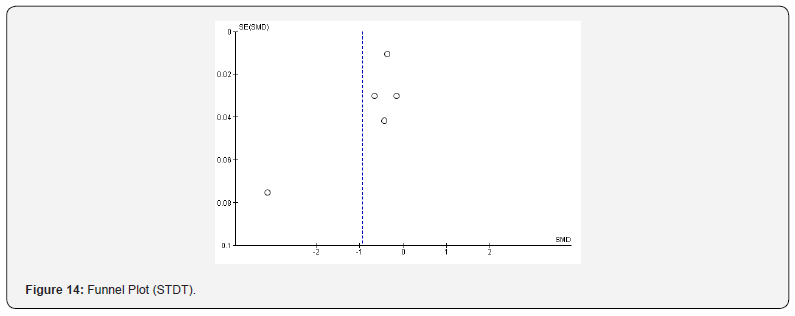
Comparison of Symptoms to Door Time (STDT) Among EMS and Non-EMS STEMI Patients
A total of 5 papers reported data on STDT. There was a high heterogeneity among the studies (I2 =100%), so the meta-analysis was carried out by the random effect model. The results showed that STDT of the EMS transported patient significantly reduced than non-EMS patients (SMD =-0.94, 95% CI: -1.41 to -0.46, P< 0.001; (Figure 13). The overall symmetry was still evident, according to the funnel plot evaluation of STDT (Figure 14). The included articles did not exhibit publication bias, according to the outcomes of Egger’s test (P>0.05), (Figure 14).
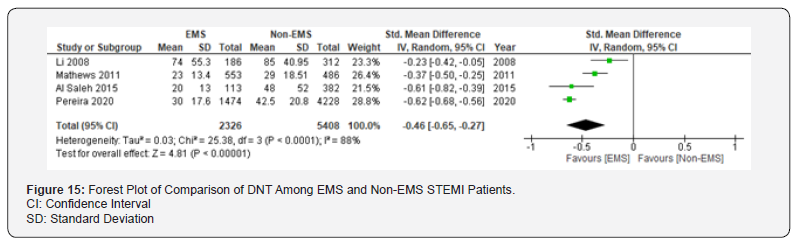
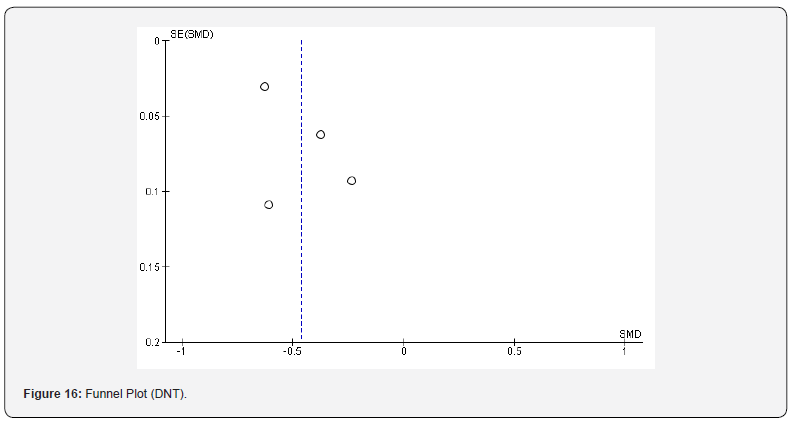
Comparison of Door to Needle Time (DNT) Among EMS and Non-EMS STEMI Patients
A total of 4 papers reported data on DNT. There was a high heterogeneity among the studies (I2 =88%), so the meta-analysis was carried out by the random effect model. The results showed that DNT of the EMS transported patient was significantly lower than non-EMS patients (SMD =-0.46, 95% CI: -0.65 to -0.27, P< 0.001; (Figure 15). The overall symmetry was still evident, according to the funnel plot evaluation of DNT (Figure 16). The included articles did not exhibit publication bias, according to the outcomes of Egger’s test (P>0.05), (Figure 16).
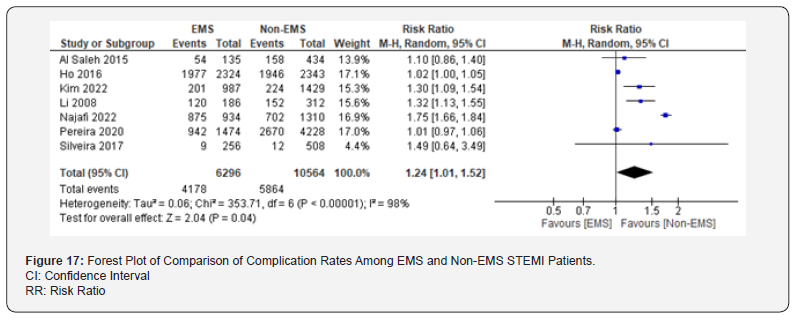
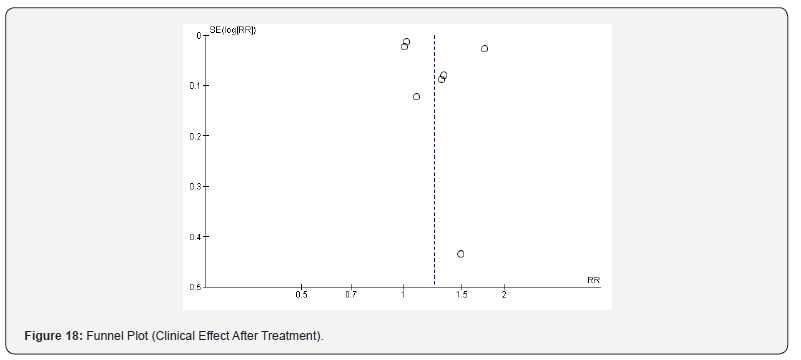
Comparison of Incidence of Complications After Treatment
A total of 7 papers reported data on the incidence of complications in patients transported by EMS and those non-EMS transported patients. There was a high heterogeneity among the studies (I2 =98%), therefore the meta-analysis was performed using the random effect model. The results showed that the incidence of complications after treatment among non-EMS patients was significantly higher than those patients transported by EMS means (RR =1.24, 95% CI: 1.01 to 1.52, P=0.04 (Figure 17). The overall symmetry was still evident, according to the funnel plot evaluation of complications rate (Figure 18). The included articles did not exhibit publication bias, according to the outcomes of Egger’s test (P>0.05), (Figure 18).
Discussion
Early medical interventions and prompt detection of myocardial infarction are critical in mitigating mortality, complications, and disability in patients [27-31]. Patients with acute AMI have unexpected conditions, and they could experience a deadly dysrhythmia at any time [32,33]. Thus, prompt clinical procedures performed by emergency care professionals are crucial in lowering the disease’s death and morbidity rates [34]. Alrawashdeh et al. [35] carried out research in Australia and Canada in which they demonstrated that EMS-transported AMI patients had superior outcomes from primary percutaneous coronary intervention (PPCI) and a decreased rate of cardiac arrest outside of the medical facility. According to Varcoe et al. [36], individuals with AMI who were transported to the hospital by EMS within the first few minutes of their condition experienced good treatment outcomes. Additionally, Rodríguez-Leor et al. [37] demonstrated that the death rate in the ambulance and hospital was reduced for patients with AMI who received appropriate primary medical treatment and utilized efficient EMS transportation to the hospital.
Additionally, this study demonstrated that EMS-transported AMI patients had better outcomes from PPCI than did non- EMS-transported patients. Clinical recommendations state that improved treatment outcomes occur when patients receive interventional treatments more quickly, such as PPCI for AMI patients, and when they are transported to the hospital by EMS more quickly [38]. 1244 individuals in this study who suffered from AMI (55.43%) were transported to the hospital by non-EMS means. Furthermore, 113 (5.03%) of the 169 patients who died from AMI (7.26%) did not employ emergency medical services to go to the hospital. 52 patients utilising EMS transport had successful cardiopulmonary resuscitations (CPRs) performed on them. Ventricular fibrillation also resulted in an effective DC shock for 27 patients. The findings demonstrated that individuals with AMI who employed EMS transport had a reduced death rate than those who did not. Therefore, it is essential to undertake culture-building events to raise awareness among the general population about the need for emergency medical services (EMS) to transport patients, especially those who have had a myocardial infarction.
In this context, Ghasemi et al. [39] demonstrated that EMS technicians’ performance of cardiopulmonary resuscitation is one of the most important variables reducing the death rate in patients with AMI. They demonstrated how the rate of death is increased when patients’ relatives do not know how to handle patients experiencing AMI and cardiac arrest and do not use pre-hospital emergency services in these situations. The results of this research are in line with the outcomes of Schultz et al. study [40], which demonstrated the elevated survival rates for individuals with STEMI complicated by OHCA and the critical role EMS plays in giving prompt CPR and defibrillation. Primary medical procedures, such as patient immobilization, managing pain, oxygen utilization, and the use of antiplatelet and anticoagulation medications like aspirin, are crucial in avoiding and minimizing complications in patients suffering from AMI, according to medical recommendations and management protocols [41].
As a result, EMS will be helpful and effective in reaching the stated therapy objectives. Assume that both patients and their partners transport their patients to the medical centers by non- EMS means. The patient’s treatment outcomes will be affected if they are unable to receive primary care from emergency medical technicians. Since cardiac dysrhythmias, particularly ventricular fibrillation (VF), are the most common cause of death for patients with AMI in the first few minutes and hours after the event, the likelihood that these patients will die will rise if they employ non-EMS transport [42]. According to current meta-analysis, the mean time from the start of symptoms to hospital arrival was significantly lower among STEMI EMS-transported patients than non-EMS transported STEMI patients. However, non-EMS patients may experience cardiac arrest during transportation because their relatives lack the required clinical skills and knowledge to take appropriate action, endangering the patient’s life.
It should be pointed out that emergency medical professionals and paramedics execute the essential primary medical and therapeutic measures as well as, in certain instances, cardiopulmonary resuscitation, which may increase the survival time. This article demonstrates how EMS transportation can greatly enhance sufferers’ clinical results by lowering mortality rate, SBP, heart rate, DBT, SBT, STDT, DNT and incidence of after-treatment complications. Reperfusion treatment is of the utmost importance because those suffering from AMI may have myocardial cells that are not sufficiently contractile and lose functionality as a result of ischemia. Time dependency is considerable with this form of therapy [43]. The patient’s prognosis improves with a shorter reperfusion period during therapy. Consequently, restoring myocardial perfusion ought to constitute the priority for patients requiring pre-hospital emergency therapy if they have a possibility of experiencing AMI [44]. Once the patient no longer has symptoms related to their heart rate, breathing, or blood pressure, they can be moved to a licensed hospital for all-encompassing care that will enhance their clinical outcome and prognosis.
Limitations
There are a few other restrictions and issues with the study. First off, despite our best efforts to locate papers and track down sources for this article, there might still be omissions due to lack of some essential outcomes.
Conclusions
In conclusion, those suffering from STEMI can benefit clinically from the EMS pre-hospital first aid transport. This approach may successfully avoid the patients from getting worse, lower the risk of complications, and decrease the time it takes for patients to receive comprehensive medical care. This article demonstrates how EMS transportation can greatly enhance sufferers’ clinical results by lowering mortality rate, SBP, HR, DBT, SBT, STDT, DNT and incidence of after-treatment complications. Additional high-quality randomised controlled trials are required to confirm this result.
Acknowledgment
The author would like to express his gratitude to Dar Al Uloom University, Riyadh. KSA
References
- Lim SC, A Rahman, NM Yaacob (2019) Pre-hospital factors influencing time of arrival at emergency departments for patients with acute ST-elevation myocardial infarction. The Malaysian journal of medical sciences: MJMS 26(1): 87-98.
- Fowler RL, Taylor Sanders, Rachel Nguyen, Reagan Rosenberger, Jeffrey Metzger (2021) The impact of mode of presentation to the ED on time metrics for STEMI patients. JEMS, Pakistan.
- Pendyal A, Rothenberg C, Scofi JE, Krumholz HM, Safdar B et al. (2020) National trends in emergency department care processes for acute myocardial infarction in the United States, 2005 to 2015. Journal of the American Heart Association 9(20): e017208.
- Jollis JG, Al Khalidi HR, Roettig ML, Berger PB, Corbett CC et al. (2018) Impact of regionalization of ST-segment–elevation myocardial infarction care on treatment times and outcomes for emergency medical services-transported patients presenting to hospitals with percutaneous coronary intervention: Mission: Lifeline Accelerator-2. Circulation 137(4): 376-387.
- Feng L, Li M, Xie W, Zhang A, Lei L, et al. (2019) Prehospital and in-hospital delays to care and associated factors in patients with STEMI: an observational study in 101 non-PCI hospitals in China. BMJ Open 9(11): e031918.
- Kontos MC, Gunderson MR, Zegre-Hemsey JK, Lange DC, French WJ, et al. (2020) Prehospital Activation of Hospital Resources (PreAct) ST‐Segment–Elevation Myocardial Infarction (STEMI): A Standardized Approach to Prehospital Activation and Direct to the Catheterization Laboratory for STEMI Recommendations from the American Heart Association's Mission: Lifeline Program. Journal of the American Heart Association 9(2): e011963.
- Balk M, Gomes HB, De Quadros AS, Saffi MA, Leiria TL (2019) Comparative analysis between transferred and self-referred STEMI patients undergoing primary angioplasty. Arquivos Brasileiros de Cardiologia 112(4): 402-407.
- Hsiao YT, Hung JF, Zhang SQ, Yeh YN, Tsai MJ, et al. (2023) The Impact of Emergency Department Arrival Time on Door-to-Balloon Time in Patients with ST-Segment Elevation Myocardial Infarction Receiving Primary Percutaneous Coronary Intervention. Journal of Clinical Medicine 12(6): 2392.
- Yiadom M, W Gong, S Bloos, D Liu (2022) 287 influences of time to diagnosis on time to percutaneous coronary intervention for emergency department ST elevation myocardial infarction (STEMI) patients: door to ECG matters. Annals of Emergency Medicine 80(4): S125.
- Trabattoni D, Montorsi P, L Merlino (2020) Late STEMI and NSTEMI patients’ emergency calling in COVID-19 outbreak. Canadian Journal of Cardiology 36(7): 1161. e7-1161. e8.
- Scholz KH, Friede T, Meyer T, Jacobshagen C, Lengenfelder B, et al. (2020) Prognostic significance of emergency department bypass in stable and unstable patients with ST-segment elevation myocardial infarction. European Heart Journal: Acute Cardiovascular Care 9(1_suppl): 34-44.
- Pathan SA, Jason Soulek, Isma Qureshi, Howard W, Andrew P Reimer, et al. (2017) Helicopter EMS and rapid transport for ST-elevation myocardial infarction: The Hearts study. Journal of Emergency Medicine, Trauma and Acute Care 2017(1).
- Melsen WG, Bootsma MC, Rovers MM, Bonten MJ (2014) The effects of clinical and statistical heterogeneity on the predictive values of results from meta-analyses. Clinical microbiology and infection, 2014. 20(2): 123-129.
- Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414): 557-560.
- Lin L, H Chu (2018) Quantifying publication bias in meta‐analysis. Biometrics 74(3): 785-794.
- Li S, Hu DY, Yan HB, Yang JG, Sun YH, et al. (2008) Influence of ambulance use on early reperfusion therapies for acute myocardial infarction. Chinese medical journal 121(9): 771-775.
- Mathews R, Peterson ED, Li S, Roe MT, Glickman SW, et al. (2011) Use of emergency medical service transport among patients with ST-segment–elevation myocardial infarction: findings from the national cardiovascular data registry acute coronary treatment intervention outcomes network registry–get with the guidelines. Circulation 124(2): 154-163.
- Tan LL, Wong HB, Poh CL, Chan MY, Seow SC, et al. (2011) Utilisation of emergency medical service among Singapore patients presenting with ST‐segment elevation myocardial infarction: prevalence and impact on ischaemic time. Internal Medicine Journal 41(12): 809-814.
- Scherer TM, Russ S, Jenkins CA, Jones ID, Slovis CM, et al. (2012) Predictors of ambulance transport in patients with ST-elevation myocardial infarction. Prehospital and disaster medicine 27(3): 226-230.
- Al Saleh A (2015) Feasibility of Developing Emergency Medical Services (EMS) Registry and Exploring the benefits of using EMS among Arabian Gulf patients presenting with ST elevation myocardial infarction (STEMI). Data analysis and interpretation thesis of the RACE III registry (Gulf Registry of Acute Coronary Events: Primary PCI programs). Open Access Dissertations and Theses.
- Ho AF, Loy EY, Pek PP, Wah W, Tan TX, et al. (2016) Emergency medical services utilization among patients with ST-segment elevation myocardial infarction: Observations from the Singapore myocardial infarction registry. Prehospital Emergency Care 20(4): 454-461.
- Silveira I, Sousa MJ, Rodrigues P, Brochado B, B Santos R, et al. (2017) Developments in pre-hospital patient transport in ST-elevation myocardial infarction. Revista Portuguesa de Cardiologia 36(11): 847-855.
- Choi H, Cha WC, Jo IJ, Choi JH, Sim MS, et al. (2020) The individual and neighborhood factors associated with the use of emergency medical services in patients with ST-elevation myocardial infarction. Clinical and Experimental Emergency Medicine 7(4): 302-309.
- Pereira JG, Abreu L, Antunes H, Gonçalves ML, Marmelo B, et al. (2020) Impact of Emergency Medical System Transportation in ST-segment Elevation Myocardial Infarction: A Nationwide Retrospective Study. Acta Médica Portuguesa 33(6): 390-400.
- Kim YR, Jeong MH, An MJ, Han X, Cho KH, et al. (2022) Comparison of Prognosis According to the Use of Emergency Medical Services in Patients with ST-Segment Elevation Myocardial Infarction. Yonsei Medical Journal 63(2): 124-132.
- Najafi H, Bahramali E, Bijani M, Dehghan A, Amirkhani M, et al. (2022) Comparison of the outcomes of EMS vs. Non-EMS transport of patients with ST-segment elevation myocardial infarction (STEMI) in Southern Iran: a population-based study. BMC emergency medicine 22(1): 46.
- Masiewicz S, Gutovitz S, Hart L, Leaman SM, Jehle D, et al. (2020) Presentation times of myocardial infarctions to the emergency department: disappearance of the morning predominance. JEM 58(5): 741-748.
- Redwood E, Hyun K, French JK, Kritharides L, Ryan M, et al. (2021) The influence of travelling to hospital by ambulance on reperfusion time and outcomes for patients with STEMI. The Medical Journal of Australia 214(8): 377-378.
- Frisch SO, Faramand Z, Li H, Abu-Jaradeh O, Martin-Gill C, et al. (2019) Prevalence and predictors of delay in seeking emergency care in patients who call 9-1-1 for chest pain. The Journal of emergency medicine 57(5): 603-610.
- Su HY, Tsai JL, Hsu YC, Lee KH, Chang CS, et al. (2021) A modified cardiac triage strategy reduces door to ECG time in patients with ST elevation myocardial infarction. Sci Rep 11(1): 6358.
- Alrawashdeh A, Nehme Z, Williams B, Stub D (2020) Emergency medical service delays in ST-elevation myocardial infarction: a meta-analysis. Heart 106(5): 365-373.
- Trimmel H, Bayer T, Schreiber W, Voelckel WG, Fiedler L, et al. (2018) Emergency management of patients with ST-segment elevation myocardial infarction in Eastern Austria: a descriptive quality control study. Scand J Trauma Resusc Emerg Med 26: 1-8.
- Maliszewski B, Whalen M, Lindauer C, Williams K, Gardner H, et al. (2020) Quality improvement in the emergency department: a project to reduce door-to-electrocardiography times for patients presenting with chest pain. J Emerg Nurs 46(4): 497-504. e2.
- Anno AD, Martone A, Natale E, Rizzon B, et al. (2020) Prehospital ECG transmission results in shorter door-to-wire time for STEMI patients in a remote mountainous region. The American Journal of Emergency Medicine 38(2): 252-257.
- Nehme Z, Williams B, Smith K, Brennan A, et al. (2021) Impact of emergency medical service delays on time to reperfusion and mortality in STEMI. Open Heart 8(1): e001654.
- Varcoe RW, Clayton TC, Gray HH, de Belder MA, Ludman PF, et al. (2017) Impact of call-to-balloon time on 30-day mortality in contemporary practice. Heart 103(2): 117-124.
- Fernández-Nofrerías E, Mauri F, Salvatella N, Carrillo X, et al. (2011) Analysis of reperfusion delay in patients with acute myocardial infarction treated with primary angioplasty based on first medical contact and time of presentation. Rev Esp Cardiol 64(6): 476-483.
- Solhpour A, Won Chang K, Arain SA, Balan P, Loghin C, et al. (2016) Ischemic time is a better predictor than door‐to‐balloon time for mortality and infarct size in ST‐elevation myocardial infarction. Catheter Cardiovasc Interv 87(7): 1194-1200.
- Ghasemi A, Nasrabad RR, Mokhlesabadifarahani T, Alizadeh Z, Beygi N, et al. (2021) Exploring the challenges affecting the quality of cardiopulmonary resuscitation from the perspective of Emergency Medical Service personnel: a qualitative study. AVFT 40(2): 154-163.
- Doan TN, Bosley E, Rogers B, Rashford S, et al. (2021) Prehospital study of survival outcomes from out-of-hospital cardiac arrest in ST-elevation myocardial infarction in Queensland, Australia (the PRAISE study). European Heart Journal Acute Cardiovascular Care 10(6): 616-623.
- Mesas CE, Mesas CE, Rodrigues RJ, Mesas AE, Feijó VBR, et al. (2018) Symptoms awareness, emergency medical service utilization and hospital transfer delay in myocardial infarction. BMC Health Serv Res 18(1): 490.
- Baldi E, Camporotondo R, Gnocchi M, Otero R, Guida S, et al. (2022) Barriers associated with emergency medical service activation in patients with ST-segment elevation acute coronary syndromes. Intern Emerg Med 17(4): 1165-1174.
- McLaren JT, Taher A, Kapoor M, L Yi S, Chartier LB, et al. (2021) Sharing and Teaching Electrocardiograms to Minimize Infarction (STEMI): reducing diagnostic time for acute coronary occlusion in the emergency department. Am J Emerg Med 48: 18-32.
- Zameer I, Baig A, Ahmed Z, Qayyum J, Amir A, et al. (2022) Factors leading to delayed presentation among patients presenting with ST-elevation Myocardial Infarction in Emergency Department of a tertiary care hospital. Pakistan Biomedical Journal 5(1).






























